Virtual Reality Therapy (VRT) represents a groundbreaking evolution in addiction treatment, blending technology with psychology to create immersive, controlled environments for behavioral change. By simulating real-life triggers—such as bars, social gatherings, or stress-inducing settings—VRT allows individuals to confront cravings and practice coping strategies safely under therapist supervision. This approach enhances emotional regulation, relapse prevention, and self-awareness. However, adopting VRT also raises challenges, including costs, accessibility, and ethical dilemmas related to data privacy, emotional safety, and therapist competency. Determining whether this therapy is appropriate requires self-management insight, family collaboration, and informed community support to ensure that innovation enhances—not replaces—human-centered recovery care.
Virtual Reality Therapy in Addiction Treatment
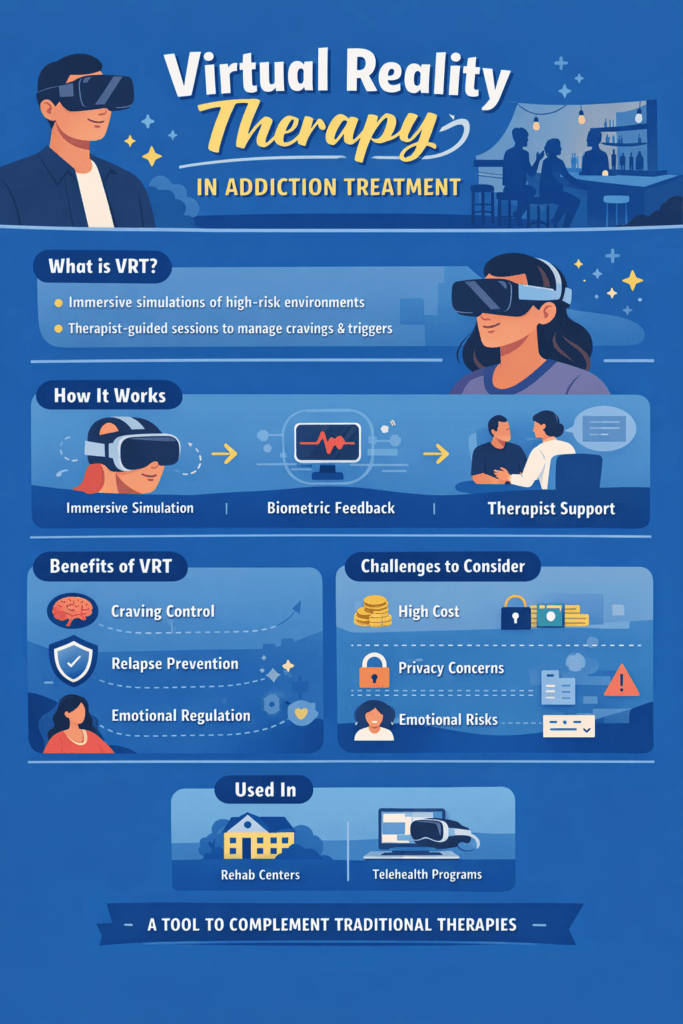
Virtual Reality Therapy (VRT) is an emerging, evidence-based approach in addiction treatment that uses immersive technology to help individuals understand, manage, and reduce substance use behaviors. By recreating real-life high-risk environments—such as bars, parties, or stressful situations—VRT allows clients to safely face triggers in a controlled setting under clinical supervision. This bridges the gap between learning coping skills in therapy and applying them in real-world situations.
