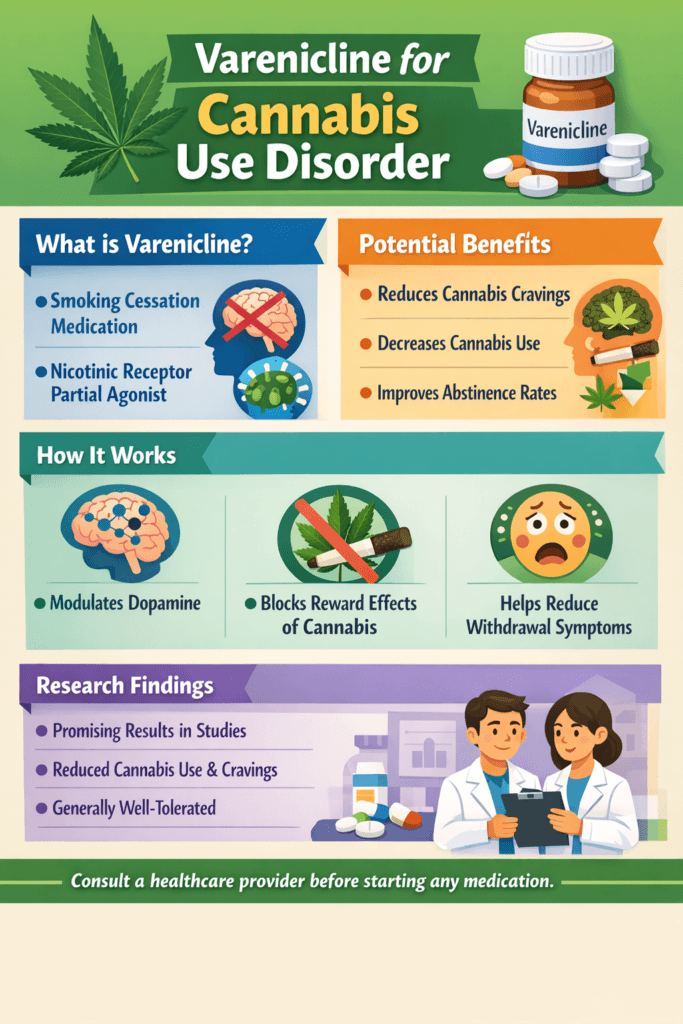
Cannabis use disorder (CUD) is an increasingly recognized public health concern as marijuana becomes more widely available, legally accessible, and socially accepted. While many individuals use cannabis without dependence, others experience cravings, withdrawal, and difficulty controlling use. Treatment has relied mainly on behavioral therapy, but varenicline, a medication originally for smoking cessation, is now being studied for its potential to reduce cannabis cravings and withdrawal by stabilizing brain reward pathways. This offers a promising new direction in CUD treatment.
Varenicline for Cannabis Use Disorder: A New Direction in Treatment Research
Cannabis use disorder (CUD) is becoming increasingly common as marijuana legalization expands and public perception shifts toward viewing cannabis as low-risk. While many individuals use cannabis without developing dependence, a significant portion experience cravings, withdrawal symptoms, tolerance, and difficulty controlling use. Until recently, treatment options for CUD relied mainly on behavioral therapies, with no FDA-approved medications available. Emerging research now suggests that varenicline — a medication originally developed for smoking cessation — may offer new promise in reducing cannabis dependence.
Varenicline works by targeting nicotinic acetylcholine receptors in the brain. These receptors play a key role in the reward pathway, influencing dopamine release and reinforcement behaviors. Although originally designed to help individuals quit tobacco, scientists discovered that these same neural pathways interact with cannabinoid reward systems. By partially stimulating these receptors while blocking stronger activation, varenicline may reduce cravings and withdrawal symptoms associated with cannabis cessation.
Early clinical trials indicate that individuals taking varenicline report fewer cannabis cravings, reduced frequency of use, and improved abstinence rates compared to placebo groups. Participants also describe decreased irritability, sleep disruption, and restlessness — common withdrawal symptoms that often lead to relapse. While research is still ongoing, these findings suggest varenicline could become an important medication-assisted treatment option for CUD in the future.
It is important to note that varenicline is not yet approved specifically for cannabis use disorder, and individuals should never self-medicate. Side effects may include nausea, vivid dreams, and mood changes, requiring medical supervision. Behavioral therapies such as cognitive-behavioral therapy, motivational enhancement, and relapse-prevention planning remain the foundation of CUD treatment, with medication serving as a potential supportive tool.
