Stimulant addiction occurs when drugs like amphetamines, cocaine, or prescription stimulants alter the brain’s reward system, leading to dependence and compulsive use. It often begins as a way to boost focus or manage stress but quickly turns into a harmful cycle of craving and tolerance. Preventing stimulant addiction requires a holistic approach—through self-management strategies that promote healthy coping, family support that fosters accountability and understanding, and community resources that provide education and early intervention. Together, these supports help individuals build resilience and reduce the risk of addiction.
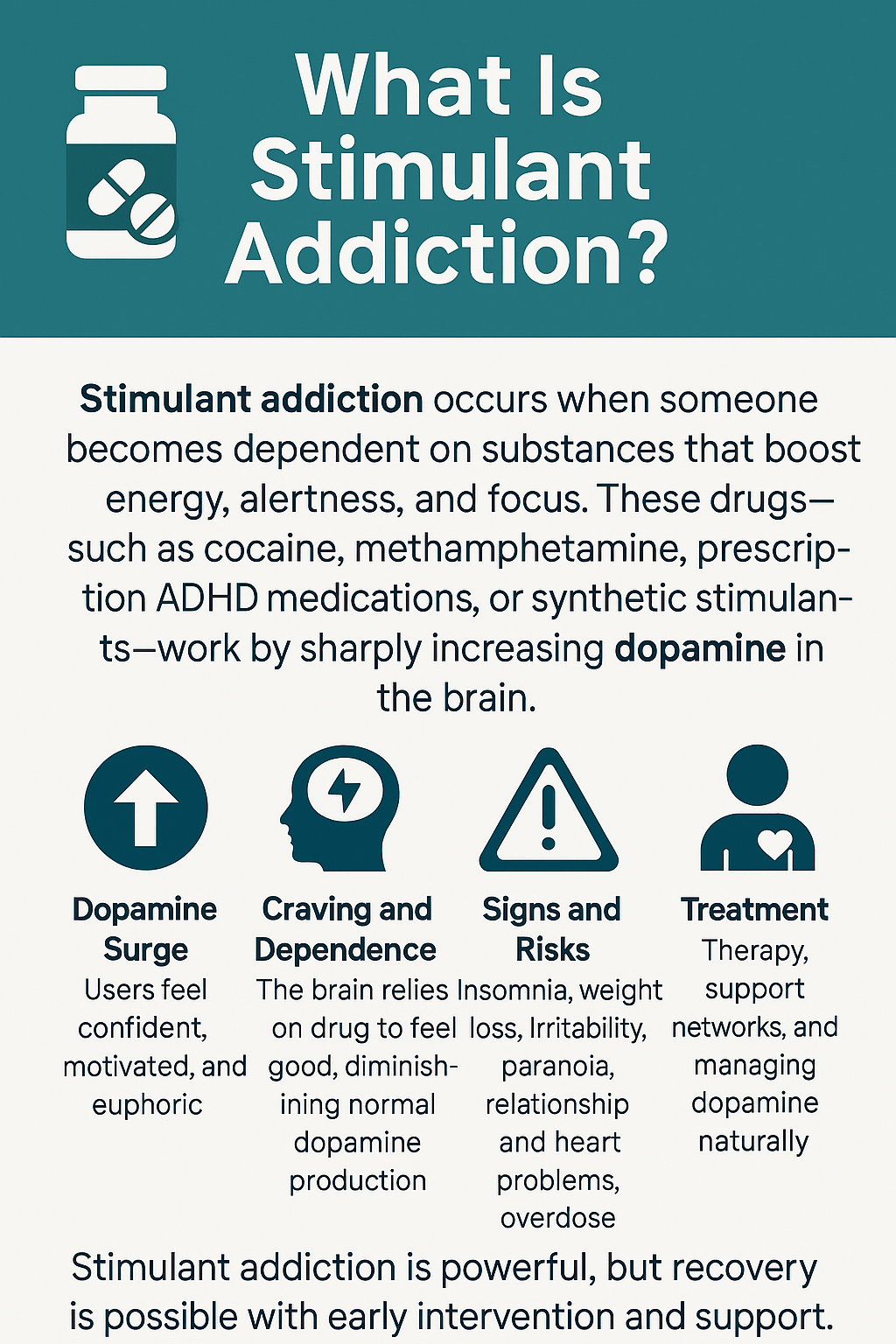
What Is Stimulant Addiction?
