Combat veterans know all too well what it’s like to come home carrying not just physical scars, but deep emotional and psychological ones as well. I’ve talked with several veterans who’ve opened up about just how heavy this load can feel, especially when it’s tangled up with substance abuse. Many are surprisingly honest about the uphill battles they face, tracing the line from traumatic experiences in combat to later struggles with drugs or alcohol. Figuring out these connections is crucial for anyone hoping to support veterans or address substance use in veteran communities.
The Hidden Struggle: Why Combat Trauma Can Lead to Substance Abuse
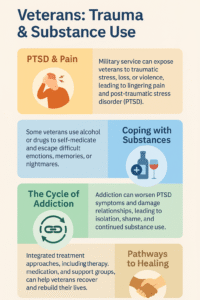
Military life—especially time spent in combat—leaves marks that aren’t just physical. Many of the veterans I’ve spoken with recall stories about blaring sirens, unpredictable environments, or profound loss that lingers long after returning home. These effects are often grouped under posttraumatic stress disorder (PTSD), but trauma comes in many shapes that don’t always fit a single label. When coping or talking about these events feels impossible, some veterans reach for alcohol, prescription drugs, or even heavier substances, hoping for relief.
This isn’t just a hunch; research backs it up. The U.S. Department of Veterans Affairs has found that about 1 in 3 veterans seeking treatment for substance use disorder also deal with PTSD (VA source). Self-medicating with drugs or alcohol may start as a way to turn down anxiety, block out nightmares, or quiet guilt. But what begins as a short-term escape can quickly spiral, leading to dependence and even more stress on mind and body.
Common Stories and Triggers Shared by Veterans
If you talk to veterans, it’s clear that substance abuse after military service is tied closely to real, raw experiences. It’s not just what happened during combat; daily life after leaving the service brings its own hurdles. Here are some of the most frequent points I hear from veterans:
- Nightmares and flashbacks: Trouble sleeping and reliving traumatic moments often push people to use substances to get some rest or to escape runaway thoughts.
- Chronic pain and injuries: Combat injuries can mean long-term prescriptions for strong pain relievers, and those medications can be addictive over time.
- Isolation and alienation: Veterans may feel a gap between themselves and civilians. Using substances can be a way to fill that emptiness or numb out difficult emotions.
- Survivor’s guilt or shame: Playing certain moments over in their minds or feeling responsible for uncontrollable events can leave veterans searching for anything that brings relief.
These triggers might burst onto the scene suddenly or show up gradually. Either way, the outcome often looks the same: substances used as a crutch, leading to more hurdles down the road.
Recognizing the Warning Signs in Everyday Life
Spotting trauma-related substance abuse isn’t always simple. Drinking or drug use can be shrugged off as “normal,” especially in social settings or high-stress environments. Still, there are warning signs that come up again and again in the stories veterans share:
- Needing more alcohol or drugs to work, relax, or get to sleep
- Drifting away from family, friends, or the things they used to enjoy
- Mood changes or irritability when not using substances
- Letting work, home, or school responsibilities slide
- Mixing several kinds of substances (like painkillers with alcohol)
Family, friends, or coworkers often notice these changes and check in. Open, honest conversations—without judgment—can make all the difference. Many veterans finally reach out once they realize that support comes without blame.
Overcoming the Stigma Around Asking for Help
One of the most challenging hurdles veterans face is the ongoing stigma attached to substance abuse and trauma. Many have been taught to keep struggles to themselves, to “tough it out” even when every day feels impossible. Worrying about future jobs or relationships makes asking for help seem risky or shameful.
But here’s what many people miss: reaching out opens more doors than it shuts. There are veteran peer groups, counselors who truly get military life, and VA-supported programs quietly creating supportive, private spaces. Many veterans describe their first group meeting as a giant weight lifted—just knowing they’re not alone changes everything.
Steps Toward Healing and Recovery
Recovery is a unique ride for each veteran, but there are a few tried and tested routes that seem to help most:
- Peer support: Connecting with others who’ve walked the same path offers understanding and keeps people accountable.
- Integrated treatment: Getting mental health and substance use treatment together works better than treating each problem alone.
- Physical activity and mindfulness: Hiking, lifting weights, or practicing yoga can relieve stress and improve focus.
- Creative outlets: Making art, writing, or playing music can help release challenging emotions safely and healthily.
- Easy access to medical care: Help from the VA or local clinics—including medication, therapy, and regular follow-ups—prevents setbacks and supports steady progress.
Setbacks happen, but they don’t spell defeat. Most veterans I know call recovery a long adventure—sometimes messy, but worth the effort at every stage.
Pitfalls and Barriers Veterans Often Face
Even with plenty of resources, major roadblocks can trip up veterans working to break the trauma-substance abuse cycle. These are some recurring issues:
- Limited local resources: Finding nearby treatment or support can be hard, especially in smaller communities.
- Delays in care: Overcrowded clinics and lengthy wait lists keep veterans from the help they need, sometimes for weeks or longer.
- Financial burdens: Juggling unemployment or difficulties transitioning from military life often means money worries—making it challenging to pay for treatment or even take time off work.
- Strained family life: Tensions at home can flare, especially if loved ones don’t understand the underlying struggles.
Getting past these hurdles requires patience, encouragement from others, and sometimes, just stumbling on the right provider or vet-friendly group. Plugging into organizations like the National Veterans Foundation or local veteran centers can smooth the way to much-needed help.
Practical Tips for Veterans and Families Navigating Recovery
Supporting a veteran through trauma and substance abuse recovery takes patience and a solid game plan. Here are tips I’ve heard repeatedly in vet circles:
- Spot triggers early: Talk about situations that crank up cravings and brainstorm healthy alternatives.
- Create daily routines: Sticking to regular meals, sleep, and social schedules lowers the risk of reverting to old habits.
- Build connections: Staying in touch makes all the difference, whether texting another vet or sharing weekly coffee with a friend.
- Educate the family: Learn about PTSD and substance use as a group, so every family member knows how to support and when to speak up if problems return.
- Celebrate every step: Mark even small milestones with encouragement—small wins help fuel progress.
Remember: what works for one veteran might not work for another. Some may try different programs before finding the right fit; others stumble upon helpful routines quickly. Flexibility is key.
Frequently Asked Questions
Question: How common is substance abuse after combat service?
Answer: Rates of substance abuse among veterans are higher than in the general population, especially among those who have gone through traumatic experiences in service, according to VA reports.
Question: What types of substances do veterans most often struggle with?
Answer: Alcohol tops the list, but many also deal with prescription painkillers, anti-anxiety medications, and sometimes street drugs. The pattern depends on a veteran’s medical needs and post-service experience.
Question: Where can veterans get confidential help?
Answer: Veterans can call the VA crisis line, connect with community groups, join veteran support hotlines, or attend peer support meetings. Confidentiality is a priority; reaching out won’t automatically affect benefits or records.
Takeaways: Supporting Veterans for the Long Haul
Combat trauma doesn’t just step aside when the fighting ends. The risk of substance abuse is very real, but it can be managed and even turned around with steady, informed support. Veterans are among the most resilient folks I’ve ever met, and while recovery isn’t always easy, open conversations and ongoing support make all the difference. Whether you are a veteran, family member, or friend, learning and listening lay the groundwork for healing—a path well worth sticking with.
Video: Why Do Veterans Struggle After War?