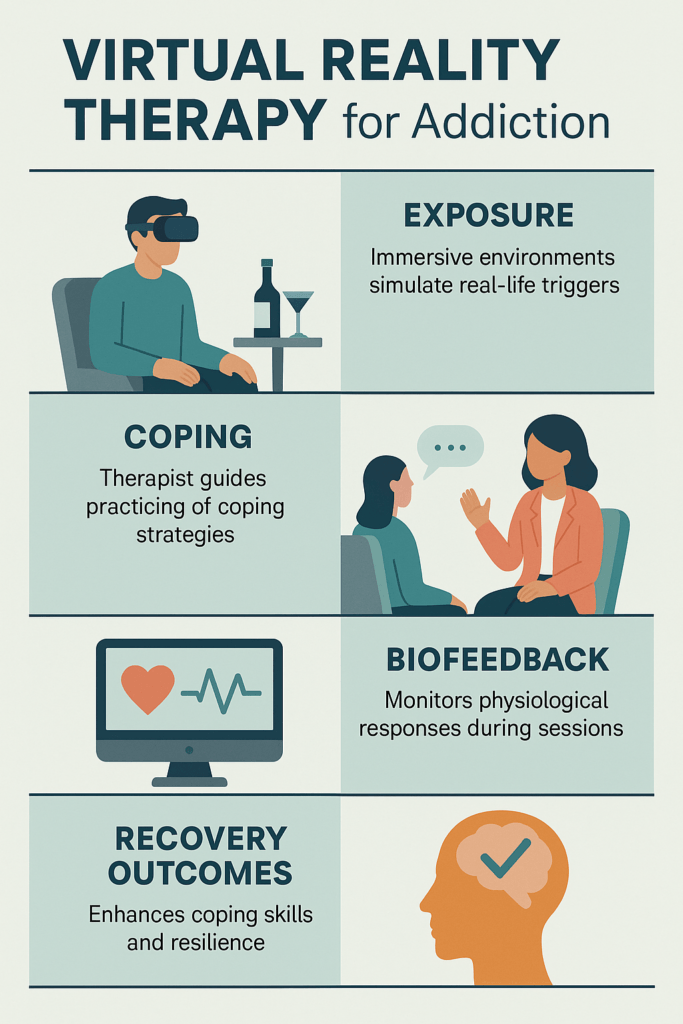
VRT works through immersive simulation. Clients wear a VR headset that places them inside realistic scenarios associated with past substance use, without actual exposure to drugs or alcohol. During sessions, therapists monitor emotional and physical reactions while guiding clients through coping techniques, mindfulness practices, and refusal skills. Some systems also integrate biometric feedback, such as heart rate or skin response, to measure stress and cravings in real time, allowing personalized interventions. With repeated exposure, individuals become desensitized to triggers, similar to exposure therapy used for anxiety, phobias, or PTSD.
Clinical benefits include improved craving management, stronger emotional regulation, and increased confidence in relapse prevention. VRT helps uncover hidden triggers tied to stress, social pressure, or emotional discomfort. It is most effective when combined with traditional approaches such as Cognitive Behavioral Therapy (CBT), Medication-Assisted Treatment (MAT), and group counseling.
Despite its promise, challenges remain. VR equipment can be costly, limiting accessibility. Ethical care is required to prevent emotional overwhelm during intense simulations. Additionally, current programs may not fully capture the unique personal experiences of every individual in recovery.
Today, many rehabilitation centers and research institutions incorporate VRT into early recovery programs and telehealth services. As technology becomes more affordable and personalized, Virtual Reality Therapy continues to expand its role in modern addiction care.
By transforming coping practice into lived experience, VRT strengthens self-awareness, emotional control, and relapse resistance—offering a powerful new pathway toward long-term recovery.
Disadvantages of Virtual Reality Therapy in Addiction Treatment
Virtual Reality Therapy (VRT) is gaining attention as an innovative tool in addiction treatment, but like any emerging technology, it comes with important limitations. Understanding these disadvantages helps clinicians, patients, and treatment programs use VRT responsibly and effectively rather than viewing it as a universal solution.
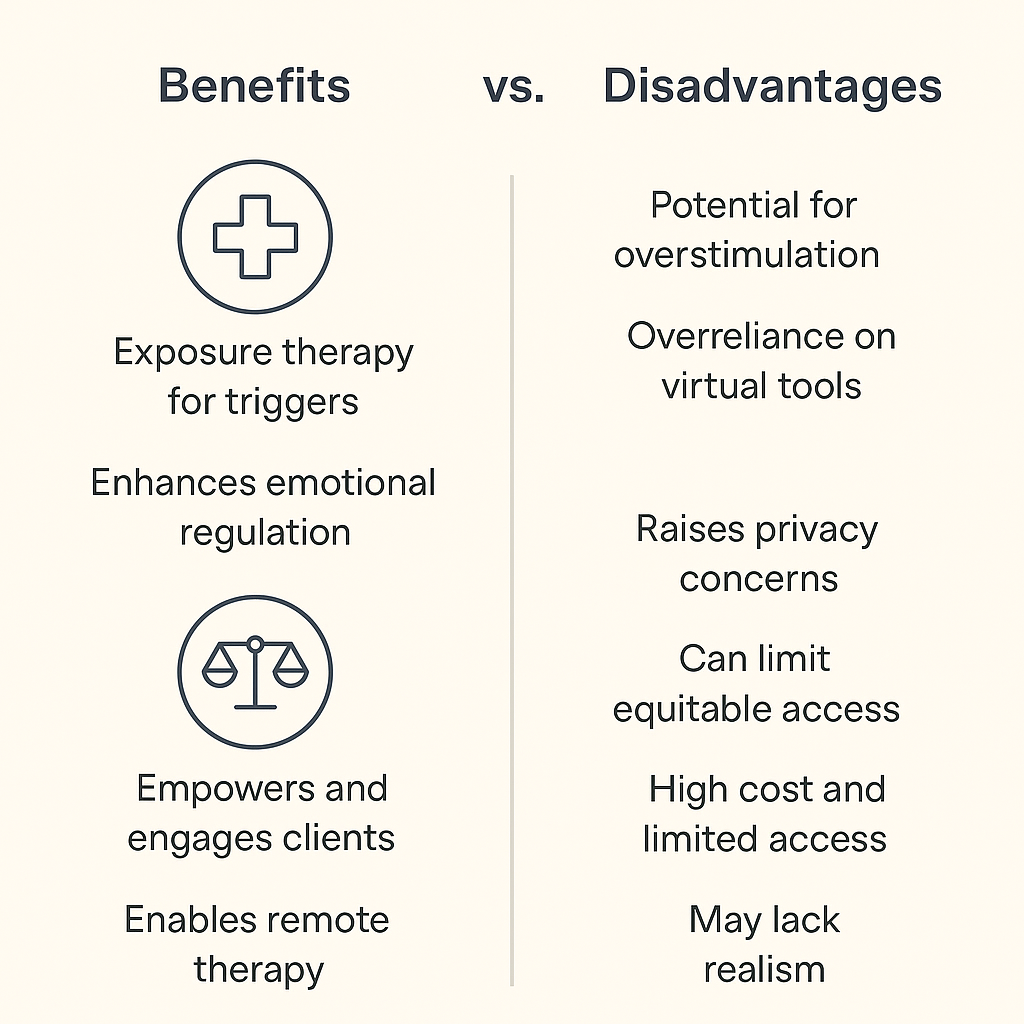
One of the largest barriers is cost and accessibility. VR equipment, specialized software, and ongoing technical support require significant financial investment. Smaller treatment centers, community clinics, and rural programs may struggle to afford or maintain these systems. This creates unequal access, with only well-funded facilities able to offer VRT, reinforcing existing healthcare disparities.
Another concern is emotional overstimulation. Because VR environments feel realistic, they can provoke strong emotional and physical reactions. Individuals with trauma histories, anxiety disorders, or severe cravings may become overwhelmed during simulations. Without skilled therapist guidance and careful debriefing, exposure to drug-related environments could unintentionally intensify distress or trigger cravings instead of reducing them.
Technical and design limitations also affect effectiveness. Virtual scenarios cannot yet capture the full complexity of real-world social pressures, emotional conflicts, or environmental unpredictability linked to substance use. Poor graphics, motion sickness, or system malfunctions may interrupt sessions and reduce engagement, making the experience less therapeutic.
Ethical and privacy issues present additional challenges. Many VRT systems collect biometric data such as heart rate, eye tracking, or stress responses. Protecting this sensitive information is critical, yet standardized ethical guidelines for VR use in addiction treatment are still developing. Some clients may also feel uncomfortable being monitored in immersive environments, creating concerns about vulnerability and consent.
Research limitations remain significant. Although early studies show promise, long-term evidence on relapse prevention and sustained recovery outcomes is still limited. There is no universal clinical protocol for session length, frequency, or substance-specific adaptation. Providers must balance innovation with scientific caution.
Finally, dependence on technology can shift focus away from real-world coping and human connection. Recovery is built on relationships, community support, and daily life practice. If VRT becomes overemphasized, it may weaken the therapeutic alliance or give clients a false sense of readiness outside controlled environments.
In summary, Virtual Reality Therapy offers exciting possibilities, but its disadvantages include high cost, limited access, emotional risk, technical constraints, ethical uncertainty, and insufficient long-term research. VRT works best as a supportive tool—complementing, not replacing—evidence-based therapies such as CBT, group counseling, and medication-assisted treatment.
Ethical Dilemmas of Virtual Reality Therapy in Addiction Treatment
Virtual Reality Therapy (VRT) is reshaping addiction treatment by offering immersive, real-world simulations that help individuals practice coping skills in controlled environments. However, the same realism that makes VRT powerful also introduces ethical dilemmas. As this technology becomes more common in recovery settings, clinicians must carefully balance innovation with patient protection, dignity, and trust.
A primary ethical concern is informed consent and emotional safety. Many clients may not fully anticipate how intense virtual exposure to substance-related environments can feel. Simulations may provoke cravings, anxiety, or trauma responses, particularly in early recovery. If patients are not thoroughly educated about these risks beforehand, consent cannot be considered fully informed. Ethical practice requires that clients understand what to expect, retain the right to stop sessions at any time, and receive proper emotional debriefing afterward.
Privacy and data security present another major dilemma. Many VR systems collect biometric and behavioral data such as heart rate, gaze patterns, and stress responses. These records reveal deeply personal psychological information. Without strict safeguards, there is a risk of data misuse or breaches that compromise confidentiality. Ethical implementation demands transparent data policies, secure storage, and clear limits on who can access patient information.
Psychological boundaries must also be protected. Because VR feels real, the line between therapeutic exposure and emotional manipulation can blur. Overly intense simulations may retraumatize clients or give a false sense of readiness for real-world challenges. Therapists must ensure sessions remain clinically guided, with grounding and reflection that connect virtual experiences to real-life recovery goals.
Equity and accessibility raise additional ethical questions. VR equipment and software remain costly, meaning advanced treatment options are often available only in well-funded or urban programs. This creates a digital divide in care. Ethical healthcare innovation requires striving for fair access so that technology enhances treatment opportunities rather than widening disparities.
Therapist competency and oversight are equally important. VRT demands both technical knowledge and advanced clinical skill. Without proper training, therapists may misuse exposure scenarios or rely too heavily on technology. Ethical responsibility requires ongoing education, supervision, and maintaining the therapist–client relationship as the core of treatment.
Finally, the lack of standardized guidelines and commercial pressures introduces integrity concerns. Some VR products enter the market without strong clinical validation. Patients may feel pressured to try “cutting-edge” therapy even if it does not suit their needs. Respect for autonomy means offering VRT as an optional supplement—not a replacement—for proven evidence-based treatments.
In summary, ethical dilemmas surrounding Virtual Reality Therapy in addiction care involve consent, privacy, emotional protection, fairness, clinician responsibility, and research integrity. When guided by transparency, empathy, and professional accountability, VRT can enhance recovery without compromising patient trust or ethical standards.