Stimulant addiction is a chronic condition in which a person becomes physically and psychologically dependent on stimulant substances—drugs that increase alertness, focus, and energy by elevating dopamine and norepinephrine levels in the brain. Over time, this repeated stimulation changes brain chemistry, making the brain rely on stimulants just to function normally.
⚡ Common Stimulants
Prescription Stimulants
- Adderall (amphetamine)
- Ritalin, Concerta (methylphenidate)
- Dextroamphetamine
Illicit Stimulants
- Cocaine, crack cocaine
- Methamphetamine
- MDMA (ecstasy)
- Synthetic cathinones (“bath salts”)
Mild Stimulants
- Caffeine
- Nicotine
(These are stimulants, but addiction typically looks different compared to stronger drugs.)
🧠 How Stimulant Addiction Works
Stimulants activate the brain’s reward system, producing intense bursts of energy, motivation, focus, or euphoria. Over time, this causes changes in the prefrontal cortex (responsible for decision-making) and the limbic system (linked to cravings and emotions).
The result:
- Strong cravings
- Decreased control
- Needing the drug to feel “normal”
🚨 Signs and Symptoms
- Increased energy, talkativeness, or euphoria
- Extreme focus or restlessness
- Appetite loss; sleeping less
- Dilated pupils; fast heart rate
- Paranoia, irritability, or agitation
- “Crash” phases: fatigue, depression, irritability
- Neglecting work, school, or relationships
- Inability to stop despite harm
💉 Health Risks
- Heart attack, stroke, or dangerously high blood pressure
- Anxiety, panic attacks, or stimulant-induced psychosis
- Severe weight loss and malnutrition
- Memory problems and cognitive decline
- Sleep deprivation
- High overdose risk (especially with polysubstance use)
💬 Treatment and Recovery
Effective treatment requires a comprehensive, supportive approach:
1. Detoxification
Safe management of withdrawal symptoms such as depression, fatigue, and cravings.
2. Behavioral Therapies
- Cognitive Behavioral Therapy (CBT)
- Contingency Management (reward-based support)
- Motivational Interviewing (MI)
These help change thinking patterns, build coping skills, and reduce cravings.
3. Medications
There are no FDA-approved medications yet, but research is exploring options to stabilize mood and reduce cravings.
4. Support Networks
- Peer recovery groups
- Family support
- Community programs
- Professional counseling
Support systems greatly improve long-term outcomes.
✅ Summary
Stimulant addiction is a brain-based relapsing condition marked by compulsive drug use and powerful cravings. With early intervention, behavioral therapy, and strong support networks, individuals can recover, rebuild stability, and regain control of their lives.
Self-Management Strategies to Prevent Stimulant Addiction
Preventing stimulant addiction begins with awareness—understanding why stimulants are used, how dependence develops, and which daily habits either reduce or increase risk. Whether someone uses prescription stimulants for medical reasons or encounters illicit stimulants in social or academic settings, strong self-management strategies can protect brain health, emotional well-being, and long-term stability. Below are science-based approaches rooted in prevention science, behavioral psychology, and neuroscience.
🧠 1. Understand the Risk and Purpose of Use
Healthy stimulant use starts with clarity.
- Know your intention—whether it’s for focus, energy, or mood.
- If prescribed for ADHD or another condition, follow dosage and timing exactly as directed.
- Avoid using stimulants to self-medicate stress, fatigue, anxiety, or academic pressure—the most common pathway to dependence.
Understanding why you reach for stimulants helps identify triggers early.
⏱️ 2. Build Healthy Routines for Energy and Focus
Most stimulant misuse begins when natural energy is low. Protect your body’s rhythms by supporting them.
- Sleep (7–9 hours) each night; chronic exhaustion increases misuse.
- Fuel your brain with balanced meals, protein, and complex carbohydrates.
- Exercise regularly, which naturally boosts dopamine and norepinephrine—the same neurotransmitters stimulants target.
Strong routines reduce the need for artificial boosts.
💬 3. Manage Stress and Emotional Triggers
Stimulants are often misused to cope with pressure or emotional discomfort.
- Practice mindfulness, meditation, or breathing exercises to lower stress.
- Use healthy coping skills like journaling, art, or nature time.
- Seek therapy early if emotional distress increases your temptation to use.
Emotional regulation is one of the strongest protective factors against addiction.
📱 4. Limit Exposure and Peer Pressure
Environment matters.
- Avoid settings where stimulant misuse is normalized (college parties, “study drug” circles).
- Learn to say no confidently and help shift conversations toward healthier habits.
- Use academic support services or tutoring instead of relying on illicit performance-enhancers.
A strong environment can prevent high-risk situations altogether.
🧭 5. Monitor Your Behavior and Mindset
Self-awareness is key to catching early warning signs.
- Keep a self-check log of sleep, mood, and energy.
- Notice when thoughts like “I need something to keep up” start appearing.
- Reflect weekly on your reliance on caffeine or stimulants.
- Reach out for help if tolerance or cravings begin to form.
Monitoring your internal cues protects against escalation.
🫶 6. Build a Support System
Connection strengthens resilience.
- Stay close with loved ones who support healthy living.
- Join wellness or mental health groups to share stress-management strategies.
- Be honest with healthcare providers about energy challenges or temptation to misuse medication.
A supportive network provides accountability and guidance.
✅ Summary
Preventing stimulant addiction requires self-awareness, balanced routines, emotional regulation, strong boundaries, and supportive relationships. By prioritizing sleep, nutrition, exercise, mental health, and honest communication, individuals can maintain natural energy, reduce risk, and stay aligned with healthy recovery-focused choices.
Family Support Strategies to Prevent Stimulant Addiction in Teens and Young Adults
Preventing stimulant addiction starts at home. Teens and young adults often face intense pressure—from academics, sports, social expectations, or managing emotions. Families play a powerful role in shaping healthy habits, emotional resilience, and safe attitudes toward substances. By creating a supportive, informed, and structured environment, families can significantly reduce the likelihood of stimulant misuse. Here are evidence-based strategies that make a meaningful difference.
👨👩👧 1. Open and Honest Communication
Regular, compassionate conversations help teens feel heard and supported.
- Discuss stress, school demands, friendships, and pressure to perform—common triggers for stimulant misuse.
- Keep the tone calm and nonjudgmental so your child feels safe sharing concerns.
- Talk openly about the risks of misusing prescription “study drugs” like Adderall or illegal stimulants like cocaine or methamphetamine.
Open communication reduces secrecy and increases trust.
🧠 2. Education and Awareness
Knowledge protects teens from misinformation.
- Learn the warning signs of stimulant misuse—changes in mood, appetite, sleep, or sudden bursts of energy.
- Explain how stimulants affect the brain, including risks of dependence and reduced impulse control.
- If someone in the household uses prescription stimulants, keep them securely stored and emphasize the dangers of sharing medication.
Educated families recognize problems early and respond quickly.
🕰️ 3. Model Healthy Coping and Lifestyle Habits
Teens watch how adults handle stress and productivity.
- Demonstrate healthy patterns of sleep, nutrition, and physical activity.
- Show that rest is normal—not something to avoid or “push through.”
- Be mindful not to normalize using caffeine, pills, or energy supplements to manage busy schedules.
Healthy modeling teaches teens sustainable ways to manage pressure.
🤝 4. Strengthen Emotional Support and Connection
Feeling supported reduces the urge to seek escape or enhancement.
- Build strong emotional bonds through quality time and open dialogue.
- Reinforce that their worth is not defined by grades or performance.
- Praise effort, consistency, and resilience, not just achievements.
Emotional safety reduces the likelihood of turning to stimulants for confidence or energy.
🏫 5. Collaborate with Schools and Healthcare Providers
A united support system helps prevent high-risk behaviors.
- Stay informed about academic expectations and pressures your teen may face.
- Work with teachers or counselors to promote healthy study habits, time management, and stress-reduction strategies.
- If your child is prescribed stimulants for ADHD, maintain regular communication with the prescriber to ensure safe dosing and monitoring.
Partnerships ensure teens receive consistent and supportive guidance.
🔒 6. Set Boundaries and Structure
Clear structure helps teens feel grounded and safe.
- Store prescription medications securely to prevent access or sharing.
- Set clear rules regarding substance use, including misuse of prescriptions.
- Encourage offline hobbies, screen-free relaxation, and balanced routines that reduce stress and impulsivity.
Healthy boundaries protect both mental health and physical safety.
🌍 7. Encourage Community and Peer Involvement
A sense of belonging reduces the appeal of substance use.
- Connect teens with positive groups—sports teams, youth clubs, volunteer work, or mentorship programs.
- Support involvement in substance-free social events and wellness activities.
- Participate together in community events or workshops on addiction prevention and healthy coping.
Community engagement builds resilience and positive identity.
✅ Summary
Family support is one of the strongest protective factors against stimulant addiction. By promoting open communication, educating teens about risks, modeling healthy habits, fostering emotional connection, coordinating with schools and clinicians, setting boundaries, and encouraging community involvement, families create an environment where balance—not performance—drives well-being. A connected, informed, and supportive home reduces the need for teens to seek artificial boosts to manage stress, energy, or expectations.
Community Strategies to Prevent Stimulant Addiction
Preventing stimulant addiction isn’t just an individual or family responsibility—it’s a community-wide effort. Schools, health systems, organizations, and local leaders all play a vital role in shaping environments that protect teens and young adults from pressures that lead to stimulant misuse. By focusing on education, access to care, and supportive networks, communities can create strong layers of prevention that reduce risk long before addiction begins.
🏥 1. Community Health and Prevention Programs
Community health systems serve as the first line of prevention.
- Early Screening & Education: Health departments and clinics can provide screenings in schools or youth centers to identify early misuse or risk factors like academic stress, anxiety, or sleep issues.
- Public Health Campaigns: Awareness messaging about the dangers of prescription stimulant misuse and safe medication practices can reach broad audiences.
- Accessible Counseling: Low-cost or free mental health services help youth manage stress or performance pressure without turning to stimulants.
Preventive care becomes more effective when it’s accessible, stigma-free, and easy to navigate.
🎓 2. School and Youth Initiatives
Schools shape daily routines and expectations for youth.
- Life Skills Education: Teach healthy coping, stress management, time management, and study skills.
- Teacher & Counselor Training: Equip staff to recognize signs of stimulant misuse early and guide students to appropriate resources.
- Peer Mentorship Programs: Promote substance-free clubs, after-school activities, and leadership groups that reinforce healthy choices.
Schools that prioritize wellness create a strong barrier against stimulant misuse.
🤝 3. Collaboration with Local Organizations
Community organizations amplify prevention efforts.
- Partnerships with Nonprofits & Faith-Based Groups: Host workshops, prevention seminars, and supportive programming for families.
- Parent Education: Provide resources that help parents understand stimulant risks and recognize early warning signs.
- Community Coalitions: Bring together schools, healthcare providers, law enforcement, and youth groups to coordinate prevention strategies.
Shared responsibility leads to stronger, more consistent support.
📱 4. Accessible Digital and AI Tools
Technology can support prevention when used safely.
- AI-Based Prevention Tools: Apps that track mood, promote study skills, or encourage stress reduction offer healthier alternatives to stimulant misuse.
- Digital Outreach Campaigns: Social media and online content can spread awareness quickly and connect youth with mental health services.
Digital supports help meet youth where they already spend most of their time—online.
⚖️ 5. Policy and Advocacy Support
Policy-level strategies ensure long-term community protection.
- Medication Safety Policies: Promote safe storage and disposal of prescriptions to prevent diversion or sharing.
- Advocacy for Funding: Push for more mental health resources, addiction-prevention programs, and youth support services.
- Community Oversight: Ethical boards or youth advisory groups can guide how prevention technology, including AI, is implemented.
Stronger policies create safer environments for all.
🌍 6. Promote Social and Cultural Engagement
Connection and belonging reduce the appeal of substances.
- Volunteer Opportunities: Encouraging community involvement helps youth build purpose and confidence.
- Recreational Activities: Investment in sports, arts, music, and cultural programs provides healthy ways to manage stress.
- Culturally Tailored Outreach: Prevention messages should respect cultural norms, reduce stigma, and feel inclusive.
Communities that foster belonging make stimulant misuse less attractive.
✅ Summary
Community strategies to prevent stimulant addiction emphasize education, prevention, access to care, connection, and cultural inclusion. When schools, families, health systems, and organizations work together, they create a robust safety net that helps youth build resilience, manage stress, and access help early. Strong, connected communities reduce the pressures that drive stimulant misuse—and make healthy, balanced living the easier choice.
Frequently Asked Questions
Here are some common questions:
Question: Is caffeine or nicotine considered a stimulant addiction?
Answer: Caffeine and nicotine are stimulants, and both can lead to addiction, but they differ from stronger stimulants in intensity, risk, and impact on daily life.
Here’s a clear breakdown:
☕ Is Caffeine a Stimulant Addiction?
Yes — caffeine is a mild stimulant and can cause dependency.
What it does:
Caffeine increases alertness by elevating dopamine and blocking adenosine (the “sleepiness” chemical).
Signs of caffeine dependence:
- Needing more caffeine to feel awake
- Headaches, fatigue, or irritability without it
- Difficulty cutting back
- Use interfering with sleep or anxiety levels
Severity:
Caffeine dependence is usually milder and less harmful than addiction to prescription stimulants, cocaine, or meth.
However, for some individuals—especially teens, people with anxiety, or heavy energy drink users—caffeine can contribute to:
- Heart palpitations
- Panic attacks
- Sleep disruption
- Increased stimulant-seeking behavior
🚬 Is Nicotine a Stimulant Addiction?
Absolutely — nicotine addiction is one of the most common stimulant addictions.
What it does:
Nicotine rapidly stimulates dopamine, adrenaline, and norepinephrine, increasing alertness, focus, and mood.
Why it’s highly addictive:
- Effects hit the brain in seconds
- Fast “spike and crash” pattern encourages frequent use
- Strong physical and psychological dependence
Risks:
- Heart disease, stroke
- Lung cancer (with smoked forms)
- Increased anxiety, irritability, and withdrawal cravings
- Higher risk of relapse in other substance addictions
Forms of use:
- Cigarettes
- Vapes/e-cigarettes
- Nicotine pouches
- Chewing tobacco
Nicotine is considered one of the most addictive legal stimulants, especially among teens due to vaping.
🌡️ How They Compare to Other Stimulant Addictions
| Substance | Addiction Risk | Health Risks | Typical Pattern |
|---|---|---|---|
| Caffeine | Low–moderate | Sleep issues, anxiety | Daily dependence |
| Nicotine | High | Cardiovascular & respiratory harm | Frequent cravings |
| Prescription stimulants | High (if misused) | Heart risks, mental health effects | Escalating misuse |
| Cocaine/Meth | Very high | Severe physical & mental harm | Rapid addiction |
Summary
Both alter brain chemistry and can contribute to the cycle of stimulant dependence, especially in teens or individuals with high stress, poor sleep, or mental health conditions.
Caffeine → mild stimulant, can cause dependence but usually not severe addiction.
Nicotine → highly addictive stimulant, one of the most common and harmful addictions worldwide.
Question: Is detox needed for stimulant addiction?
Answer: Detox may be helpful for stimulant addiction, but it is not always required in the same way it is for alcohol, benzodiazepines, or opioids.
Here’s a clear explanation:
🧠 Why Stimulant Detox Is Different
Stimulants (like cocaine, methamphetamine, or Adderall) do not cause life-threatening physical withdrawal the way alcohol or opioids can.
However, they do cause intense psychological and emotional withdrawal symptoms.
⚠️ When Detox Is Helpful
Detox is recommended when withdrawal symptoms are severe, unsafe, or unmanageable, including:
Common stimulant withdrawal symptoms
- Extreme fatigue
- Depression or hopelessness
- Anxiety or panic
- Irritability or agitation
- Intense cravings
- Sleep problems
- Low motivation
- Difficulty thinking clearly
Red-flag symptoms needing medical supervision
- Suicidal thoughts
- Severe depression
- Psychosis (paranoia, hallucinations)
- Aggression or confusion
- Co-occurring substance use (alcohol, opioids, benzos)
In these cases, medical detox provides monitoring, safety, and emotional stabilization.
🏥 What Stimulant Detox Usually Looks Like
Unlike opioid or alcohol detox, stimulant detox typically focuses on:
1. Medical Monitoring
- Monitoring sleep, hydration, heart rate, mental health
- Providing a safe environment during the “crash” phase
2. Symptom Management
- Sleep support
- Nutritional support
- Anxiety and mood stabilization
- Treatment for co-occurring mental health issues
3. Crisis Management
- Safety checks for self-harm risk
- Managing stimulant-induced psychosis
4. Transition to Treatment
Because cravings return quickly, detox is followed immediately by therapy or outpatient care.
🧭 When Detox Is Not Needed
Some individuals with mild or moderate stimulant misuse can safely begin treatment without detox if they do not experience:
- Severe depression
- Psychosis
- Suicidal thoughts
- High-risk binge patterns
- Co-occurring substance dependencies
In these cases, outpatient behavioral therapies (CBT, Contingency Management, MI) are often the first step.
✅ Summary
Even when detox isn’t needed, immediate follow-up treatment is essential due to strong cravings and relapse risk.
Detox is not medically required for everyone with stimulant addiction, but it can be very important when psychological withdrawal is severe.
Stimulant withdrawal can trigger dangerous mood symptoms, so professional support is often recommended.
Question: How is stimulant addiction diagnosed?
Answer: Stimulant addiction is diagnosed through a clinical evaluation, not a single test. Healthcare providers use a combination of interviews, behavioral assessments, and medical tools to determine whether someone meets criteria for a stimulant use disorder. Here’s a clear, step-by-step explanation:
🧠 1. Clinical Interview (Most Important Step)
A clinician (doctor, psychologist, or addiction specialist) asks detailed questions about:
- Type of stimulant used (Adderall, cocaine, meth, etc.)
- Frequency and amount
- Reasons for use (energy, focus, mood, weight loss)
- Loss of control (“Do you take more than intended?”)
- Impact on responsibilities (school, work, relationships)
- Cravings or withdrawal symptoms
- Prior attempts to cut down
This helps identify patterns of problematic use.
📋 2. DSM-5 Diagnostic Criteria for Stimulant Use Disorder
Clinicians diagnose based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
A person may be diagnosed if they meet 2 or more of the following within a 12-month period:
- Taking more than intended
- Unsuccessful attempts to cut back
- Spending large amounts of time obtaining or recovering from stimulants
- Cravings
- Failure to meet obligations
- Continued use despite social or relationship problems
- Giving up activities
- Use in risky situations (driving, mixing substances)
- Continued use despite physical or psychological harm
- Developing tolerance
- Withdrawal symptoms
Severity is classified as:
- Mild: 2–3 symptoms
- Moderate: 4–5 symptoms
- Severe: 6+ symptoms
🧪 3. Physical and Mental Health Evaluation
Providers check for health effects related to stimulant misuse:
Physical signs
- Rapid heart rate or high blood pressure
- Weight loss or poor appetite
- Insomnia
- Dilated pupils
- Skin sores (especially with meth)
Mental health signs
- Anxiety or agitation
- Panic attacks
- Paranoia or hallucinations
- Mood swings
- Depression during “crash” cycles
This helps differentiate stimulant addiction from other conditions.
🧬 4. Screening Tools & Questionnaires
Clinicians may use validated screening tools such as:
- ASSIST (WHO Alcohol, Smoking, and Substance Involvement Screening Test)
- DAST-10 (Drug Abuse Screening Test)
- SDS (Severity of Dependence Scale)
- CRAFFT (for adolescents)
These measure severity, risk, and functional impairment.
💉 5. Toxicology or Drug Testing (Optional)
Urine, blood, or saliva tests can confirm recent stimulant use, but cannot diagnose addiction alone.
They simply provide supporting evidence.
🧭 6. Assessment for Co-Occurring Conditions
Providers check for mental health issues that often occur with stimulant addiction, such as:
- ADHD
- Anxiety disorders
- Depression
- Trauma or PTSD
- Eating disorders
- Sleep disorders
These conditions can drive stimulant misuse and affect treatment planning.
📌 Summary
Stimulant addiction is diagnosed through:
- A clinical interview
- The DSM-5 criteria
- A physical and mental health assessment
- Screening tools
- Optional toxicology testing
Diagnosis focuses on patterns of use, loss of control, harm, and withdrawal, not just a positive drug test.
Conclusion
Addressing stimulant addiction requires collaboration between individuals, families, and communities. While self-management builds personal resilience and coping skills, family support reinforces trust and consistency, and community resources expand access to prevention, education, and recovery care. Through early awareness, open communication, and coordinated action, the cycle of stimulant misuse can be interrupted before it becomes dependency. A united approach that integrates personal responsibility with social and community engagement creates the foundation for lasting recovery and healthier, addiction-free futures.
Video: Why Do People Get Hooked On Stimulants?