Withdrawal from drug addiction is a complex process with varying symptoms. Opioids, benzodiazepines, and alcohol can lead to challenging physical and psychological experiences. Understanding the neuroscience of withdrawal is essential. Managing symptoms involves medical interventions, support, and behavioral strategies. This exploration delves into withdrawal intricacies, substance-specific challenges, and methods for navigating this critical phase in recovery.
Toughest drug for withdrawal symptoms.
The severity of withdrawal symptoms can vary widely depending on the individual and the substance involved. However, some drugs are commonly associated with particularly challenging withdrawal experiences. Opioids, including heroin and prescription painkillers, are often considered among the toughest to quit due to intense physical and psychological withdrawal symptoms. Benzodiazepines, which are commonly prescribed for anxiety and sleep disorders, can also result in severe withdrawal symptoms, including seizures, making them challenging to quit without proper medical supervision. It’s important to note that seeking professional help and guidance is crucial when attempting to stop any substance with potentially problematic withdrawal symptoms.
Neuroscience of drug withdrawals.
Withdrawal from drugs involves complex neurobiological processes that result from the brain’s attempt to adapt to the presence of the substance and then readapt when the substance is removed. Different drugs affect various neurotransmitter systems, leading to diverse withdrawal symptoms. Here is a general overview of the neuroscience of withdrawal:
- Neurotransmitter Imbalance:
- Chronic drug use can disrupt the balance of neurotransmitters, the chemical messengers in the brain.
- Withdrawal occurs when the drug is removed, causing an imbalance in neurotransmitter levels.
- Dopamine Dysregulation:
- Many drugs, including opioids and stimulants, affect the dopamine system, leading to heightened levels during drug use.
- Withdrawal may involve a drop in dopamine levels, contributing to symptoms like depression, fatigue, and anhedonia.
- GABA and Glutamate Interaction:
- Benzodiazepines and alcohol affect the GABAergic system, leading to increased inhibitory signals in the brain.
- Withdrawal involves a rebound effect, with excessive excitability due to reduced inhibitory input.
- Opioid Receptor Adaptation:
- Opioids bind to specific receptors in the brain, and chronic use leads to receptor adaptations.
- Withdrawal symptoms, such as pain, anxiety, and gastrointestinal issues, result from the absence of the drug binding to these receptors.
- Serotonin Changes:
- Drugs like MDMA and certain antidepressants affect serotonin levels.
- Withdrawal may involve mood disturbances, sleep problems, and changes in appetite due to alterations in serotonin transmission.
- Endocannabinoid System:
- Cannabis affects the endocannabinoid system, which plays a role in mood, appetite, and sleep.
- Withdrawal may lead to mood changes, sleep disturbances, and irritability.
- NMDA Receptor Involvement:
- Alcohol and some hallucinogens impact the NMDA receptors.
- Withdrawal symptoms, including seizures and cognitive disturbances, may be related to NMDA receptor hyperactivity during withdrawal.
- Neuroadaptive Changes:
- The brain undergoes neuroadaptive changes during chronic drug use, and withdrawal reflects the attempt to return to a state of equilibrium.
Understanding the neuroscience of withdrawal is crucial for developing effective treatments and interventions to support individuals going through the challenging process of drug withdrawal.
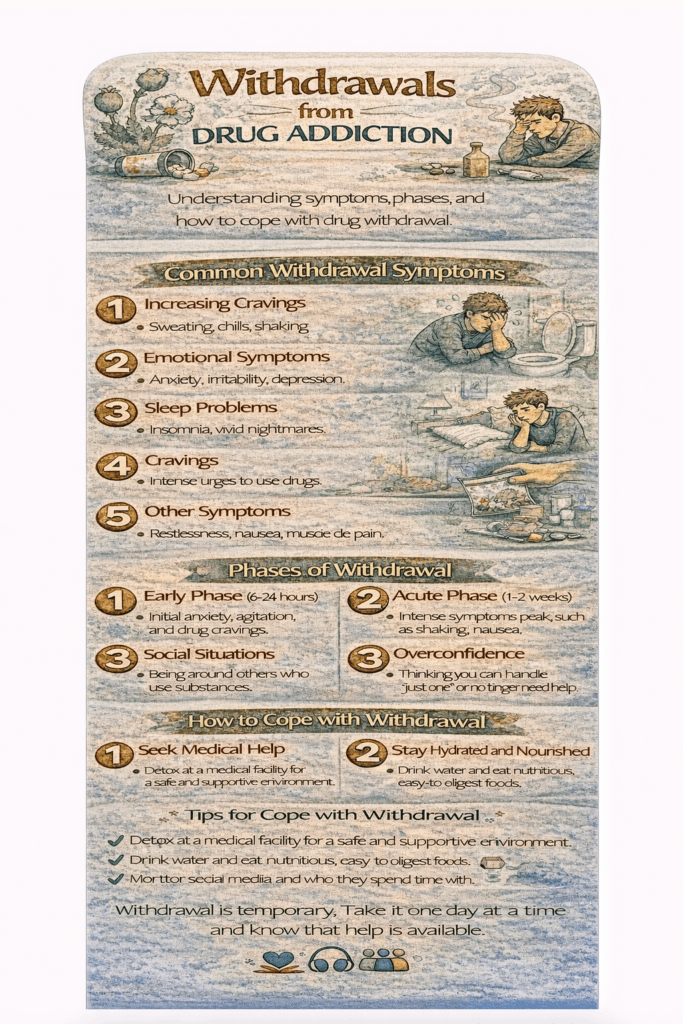
Drug withdrawal symptoms.