Self-Management Strategies for Deciding if Virtual Reality Therapy Is Right for Addiction Recovery
Virtual Reality Therapy (VRT) is an exciting advancement in addiction treatment, offering immersive environments where individuals can safely practice coping with real-world triggers. Yet, VRT is not the right fit for everyone or for every stage of recovery. Self-management strategies help individuals take an active role in determining whether this technology aligns with their needs, readiness, and recovery goals.
A helpful first step is self-assessment of readiness and trigger control. Because VRT recreates high-risk environments, individuals should honestly evaluate their emotional stability before starting. If cravings, anxiety, or trauma responses are still highly intense, immersive exposure may feel overwhelming rather than therapeutic. Asking yourself whether you feel grounded enough to face simulated triggers safely provides important insight into timing and preparedness.
Clarifying treatment goals is equally important. VRT works best when it supports specific recovery objectives such as craving management, relapse-prevention practice, or stress regulation. Individuals benefit from discussing with their clinician how VR sessions will fit alongside other treatments like Cognitive Behavioral Therapy, mindfulness training, or Medication-Assisted Treatment. When goals are clear, it becomes easier to judge whether VRT adds value rather than distracts.
Because VR programs vary widely in quality, researching program credibility protects against ineffective or unethical use. Individuals should ask whether the technology is research-supported, therapist-guided, and transparent about privacy protections for biometric data. Seeking recommendations from licensed addiction professionals rather than marketing materials ensures informed decision-making.
Developing emotional regulation skills strengthens safety during VR exposure. Practicing grounding techniques, journaling reactions after sessions, and scheduling debriefs with a therapist help individuals process emotions that arise in simulations. These strategies turn intense virtual experiences into meaningful therapeutic growth rather than emotional overload.
Involving support systems also improves outcomes. Discussing the decision with family, sponsors, or trusted peers provides perspective and reduces uncertainty about trying new technology. Sharing session experiences with supportive others reinforces accountability and emotional balance.
Finally, tracking progress allows individuals to evaluate whether VRT is truly beneficial. Monitoring cravings, stress responses, and confidence levels before and after sessions provides measurable feedback. If benefits plateau or distress increases, it may be time to adjust or discontinue VR use in collaboration with a clinician.
In summary, self-management strategies empower individuals to make informed choices about Virtual Reality Therapy. By assessing readiness, defining goals, verifying program quality, strengthening emotional coping, involving support, and tracking progress, individuals can determine whether VRT is a helpful complement to their recovery journey. When guided by self-awareness and professional support, technology becomes a tool for empowerment—not a substitute for healing.
Family Support Strategies for Deciding if Virtual Reality Therapy Is Right for Addiction Recovery
Virtual Reality Therapy (VRT) is an emerging tool in addiction treatment that allows individuals to practice coping with real-world triggers in a controlled, immersive environment. While this technology can be highly beneficial, it is not suitable for everyone or every stage of recovery. Families play a vital role in helping loved ones evaluate whether VRT is an appropriate and safe option. Supportive involvement grounded in communication, education, and respect can make this decision clearer and more empowering.
Open and nonjudgmental communication is the foundation. Families should create a safe space to discuss VRT without pressure or skepticism. Asking curious, supportive questions about interest, expectations, and concerns helps loved ones feel heard rather than directed. When families explore information together—watching demonstrations, reading credible sources, or discussing treatment center materials—the decision becomes shared rather than imposed.
Understanding the technology and its purpose allows families to provide informed guidance. Attending orientation sessions, asking clinicians how VR scenarios are structured, and learning what data may be collected during sessions ensures transparency. When families understand how VRT works, they can better evaluate safety, privacy protections, and therapeutic intent.
Families are also well-positioned to assess emotional readiness. Because immersive simulations can evoke strong emotional responses, noticing signs of anxiety, trauma sensitivity, or mood instability is important. Encouraging grounding practices and discussing reactions after sessions helps protect emotional safety. If distress appears overwhelming, families can advocate for pacing adjustments or additional clinical support.
Supporting integration with other recovery approaches keeps treatment balanced. VRT is most effective when combined with counseling, peer support, medication-assisted treatment, or family therapy. Families can help coordinate schedules, encourage consistent participation, and check in on how VRT fits into the broader recovery plan.
Ongoing encouragement and progress monitoring reinforce motivation. Listening to reflections after sessions, acknowledging effort, and celebrating small achievements strengthen confidence. Families often notice subtle improvements in emotional regulation or stress tolerance that loved ones may overlook.
Collaboration with clinicians adds another layer of protection. Participating in joint check-ins, asking about ethical safeguards, and sharing observations from home keeps care transparent and accountable. This teamwork ensures that the technology remains a therapeutic tool under professional oversight.
Finally, respecting autonomy is essential. The person in recovery must always have the final say. Families can encourage trial periods, offer support, and express confidence—while recognizing that declining or discontinuing VRT is not failure but self-awareness.
In summary, families help ensure wise decisions about Virtual Reality Therapy through empathy, education, observation, and collaboration. When loved ones feel supported rather than pushed, they can explore new treatment options safely and confidently—knowing they are not navigating recovery alone.
Community Resource Strategies for Evaluating Virtual Reality Therapy in Addiction Treatment
Virtual Reality Therapy (VRT) is rapidly emerging as a modern tool in addiction recovery, but communities play a critical role in determining whether this technology is truly appropriate, ethical, and accessible for the people they serve. Effective evaluation requires collaboration among healthcare systems, social services, recovery organizations, and public stakeholders. When communities work together, decisions about adopting VRT become grounded in shared knowledge, equity, and accountability rather than novelty alone.
Partnerships with local health agencies and recovery centers form the foundation of responsible implementation. Behavioral health boards, addiction treatment facilities, and community clinics can help assess whether VRT programs meet clinical standards and align with local populations’ needs. Case management screenings and professional evaluations ensure that individuals are matched to VR-based therapy only when it fits their diagnosis, recovery stage, and emotional readiness. Maintaining directories of evidence-based digital treatment options also helps communities avoid unverified or unsafe programs.
Interagency collaboration further strengthens decision-making. Bringing together addiction specialists, mental health clinicians, technology developers, and recovery advocates allows communities to review emerging VR tools from multiple perspectives. Shared research updates, professional workshops, and cross-sector task forces prevent misinformation and promote ethical, evidence-driven adoption of new treatment technologies.
Public education and awareness efforts reduce uncertainty and stigma surrounding technology-based therapy. Community seminars, library-based learning sessions, university partnerships, and public Q&A forums allow individuals and families to understand how VRT works, its benefits and limitations, and how it compares to traditional treatment approaches. Informed communities empower individuals to make confident treatment decisions rather than feeling pressured by trends.
Improving accessibility and funding is essential for equitable care. Because VR systems can be costly, collaborating with public health departments, nonprofit organizations, and private donors can help secure grants or access to shared equipment programs. Mobile VR units, rotating clinic resources, and subsidized pilot programs expand access to underserved or rural populations, preventing technology from deepening healthcare disparities.
Cultural and ethical inclusion also matters. Community organizations, faith groups, cultural councils, and disability advocates can provide feedback on whether VR content is respectful, trauma-informed, and representative of diverse lived experiences. Ensuring language accessibility and culturally sensitive design makes therapy more welcoming and effective for all participants.
Peer recovery specialists bring invaluable lived experience to the evaluation process. Including peers in advisory panels, pilot testing, and feedback sessions ensures VR scenarios reflect real recovery challenges. Their insight helps determine whether simulations feel supportive, realistic, or potentially triggering.
Finally, community-based evaluation systems maintain accountability. Tracking participation, outcomes, satisfaction, and reported concerns allows local health leaders to continuously refine how VRT is used. Transparent data-sharing supports policy development and long-term quality improvement.
In summary, community resource strategies ensure Virtual Reality Therapy is introduced into addiction treatment responsibly. Through collaboration, education, equitable funding, cultural inclusion, and continuous evaluation, communities can decide whether VRT is not just innovative—but truly beneficial for the people they serve.
Frequently Asked Questions
Here are some common questions:
1. What is Virtual Reality Therapy (VRT) for addiction?
Virtual Reality Therapy is a treatment approach that uses immersive computer-generated environments to help individuals practice coping with substance-use triggers. Clients wear VR headsets and enter simulated real-life situations where they learn to manage cravings and emotional responses safely under therapist guidance.
2. How does VRT help reduce cravings?
VRT exposes individuals to virtual versions of high-risk environments such as bars, parties, or stressful situations. With repeated guided practice, clients learn to regulate emotions, apply coping skills, and reduce the intensity of cravings when faced with similar real-world triggers.
3. Is Virtual Reality Therapy safe?
Yes, when conducted by trained clinicians. Therapists monitor emotional and physical responses throughout sessions. Safety measures include the ability to pause or stop simulations at any time and debrief afterward to process reactions.
4. Can VRT replace traditional addiction therapy?
No. VRT is designed to complement, not replace, evidence-based treatments such as Cognitive Behavioral Therapy (CBT), group counseling, and Medication-Assisted Treatment (MAT).
5. Who is a good candidate for VRT?
Individuals who have achieved basic emotional stability, can tolerate exposure to triggers, and are comfortable using technology often benefit most. Clinicians assess readiness before starting VR sessions.
6. Can VRT trigger cravings or emotional distress?
It can. Because simulations feel realistic, some people experience temporary cravings or anxiety. This is why therapist supervision and grounding techniques are essential parts of the process.
7. How many VRT sessions are typically needed?
There is no universal standard yet. Programs often range from 6 to 12 sessions depending on treatment goals, recovery stage, and individual response.
8. Does VRT collect personal data?
Some systems track biometric data, such as heart rate and eye movement, to measure stress responses. Ethical programs use encrypted storage and follow privacy laws to protect patient confidentiality.
9. Is Virtual Reality Therapy widely available?
Availability varies. Larger or research-based treatment centers are more likely to offer VRT. Cost and equipment needs currently limit widespread access.
10. Is there scientific evidence supporting VRT?
Early clinical studies show promising results in reducing craving and in relapse prevention. However, long-term outcome research is still developing.
11. Can VRT be used through telehealth?
Yes. Some programs offer portable VR systems that enable supervised sessions via telehealth platforms.
12. Will insurance cover VRT?
Coverage depends on the provider and state. Some programs include VRT within standard therapy billing, while others offer it as an add-on service.
13. What if someone feels uncomfortable using VR?
Participation is always voluntary. Individuals can choose traditional therapy approaches without pressure to use VR.
14. Does VRT work for all types of addiction?
VRT has been studied most in substance-use disorders such as alcohol, opioids, and nicotine. Research is expanding into behavioral addictions like gambling.
15. What is the main benefit of VRT in recovery?
The biggest benefit is practicing real-world coping skills in safe, controlled environments, which helps build confidence and relapse-prevention skills.
Conclusion
Virtual Reality Therapy offers powerful opportunities to personalize and modernize addiction recovery, transforming treatment from passive discussion to active experience. Its success, however, depends on thoughtful implementation—balancing innovation with ethics, accessibility, and emotional safety. Through strong self-management practices, families can help evaluate readiness and monitor outcomes, while communities can promote education, equity, and transparency. When guided by ethical principles and collaborative support systems, VRT becomes more than a technological tool—it becomes a bridge between science, empathy, and sustained recovery, helping individuals rewire their brains and behaviors for long-term wellness.
Video: