Addiction shows up in all sorts of forms, including alcohol, drugs, gambling, food, internet use, and much more. While every person’s experience is different, there are some key traits and patterns that a lot of people with addiction share, no matter the specifics. My goal here is to break down what people with addiction often have in common, in clear, straightforward terms.
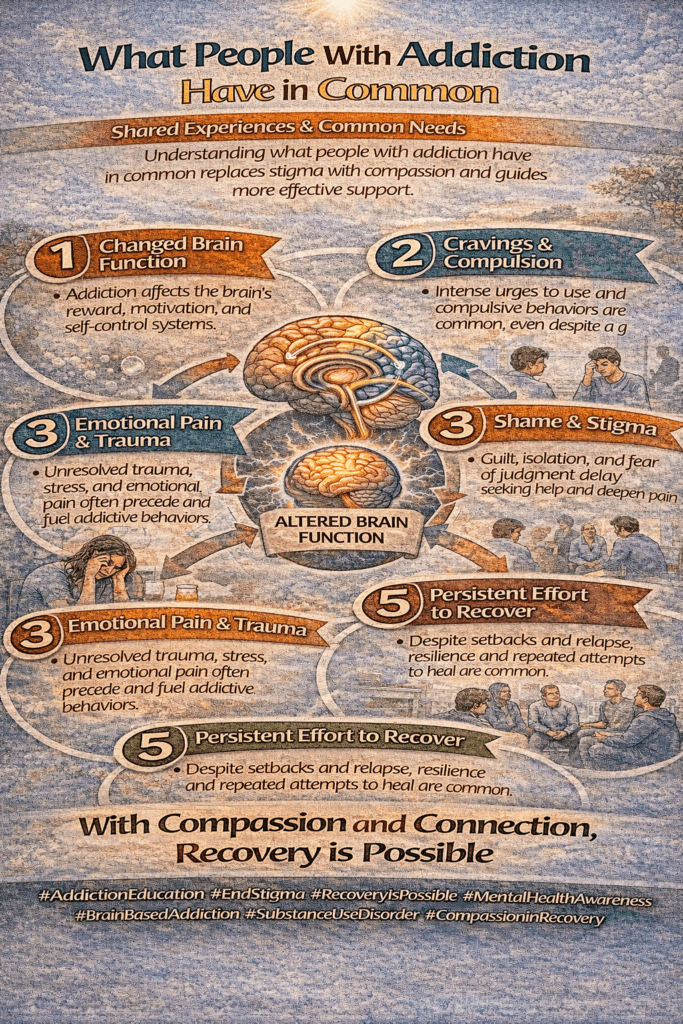
Shared Patterns in Addiction
No matter the addiction, certain patterns tend to repeat themselves in people’s lives. These patterns usually show up across different backgrounds, ages, and circumstances. While individual stories are always unique, there’s a pretty reliable framework that helps explain what’s going on and why so many folks struggle for so long.
Addiction usually doesn’t develop overnight. There’s a slow creep; maybe it starts out as something social or relaxing, and then it turns into more than just an occasional thing. Over time, people find themselves dealing with behavior patterns that feel nearly impossible to break. Once you know about these patterns, it’s easier to understand both yourself and others affected by addiction.
Some expert sources, like the National Institute on Drug Abuse, point out that about 1 in 10 Americans struggles with substance use disorder at some point. That number doesn’t even count other types of addiction. So you’re absolutely not alone in noticing these same patterns showing up again and again (NIDA).
Common Emotional and Psychological Traits
One thing I’ve seen over and over is that addiction isn’t just about what someone takes or does, it’s about how they feel inside. Here’s what usually pops up:
- Difficulty Managing Emotions: A lot of people who struggle with addiction report that feelings like stress, sadness, guilt, or anger can feel totally overwhelming. Substance use or addictive behaviors sometimes become a way to get temporary relief from all those intense feelings.
- Low Self-Esteem: It’s pretty common for those with addiction to feel like they don’t measure up, or that they’re not good enough. This can create a cycle: using something to feel better, then feeling bad about using it, and going right back to square one.
- Impulsivity: The urge to seek a quick high, escape, or immediate reward can drown out long-term thinking. Acting on impulse without a lot of thought often plays a big role in sustaining addictive habits.
- Difficulty Handling Stress: Coping with everyday challenges can feel tougher, and the addicted behavior becomes a go-to strategy for numbing out or managing discomfort.
I’ve heard many experts, plus people in recovery, say that tackling the underlying emotional struggles is just as important as changing the behavior. Getting to the root emotions is a big part of long-term recovery success. If someone keeps relapsing, sometimes it’s a sign that their emotional needs aren’t being met, so therapy and new coping tools become even more important.
How Addiction Shows Up Physically and Behaviorally
The mental side of addiction often goes hand-in-hand with physical and behavioral changes. You might notice things like:
- Developing Tolerance: Someone who’s addicted tends to need more and more of whatever they’re using to get the same effect. This pattern keeps the cycle going and can put physical health at risk.
- Withdrawal Symptoms: When someone tries to cut back or stop, withdrawal can hit hard; symptoms might be physical, emotional, or both. This makes quitting super tough for a lot of people.
- Losing Control: Attempts to cut back often fail, even if the person really wants to change. Promises to self or others tend to fall through because the urge and cravings overpower logic.
- Neglecting Responsibilities: Work, family, friendships, and basic self-care sometimes get pushed aside for the addiction. This can spiral into all sorts of new stress and life consequences, which then feed the cycle further.
Physical changes and risky behavior sometimes show up so gradually that even loved ones only realize something is wrong after things have gotten pretty serious. Recognizing these signs early can help prevent bigger problems down the line. It’s also common for health to decline or for people to lose interest in previous activities as a result of these behaviors.
Social and Environmental Influences
One thing I always highlight is how addiction almost never happens in a vacuum. The people you spend time with, your community, and your living situation all play a part. Here are some common threads:
- Family History: People with parents or close relatives who had addiction issues are more likely to struggle themselves. Sometimes it’s genetic, other times it’s about learned behaviors growing up.
- Social Circles: Hanging out with others who use drugs, drink, or have their own addictions makes it a lot easier to fall into the same patterns. Peer pressure is no joke, especially in your teens and 20s.
- Lack of Support: Feeling disconnected from people or having no one to talk to about stress increases the risk. Many people with addiction feel isolated, which only pushes them further into their habits.
- Environment: Easy access to whatever substance or behavior you’re addicted to, plus stressful, unpredictable life circumstances, can really increase the odds of developing an addiction.
This idea of social risk factors is supported by a bunch of research, and I see it reflected in personal stories too. Sometimes, changing your environment is a big step toward recovery, even if it’s tough at first. School, workplace, and even media messages can shape what feels normal or acceptable when it comes to addictive behaviors.
Barriers to Recovery You’ll Probably Run Into
If kicking an addiction were easy, way more people would do it on the first try. There are some really common barriers that almost everyone with addiction faces, and being aware of them helps.
- Denial: Many people minimize or hide the problem, even from themselves. Facing the reality of addiction can be scary, so denial becomes a coping strategy.
- Fear of Change: The idea of giving up something that’s become a coping tool can feel like losing your security blanket. Anxiety about withdrawal, failure, or coping with stress without the addiction can make people stick to old habits.
- Stigma: Worry about being judged or labeled keeps many people from reaching out. Society still has unfair attitudes about addiction, making it even harder to ask for support.
- Relapse: Slipping up is very common and can cause shame or hopelessness. Recovery usually isn’t a straight line, and knowing that setbacks are common helps with getting back on track.
Therapists and support groups often stress that setbacks don’t mean failure; they’re just part of the process for most people. The main thing is to keep going, ask for help, and reach out for new coping strategies when needed. Learning to let go of self-blame can be an important part of moving forward, as can trying different paths to recovery until something sticks.
Recognizing These Patterns in Everyday Life
If you’re wondering if you or someone you know is dealing with these common addictive patterns, here are some quick questions to help check:
- Is there a mounting need to use more of something for the same effect?
- Have things you used to enjoy, like hobbies, friends, or work, fallen off the radar?
- Are you spending more time thinking about, planning, or hiding your behavior?
- Do you feel anxious or irritable if you can’t use or engage in the addiction?
If you find yourself nodding along to a few of these, you’re definitely not alone. Seeking information is a good first step, and reaching out to support groups or professionals can make a real difference. Sometimes, self-help books and online forums offer additional guidance, especially in the early days before reaching out to someone in person feels possible.
Tried-and-True Ways People Get Back on Track
Getting out of addiction usually means trying more than one thing. Here are some strategies that come up again and again:
- Therapy: Talking with someone trained in addiction can help break down denial, find healthier coping approaches, and make a practical plan. Therapists can suggest new exercises for managing cravings and stress, turning difficult moments into learning experiences.
- Support Groups: Groups like AA, NA, and SMART Recovery connect you with others who get it. Sharing experiences and advice is super helpful. The sense of fellowship itself can boost motivation and accountability.
- New Routines: Building a different daily rhythm to replace triggers and old patterns is key. This could be anything from exercise to meditation or creative hobbies. New, positive habits can crowd out the old behaviors.
- Honest Conversations: Reaching out to family or close friends for support, even when it feels awkward, usually helps lighten the emotional load. Honest chats also break the isolation that often keeps addiction going.
- Professional Help: Sometimes withdrawal is unsafe to handle alone, and medical oversight is safest. There’s no shame in seeking outside help for detox or counseling. Medical professionals can also help address any underlying mental health or physical problems.
Recovery isn’t necessarily about willpower; it often means making changes one step at a time, and sometimes leaning into the vulnerability that comes from admitting you need help. The main thing is to try again, even after setbacks, and know you’re not the only one dealing with these shared challenges. Recovery is possible, and many people have rebuilt better, fuller lives after addiction.
Frequently Asked Questions
Here are a few common questions I see a lot when people start learning about addiction:
Question: Is addiction always physical?
Answer: Not always. Some addictions, like gambling or gaming, are behavioral but don’t involve a substance. Both can be equally tough to overcome, and they share many of the same patterns.
Question: Can people overcome addiction on their own?
Answer: Some do, but most people do better with some kind of outside support, such as therapy, groups, or trusted friends. There’s no shame in needing help.
Question: Why do some people become addicted while others don’t?
Answer: It’s a mix of genetics, environment, mental health, and personal history. No one is immune, but some people have more risk factors than others.
Question: How long does recovery take?
Answer: It varies for everyone. For many, it’s a lifelong process of learning new skills and managing setbacks, one step at a time. Patience is key, and ongoing support makes it easier.
Key Takeaways on What People With Addiction Have in Common
Most people with addiction share some patterns, traits, and challenges, even though every adventure is unique. Recognizing these common threads makes it easier to support yourself or someone you care about. If you want to read more about addiction science, check out SAMHSA’s resources or find a local support group in your area. Remember, reaching out or even just seeking information is a brave and hopeful step forward.
Video: The Common Thread in Every Addiction #addiction #mentalhealth #brainscience