As addiction medicine continues evolving, medications like varenicline represent a shift toward evidence-based, neuroscience-informed care. Continued research may soon provide clinicians with more effective tools to help individuals regain control, reduce dependence, and build sustainable recovery from cannabis use disorder.
Self-Management Strategies for Using Varenicline in Cannabis Use Disorder Recovery
Cannabis use disorder (CUD) can lead to cravings, withdrawal symptoms, sleep disruption, irritability, and difficulty reducing use despite negative consequences. While behavioral therapies remain the foundation of treatment, emerging research suggests that varenicline — a medication originally approved for smoking cessation — may help reduce cannabis cravings and withdrawal symptoms. When prescribed by a healthcare provider, combining varenicline with self-management strategies can improve treatment outcomes and support long-term recovery.
The first key self-management strategy is medication adherence. Taking varenicline exactly as prescribed helps maintain stable receptor activity in the brain’s reward system. Many individuals benefit from setting phone reminders, using pill organizers, and pairing medication intake with daily routines, such as meals or tooth brushing. Skipping doses can reduce effectiveness and increase the risk of breakthrough cravings.
Monitoring side effects is another essential strategy. Common effects such as nausea or vivid dreams often decrease over time, but keeping a symptom journal helps individuals report concerns early to their provider. Self-awareness of mood changes is particularly important, as adjusting dosage or timing may be needed for comfort and safety.
Managing cannabis triggers remains central to recovery. Individuals can identify high-risk situations such as stress, boredom, or social environments where cannabis use is common. Developing alternative coping responses — including exercise, relaxation breathing, structured hobbies, or peer support meetings — strengthens resilience while varenicline reduces physiological cravings.
Sleep and nutrition also support treatment success. Withdrawal from cannabis may disrupt sleep patterns, so maintaining consistent bedtime routines and limiting screen exposure before bed improves stability. Balanced meals and hydration assist brain recovery and medication tolerance.
Finally, combining varenicline with behavioral therapies such as cognitive-behavioral therapy or motivational enhancement provides tools to change thought patterns and strengthen commitment to recovery. Medication reduces craving intensity, while therapy builds long-term coping skills.
Using varenicline as part of a structured self-management plan empowers individuals to take active control of their recovery. With medical supervision, consistency, and supportive lifestyle strategies, individuals can reduce cannabis dependence and move toward sustained wellness.
Family Support Strategies When Using Varenicline for Cannabis Use Disorder
Cannabis use disorder (CUD) affects not only the individual but also the family system. As treatment options evolve, varenicline — a medication originally developed for smoking cessation — is being explored as a supportive aid for reducing cannabis cravings and withdrawal symptoms. When prescribed under medical supervision, varenicline may help stabilize brain reward pathways, making it easier to reduce or stop cannabis use. However, medication alone is rarely enough. Family involvement plays a powerful role in treatment success.
One of the most effective family support strategies is encouraging medication adherence. Family members can help establish consistent routines, provide reminders when appropriate, and offer positive reinforcement for following treatment plans. Simple acts of encouragement reduce shame and increase motivation during early recovery.
Emotional support is equally important. Individuals adjusting to varenicline and cannabis reduction may experience mood changes, irritability, or sleep disruption. Families can respond with patience, active listening, and non-judgmental communication. Creating a safe environment for honest conversations helps prevent secrecy and relapse behaviors.
Families also play a role in reducing environmental triggers. Removing cannabis products from shared spaces, limiting exposure to substance-using social circles, and supporting new healthy activities strengthen recovery efforts. Participating in family activities such as exercise, shared meals, or hobby time provides alternative sources of connection and reward.
Education is another key strategy. When family members understand how varenicline works, potential side effects, and the challenges of cannabis withdrawal, they can respond more effectively. Attending family therapy or educational workshops builds shared knowledge and strengthens teamwork in recovery.
Finally, families benefit from practicing healthy boundaries. Supporting recovery does not mean controlling behavior. Encouraging independence while offering consistent support promotes confidence and long-term change.
When medication, personal commitment, and family support work together, recovery outcomes improve significantly. With understanding, structure, and compassion, families become an essential partner in healing from cannabis use disorder.