Withdrawal symptoms from drugs can vary widely depending on the type of substance, the duration and intensity of use, and individual factors. Here are typical withdrawal symptoms associated with some specific classes of drugs:
- Opioids (e.g., heroin, oxycodone):
- Flu-like symptoms (nausea, vomiting, diarrhea)
- Muscle aches and pains
- Insomnia
- Anxiety
- Sweating and chills
- Runny nose and teary eyes
- Yawning
- Dilated pupils
- Benzodiazepines (e.g., Xanax, Valium):
- Anxiety
- Insomnia
- Irritability
- Tremors
- Sweating
- Difficulty concentrating
- Elevated heart rate
- Muscle stiffness
- Alcohol:
- Tremors (shakes)
- Anxiety
- Nausea and vomiting
- Headache
- Sweating
- Insomnia
- Hallucinations (in severe cases)
- Seizures (in severe cases)
- Stimulants (e.g., cocaine, methamphetamine):
- Fatigue
- Increased appetite
- Disturbed sleep patterns
- Depression
- Increased dreaming
- Slowed activity and movement
- Nicotine:
- Irritability
- Anxiety
- Difficulty concentrating
- Increased appetite
- Depression
- Insomnia
- Cannabis:
- Irritability
- Insomnia
- Loss of appetite
- Anxiety
- Restlessness
It’s important to note that the severity and duration of withdrawal symptoms can vary from person to person. Some individuals may experience more intense symptoms, especially if they have a history of heavy or prolonged substance use. In severe cases, withdrawal from certain substances can be life-threatening, underscoring the importance of seeking professional medical help.
The process of withdrawal is a challenging aspect of addiction recovery, and individuals are encouraged to seek support from healthcare professionals, addiction specialists, or support groups during this period.
Management of withdrawal symptoms.
Managing withdrawal symptoms often involves a combination of pharmacological and behavioral modalities. Here are some modalities commonly used to manage withdrawal symptoms better:
- Medication-Assisted Treatment (MAT):
- Opioid Agonists (e.g., Methadone, Buprenorphine): These medications activate opioid receptors, helping to manage cravings and reduce withdrawal symptoms in individuals with opioid use disorder.
- Benzodiazepines: For alcohol and benzodiazepine withdrawal, medications like diazepam or chlordiazepoxide may be used to taper off the substance gradually.
- Symptom-Specific Medications:
- Non-Opioid Analgesics: Over-the-counter pain relievers, such as acetaminophen or ibuprofen, may help manage pain during withdrawal.
- Antiemetics: Medications to control nausea and vomiting, which are typical withdrawal symptoms.
- Medical Monitoring:
- Inpatient Detoxification: For severe withdrawal, especially with alcohol or benzodiazepines, inpatient detoxification programs provide close medical monitoring and support.
- Outpatient Monitoring: Regular medical check-ins and monitoring can be effective for less severe cases.
- Psychosocial Support:
- Counseling and Therapy: Cognitive-behavioral therapy (CBT), motivational enhancement therapy (MET), and contingency management are examples of therapeutic approaches that can address psychological aspects of withdrawal.
- Support Groups: Participating in support groups, such as 12-step programs like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), provides peer support and a sense of community.
- Nutritional Support:
- Proper nutrition is essential during withdrawal to address deficiencies and promote overall health.
- Holistic Approaches:
- Mindfulness and Meditation: Practices that promote mindfulness and relaxation can help individuals cope with stress and anxiety during withdrawal.
- Acupuncture and Massage: Some individuals find relief from withdrawal symptoms through alternative therapies like acupuncture or massage.
- Physical Exercise:
- Regular physical activity can help regulate mood, improve sleep, and alleviate some withdrawal symptoms.
- Gradual Tapering:
- Gradual reduction of the substance under medical supervision can minimize the severity of withdrawal symptoms.
- Pharmacogenetic Testing:
- Genetic testing to determine an individual’s response to specific medications can guide the selection of appropriate medications for withdrawal management.
It’s important to note that the choice of modalities depends on the specific substance, the severity of withdrawal, and individual factors. A comprehensive and individualized approach that addresses both the physical and psychological aspects of withdrawal is typically most effective.
Conclusion
Navigating the challenges of drug withdrawal demands a comprehensive understanding of the associated symptoms and the unique difficulties posed by certain substances. From the intense withdrawals of opioids to the complexities of benzodiazepine discontinuation, the neuroscience behind withdrawal sheds light on the intricate processes at play. Fortunately, various modalities, including medical interventions and holistic approaches, can significantly alleviate the hardships of withdrawal. Acknowledging the severity of withdrawal symptoms underscores the importance of tailored strategies and compassionate support to enhance the journey toward recovery.
Video: