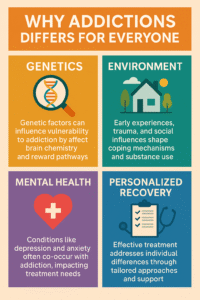
Addiction is a complicated topic, and it’s something I’ve seen affect people from all walks of life. There’s often a question that comes up: why does addiction seem to get its hooks into some people more deeply than others? I’m checking out some of the main reasons, spanning biology, environment, mental health, and personal experience, that explain why this struggle looks so different from one person to the next.
What Makes Addiction So Complex?
Addiction goes way beyond just willpower. There’s a whole mix of factors that can turn casual use into dependency for some people, while others remain pretty unaffected. Over the years, scientists and health professionals have found that addiction touches on genetics, brain differences, life experiences, access to substances, and even how someone copes with stress.
According to research from the National Institute on Drug Abuse, close to half of a person’s likelihood to develop an addiction comes from their genes. But genes are just one piece. Traumatic experiences, stress, mental health issues, and social surroundings all add up. The bottom line is there’s no one-size-fits-all reason why addiction happens more easily for some.
Why Do Some People Get Addicted More Easily?
I’ve noticed that while some people can drink occasionally or try substances without trouble, others quickly slide into patterns they can’t control. Science backs this up; a distinct mix of risk factors turns the tide for each individual.
- Genetics: Family history often plays a significant role. Having close relatives with addiction tends to increase risk.
- Brain Chemistry: Some brains are wired in a way that makes substances feel more rewarding, making it challenging to stop once started.
- Early Life Stress or Trauma: Growing up under a lot of stress or facing traumatic events can make addiction more likely later on.
- Environment: Being surrounded by substance use or having easy access can make resisting a lot more challenging.
- Mental Health: Anxiety, depression, or other mental health conditions often make people more vulnerable to addiction.
Breakdown: Key Reasons Addiction Hits Some People Harder
Each person’s struggle with addiction has its own story, but here’s how some main factors come together and interact.
Genetics and Family History
Genetics has a pretty strong say in the likelihood of developing an addiction. If you’ve got a parent or sibling who struggled with addiction, your risk can go up; it’s not guaranteed, but the numbers tilt that way. Studies suggest that genes related to dopamine (the brain’s “reward chemical”) can make specific individuals more sensitive to the effects of drugs or alcohol, or less able to control cravings.
Brain Differences
Brains are diverse. Minor structural or chemical differences can change how we respond to rewards and pleasure. In some people, the “reward system” releases stronger rushes when exposed to substances. This makes it feel even more rewarding and can cause cravings that are hard to ignore. Sometimes people with less responsive reward systems turn to substances to feel ‘normal’ or to perk up their mood.
Early Life Experiences and Trauma
Rough childhoods, neglect, or trauma are commonly linked with a greater risk for addiction. For someone growing up in a chaotic home or facing early adversity, turning to substances can be a way to cope or escape. The Adverse Childhood Experiences (ACE) study found that the more tough experiences you have as a kid, the higher your odds are for using drugs, drinking heavily, or developing other health challenges as an adult.
Environment and Social Circles
Where you live, who you hang out with, and even how much free time you have can all factor in. Some areas have more drugs or alcohol available, or cultures that normalize heavy use. Sometimes, it’s about wanting to fit in, while other times it’s simply having easier access. If people around you use or encourage it regularly, resisting gets harder.
Mental Health Connections
Having conditions like depression, anxiety, PTSD, or ADHD makes people more prone to addiction. Using substances can seem like a shortcut to feeling better, even though it often causes more trouble long-term. According to NIMH research, about half of those dealing with addiction also face other mental health challenges. Treating both together offers better chances for recovery.
How Personal Coping Styles and Stress Fit In
I’ve learned that how someone manages stress and emotions can play a big part in how addiction develops. Some naturally turn inward, maybe choosing meditation, hobbies, or exercise. Others might reach for a drink, cigarettes, or something more substantial to take the edge off. If someone hasn’t picked up healthy ways to cope, substances can start to feel like the only relief.
- Healthy Outlets: Sports, art, talking with friends, mindfulness practices, and routines help reduce risk.
- Risky Outlets: Using substances for relief or to numb emotions can send a person down the path toward addiction faster, especially when life gets stressful.
Common Challenges for Those at Higher Risk
People facing higher risk aren’t always aware until things get tough. Here are a few hurdles that pop up often for folks more vulnerable to addiction:
- Denial and Stigma: Not wanting to admit a problem or feeling ashamed to ask for help sometimes prevents people from seeking support.
- Lack of Support: Not everyone has friends or family who understand or can help find their way through challenging moments.
- Access to Help: Finding affordable or nearby addiction services is tough in some places.
- Relapse Risk: People at high risk might also fall back into old patterns if life gets stressful or they feel isolated.
How Relapse Happens
Going through tough times or being around old triggers can set off cravings, even after long periods without using. That’s why building intense routines, new relationships, and healthier outlets for stress is super important for those with a history of addiction in the family or earlier struggles themselves.
Real-World Examples of Risk Factors
It helps to see how these factors play out day to day. Imagine a college student under heavy academic and social pressure: late-night study sessions, lots of parties, and perhaps a roommate who likes to drink. Toss in feelings of anxiety or self-doubt, and it’s easy to see how risky patterns can start. Or a veteran returning from deployment who’s adjusting to civilian life; sometimes PTSD and tough transitions can steer a person toward unhealthy, quick fixes. Someone going through a breakup or a significant loss may find comfort in alcohol or other substances, especially if their support system is shaky or they grew up in a home where addiction was around. Even people recovering from major life events or job changes can fall into substance use, especially if there are genetically influenced vulnerabilities or challenging environments at play.
- College Students: Higher social pressures combined with academic stress sometimes led to higher alcohol or drug use, especially for those already anxious or struggling with depression.
- Military Veterans: PTSD and stressful transitions back to civilian life can increase the chances of substance use issues.
- People recovering from Major Life Events: Losing a job, going through a breakup, or grieving, can nudge even stable people toward unhealthy coping methods, especially if there’s a genetic or environmental push as well.
Frequently Asked Questions
Here are some questions I hear often when talking with people about addiction:
Question: Does weak willpower always cause addiction?
Answer: Not at all. Genetics, brain chemistry, life experiences, and mental health can all make it really tough to resist substances, even for people who want to quit.
Question: Can someone avoid addiction if it runs in the family?
Answer: It’s not guaranteed, but healthy coping skills, sound support systems, and awareness of personal risk factors can help significantly reduce the odds.
Question: Why do some people get hooked immediately, while others don’t?
Answer: Differences in genes, brain structure, personality type, and even the first experiences with a substance all play a role in how quickly addiction develops.
Question: Does treating mental health help with addiction?
Answer: Yes. Most experts recommend addressing both simultaneously since the two are often linked.
Healthy Ways to Lower Your Risk
Even if someone is at higher risk, many things have been proven to help prevent and recover. Building robust support networks, learning stress-relief strategies, getting mental health care, and setting boundaries with risky environments offer solid protection. Staying curious about self-care and keeping communication open with friends or professionals can make all the difference.
Understanding why addiction hits some folks harder can remove the shame and help more people find the help they need. Awareness, pro-active self-care, and a nonjudgmental approach support those who struggle; sometimes that awareness is the first step in breaking the cycle.
Anyone reading this who might be concerned for themselves or someone they care about knows that reaching out is never a sign of weakness. Dedicated professionals, online resources, and peer support groups are ready to step up. Sharing your story with someone trustworthy can be an incredible first step toward recovery. If you ever feel unsure, checking in with a healthcare expert is a solid move; they can help you spot risks, game plan practical solutions, and keep you moving forward.
Video: What’s The REAL Reason Addiction Affects People Differently?