Community Resource Strategies for Supporting Varenicline Use in Cannabis Use Disorder Recovery
Cannabis use disorder (CUD) continues to rise as access to marijuana expands, yet treatment options remain limited. Varenicline, a medication originally approved for tobacco cessation, is now being studied for its ability to reduce cannabis cravings and withdrawal symptoms by stabilizing reward pathways in the brain. While medical supervision is required for varenicline use, community resources play a vital role in helping individuals stay engaged in treatment and build lasting recovery.
One of the most valuable community supports is access to addiction-informed healthcare providers. Community health clinics, primary care offices, and behavioral health centers can screen for CUD, monitor medication response, and coordinate therapy services. Expanding provider training ensures individuals receive accurate guidance and safe medication management.
Peer recovery programs also strengthen treatment success. Local recovery groups, cannabis-specific support meetings, and online peer communities provide shared understanding and accountability. Hearing success stories from others using medication-assisted strategies reduces stigma and increases hope.
Community education initiatives further support recovery. Workshops, public health campaigns, and school-based prevention programs help families and individuals understand how medications like varenicline fit into evidence-based addiction care. Knowledge reduces misinformation and encourages early help-seeking.
Employment, housing, and social service organizations also contribute to stability during treatment. Secure housing, job placement assistance, and transportation services remove practical barriers that often prevent people from attending appointments or maintaining medication routines.
Finally, integrated care networks — where medical, mental health, and social services collaborate — provide the most effective recovery environment. When individuals can access medication management, therapy, and peer support in one coordinated system, long-term outcomes improve.
Community involvement transforms recovery from an isolated struggle into a shared support system. With accessible resources, trained providers, and compassionate networks, individuals using varenicline for cannabis use disorder can achieve stronger, more sustainable recovery.
Frequently Asked Questions
Here are some common questions:
1. What is varenicline?
Varenicline is a prescription medication originally approved to help people quit smoking. It works by partially activating nicotinic acetylcholine receptors in the brain, reducing cravings and withdrawal symptoms associated with addictive substances.
2. How can varenicline help with cannabis use disorder?
Although not yet FDA-approved for cannabis use disorder, early research suggests varenicline may reduce cannabis cravings, ease withdrawal symptoms, and support abstinence by stabilizing brain reward pathways involved in addiction.
3. Is varenicline officially approved for cannabis addiction?
No. Varenicline is currently approved for tobacco cessation only. Its use for cannabis use disorder is considered off-label and should only be done under medical supervision.
4. Who might benefit from varenicline for CUD?
Individuals who experience strong cannabis cravings, repeated relapse, or withdrawal symptoms may benefit — especially when medication is combined with behavioral therapy. A healthcare provider determines suitability.
5. What are common side effects?
Possible side effects include nausea, vivid dreams, headache, insomnia, and mood changes. Most effects are mild and temporary, but any mood or behavior changes should be reported to a provider immediately.
6. Can I take varenicline while still using cannabis?
Many treatment plans begin while a person is still using cannabis, then gradually reduce use as cravings decrease. A provider will guide timing and dosage.
7. Does varenicline work on its own?
Medication works best when combined with counseling, cognitive-behavioral therapy, relapse-prevention planning, and support systems.
8. How long does treatment last?
Treatment length varies, but typical varenicline programs last 8–12 weeks, with adjustments based on progress and response.
9. Is varenicline safe for everyone?
It may not be appropriate for individuals with certain psychiatric conditions, kidney disease, or those taking specific medications. Medical screening is required.
10. What should I do if I miss a dose?
Take it as soon as remembered unless it is close to the next dose. Do not double doses. Consistency improves effectiveness.
11. Will insurance cover varenicline for CUD?
Insurance usually covers varenicline for smoking cessation. Coverage for off-label cannabis treatment depends on the plan and provider documentation.
12. Where can I learn more or find help?
Start with a primary care provider, addiction specialist, or behavioral health clinic. Many communities also offer substance-use counseling and recovery programs.
Conclusion
Although varenicline is not yet officially approved for cannabis use disorder, ongoing research suggests it may become a valuable tool in supporting recovery. When combined with behavioral therapy, self-management strategies, family involvement, and community resources, medication-assisted approaches can improve treatment engagement and reduce relapse risk. As addiction medicine continues to evolve, integrating neuroscience-based medications with psychosocial support offers renewed hope for individuals seeking freedom from cannabis dependence. With proper medical supervision, education, and support systems, recovery from cannabis use disorder becomes more achievable and sustainable.
Video: