Opioid Agonist Therapy (OAT) is a treatment for opioid use disorder that uses methadone and buprenorphine to reduce withdrawal symptoms and cravings. While OAT lowers overdose risk and enhances stability, it may lead to side effects and long-term dependency concerns. Ethical dilemmas include substituting one opioid for another and ensuring equitable access to care. Effective OAT relies on self-management strategies for active recovery, family support for emotional assistance, and community resources such as treatment facilities and peer networks to foster a supportive recovery environment.
Understanding Opioid Agonist Therapy: A Comprehensive Approach to Treating Opioid Use Disorder
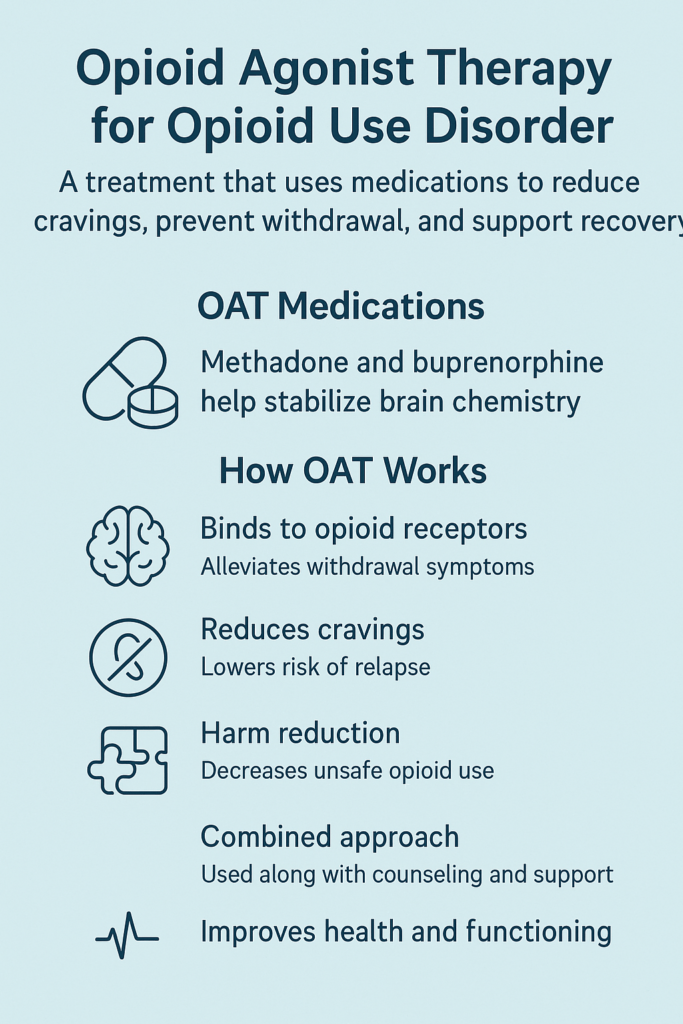
Opioid Agonist Therapy (OAT) is an effective treatment for individuals struggling with opioid use disorder (OUD). By utilizing medications known as opioid agonists, OAT aims to help individuals reduce or stop their use of harmful opioids, such as heroin or prescription painkillers. The primary medications employed in OAT are methadone and buprenorphine, both of which activate opioid receptors in the brain in a controlled and safer manner.
How OAT Works
Methadone:
Methadone is a long-acting full opioid agonist that assists individuals in managing cravings and withdrawal symptoms associated with opioid addiction. When used as prescribed, methadone provides a stabilizing effect, reducing the euphoric effects commonly experienced with other opioids, thereby allowing individuals to focus on recovery without the distraction of active addiction.
Buprenorphine:
Buprenorphine is classified as a partial opioid agonist, meaning it activates opioid receptors but to a lesser extent than full agonists like methadone. This property results in a safer profile with a significantly lower risk of overdose, making it an attractive option for many individuals in treatment.
A Comprehensive Approach to Recovery
OAT is most effective when combined with counseling and other forms of behavioral therapy, providing a holistic approach to managing opioid addiction. This combination helps to:
- Stabilize Individuals: By alleviating withdrawal symptoms and reducing cravings, OAT allows individuals to regain control over their lives and make positive changes.
- Reduce Illicit Opioid Use: With the help of OAT, individuals are less likely to seek out illicit substances, leading to decreased drug-related criminal behavior and health risks.
- Prevent Overdose: OAT lowers the chances of overdose by stabilizing opioid receptor activation and reducing the need for illicit opioid use.
- Improve Overall Quality of Life: The stabilization provided by OAT can enhance social functioning, employment, and educational engagement, enabling individuals to rebuild their lives and pursue long-term recovery.
Opioid Agonist Therapy is a vital tool in the fight against opioid use disorder. By utilizing medications like methadone and buprenorphine, OAT provides individuals with the support they need to reduce or stop harmful opioid use effectively. When paired with counseling and behavioral therapies, OAT fosters a comprehensive approach that not only addresses the physical aspects of addiction but also promotes overall well-being and a brighter future for those affected by OUD.
The Benefits of Opioid Agonist Therapy: A Path to Recovery from Opioid Use Disorder
Opioid Agonist Therapy (OAT) is a proven treatment for individuals struggling with opioid use disorder (OUD). Utilizing medications such as methadone and buprenorphine, OAT not only helps manage addiction but also offers a wide range of benefits that contribute to long-term recovery. Here are the key advantages of OAT for those facing the challenges of opioid addiction:
Critical Benefits of Opioid Agonist Therapy
- Reduces Cravings and Withdrawal Symptoms
OAT effectively manages the intense cravings and painful withdrawal symptoms associated with stopping opioids. By providing a controlled dose of a safer opioid substitute, individuals can stabilize without experiencing the discomfort that often leads to relapse. - Decreases Risk of Overdose
One of the most significant benefits of OAT is its ability to reduce the risk of overdose. By using medications like methadone or buprenorphine, which are safer alternatives to illicit opioids, individuals can avoid the dangerous highs and lows associated with street drugs. - Improves Retention in Treatment
OAT has been shown to increase the likelihood that individuals will stay in treatment programs longer. Longer retention is associated with better recovery outcomes, as individuals have more time to develop coping skills and engage in supportive therapies. - Reduces Illicit Opioid Use
With the support of OAT, many individuals can decrease or eliminate their reliance on illicit opioids. This shift not only improves their overall health but also mitigates the legal and social consequences that accompany drug use. - Promotes Physical and Mental Health
Continuous treatment with OAT enhances physical health by reducing the transmission of infectious diseases such as HIV and Hepatitis C. Additionally, the stability provided by OAT improves mental health and quality of life, enabling individuals to function more effectively in their daily lives. - Enhances Social and Occupational Functioning
OAT helps individuals regain control over their opioid use, facilitating reintegration into society. Many people find they can hold jobs, maintain relationships, and participate in daily activities more easily, contributing to a more fulfilling life. - Cost-Effective
OAT can be more cost-effective than addressing the consequences of untreated opioid addiction. The expenses related to emergency room visits, incarceration, and other medical interventions resulting from opioid misuse can far exceed the costs associated with OAT. - Harm Reduction
OAT is a crucial harm reduction strategy that provides a safer alternative to illicit opioid use. By improving health outcomes and lowering the risks associated with drug use, OAT plays an essential role in the broader strategy to combat the opioid crisis.
Opioid Agonist Therapy offers a lifeline for individuals struggling with opioid use disorder. By reducing cravings and withdrawal symptoms, lowering overdose risks, and promoting overall health and social functioning, OAT paves the way for successful recovery. As a cost-effective and harm-reduction approach, OAT not only benefits individuals but also contributes positively to communities grappling with the challenges of opioid addiction. Embracing OAT can lead to healthier, more productive lives for those affected by OUD, providing hope and a pathway to lasting recovery.
Weighing the Downsides of Opioid Agonist Therapy: Important Considerations for Recovery
Opioid Agonist Therapy (OAT) is a valuable treatment option for individuals struggling with opioid use disorder (OUD). While it provides significant benefits, it’s essential to recognize the potential disadvantages of this treatment approach. Here, we explore the challenges of OAT and help individuals and healthcare providers make informed decisions about its use.
Disadvantages of Opioid Agonist Therapy
- Dependence on Medication
OAT involves the use of opioid-based medications like methadone or buprenorphine. Although these medications are designed to be safer alternatives to illicit opioids, individuals may still develop a dependence on them for long-term management of their addiction. This ongoing reliance can raise concerns about the transition to complete sobriety. - Side Effects
Many individuals experience side effects from OAT medications, which can include constipation, drowsiness, sweating, or sexual dysfunction. These side effects can significantly impact the quality of life and deter some people from continuing treatment. - Stigma
There is a societal stigma associated with taking medications like methadone or buprenorphine, often perceived as “replacing one drug with another.” This stigma can discourage individuals from seeking treatment or staying committed to their recovery journey, leading to feelings of shame and isolation. - Access and Availability
OAT programs are not uniformly available across regions, particularly in rural or underserved areas. Regulatory barriers, a shortage of specialized clinics, and financial constraints can further limit access, making it challenging for individuals to receive the necessary treatment. - Cost
While OAT is often more cost-effective than the consequences of untreated opioid addiction, it can still be expensive for individuals, especially if not fully covered by insurance. Long-term treatment can lead to high out-of-pocket costs, creating financial strain for some patients. - Diversion Risk
Buprenorphine, a common OAT medication, has a lower but still present potential for diversion and misuse. Some individuals may sell or misuse the medication, which undermines the intended goals of treatment and poses risks to both the individual and the community. - Strict Regulations
Methadone is heavily regulated and often requires daily visits to specialized clinics for administration. This can be burdensome and inconvenient, particularly for individuals with other commitments such as work or family responsibilities. - Long-Term Commitment
OAT can require long-term, sometimes indefinite, treatment. For some individuals, the prospect of being on medication for an extended period can be daunting. Additionally, discontinuing OAT can be challenging and may lead to a return to opioid use if not carefully managed. - Inadequate Addressing of Underlying Issues
While OAT effectively manages the physical aspects of opioid addiction, it may not address the underlying psychological, social, or behavioral issues that contribute to substance use disorder. Individuals may require additional therapeutic support, such as counseling or behavioral therapy, to fully address these concerns.
Despite the challenges associated with Opioid Agonist Therapy, it remains a critical treatment option for many individuals with opioid use disorder. By understanding the disadvantages, individuals and healthcare providers can better navigate the complexities of recovery and ensure that those seeking treatment receive the comprehensive support they need. OAT can play a pivotal role in managing opioid addiction, but it’s essential to address its limitations and enhance the overall treatment experience for individuals on their journey to recovery.
Navigating Ethical Dilemmas in Opioid Agonist Therapy: A Complex Landscape
Opioid Agonist Therapy (OAT) is a vital treatment for individuals battling opioid use disorder (OUD). Yet, it is fraught with ethical dilemmas that healthcare providers, patients, and policymakers must carefully consider. These dilemmas often revolve around patient autonomy, public safety, access to care, and the complexities of individual treatment needs. Here, we explore the key ethical considerations associated with OAT and the challenges in navigating these issues.
Key Ethical Considerations in OAT
- Patient Autonomy vs. Public Safety
OAT champions patient autonomy by allowing individuals to make informed choices about their treatment. However, concerns about public safety arise, particularly regarding the potential for opioid diversion or misuse. Striking a balance between individuals’ rights to access treatment and the responsibility to ensure community safety creates ethical tensions that must be addressed. - Stigmatization of Treatment
Individuals undergoing OAT often face stigma from various sources, including healthcare providers, family members, and the broader community. This stigma can lead to feelings of shame, discouraging individuals from adhering to their treatment plans. Healthcare professionals are ethically obligated to provide non-judgmental support, which can be challenging in environments with prevalent stigma. - Access and Equity
Disparities in access to OAT raise ethical concerns regarding equity in healthcare. Not all individuals have equal access to treatment, especially in rural or underserved areas. This situation prompts questions about justice and the obligation to provide equitable care to all individuals struggling with opioid use disorder. - Informed Consent
Ensuring patients fully understand the benefits and risks associated with OAT is essential for ethical treatment. Inadequate information about treatment options can lead to uninformed decisions, undermining the principle of informed consent. Healthcare providers must prioritize clear communication to empower patients in their decision-making processes. - Long-Term Use and Dependency
OAT can lead to long-term dependence on opioid medications, which raises ethical questions about the implications for patients. Healthcare providers must consider the moral ramifications of prescribing drugs that may result in dependency, even when they are crucial for recovery. - Treatment Efficacy and Individualized Care
Not all patients respond equally to OAT, creating ethical dilemmas regarding the continuation of treatment for those who do not show improvement. Providers must balance the need for individualized care with the potential risks associated with prolonged therapy. - Diversion and Misuse
The risk of medication diversion presents ethical challenges for healthcare providers. They must navigate their responsibilities to prevent misuse while supporting patients needing OAT. This balancing act requires careful consideration and a commitment to patient-centered care. - Integration with Comprehensive Care
OAT is most effective when combined with psychosocial support and other therapeutic interventions. Ethical concerns arise when treatment focuses solely on medication, neglecting the psychological, social, or behavioral issues that contribute to substance use disorder. - Involuntary Treatment
Ethical dilemmas can arise in situations involving involuntary treatment, particularly when patients do not recognize their need for help or pose a risk to themselves or others. The principle of autonomy must be weighed against the potential necessity of intervention for the greater good. - Resource Allocation
Limited resources for addiction treatment raise ethical questions about how to allocate these resources fairly and effectively among individuals with varying needs. Policymakers and healthcare providers must grapple with the challenge of ensuring equitable access to care while addressing resource constraints.
Navigating the ethical dilemmas associated with Opioid Agonist Therapy requires a thoughtful and compassionate approach that prioritizes patient-centered care. By fostering informed decision-making and promoting equitable access to treatment options, healthcare providers and policymakers can work to ensure that individuals struggling with opioid use disorder receive the comprehensive support they need for recovery. Addressing these ethical considerations is crucial for building a more just and effective healthcare system that truly serves the needs of all patients.
Empowering Recovery: Self-Management Strategies for Individuals in Opioid Agonist Therapy (OAT)
Self-management strategies play a critical role in enhancing the effectiveness of Opioid Agonist Therapy (OAT) and supporting long-term recovery for individuals with opioid use disorder (OUD). By actively participating in their treatment, individuals can regain control over their lives, boost their physical and mental health, and reduce the risk of relapse. Below are critical self-management strategies that can significantly improve recovery.
Effective Self-Management Strategies in OAT
- Education and Understanding
- Learn About OAT: Knowledge is power in recovery. Understand how OAT works, whether methadone or buprenorphine is prescribed, and be aware of their benefits and possible side effects. For example, understanding how buprenorphine minimizes the risk of overdose can provide peace of mind and confidence in the treatment.
- Recognize Triggers: Identify triggers that may lead to cravings or relapse, such as stress, specific environments, or social groups. For instance, in regions like Appalachia, where opioid addiction rates have soared, community-specific factors like economic stress may be common triggers. Working with a therapist to address these triggers can help develop personalized strategies to avoid relapse.
- Goal Setting
- Set Realistic Goals: Recovery is a journey, not a race. Start by setting achievable goals—such as attending all OAT appointments for a month or reducing the use of any non-prescribed substances. Longer-term goals might include rebuilding relationships or returning to work.
- Monitor Progress: Keeping a journal can be a helpful way to track your progress. Small victories, like declining an offer to use opioids, are steps worth celebrating.
- Healthy Lifestyle Choices
- Nutrition: Maintaining a balanced diet supports overall health. Eating nutrient-rich foods can improve energy levels and mental clarity. Simple shifts like replacing fast food with home-cooked meals can make a big difference.
- Exercise: Engaging in physical activity, whether walking around the neighborhood or joining a local gym, boosts mood and reduces stress. Physical activities like hiking or yoga are accessible ways to incorporate fitness into your routine.
- Sleep Hygiene: Sleep is critical for mental and physical recovery. Establishing a regular sleep schedule and creating a peaceful bedtime routine can improve overall health. Avoiding screens before bed or using relaxation techniques may improve sleep quality.
- Stress Management
- Mindfulness and Meditation: Practicing mindfulness or meditation can help reduce anxiety and increase emotional control. These techniques can be as simple as taking 5 minutes daily to breathe deeply and focus on the present.
- Relaxation Techniques: Techniques like progressive muscle relaxation or deep breathing can calm the mind and body. Incorporating these strategies into daily routines can provide relief for those dealing with stress from family or job challenges.
- Social Support
- Engage with Support Networks: Connecting with supportive family members, friends, or community groups can be a source of strength. In many Native American communities, recovery programs integrate traditional practices, such as talking circles, which can foster both connection and healing.
- Participate in Peer Support: Peer support groups like Narcotics Anonymous (NA) offer a non-judgmental space to share experiences and gain encouragement from others on the same path.
- Medication Adherence
- Follow Prescriptions: Sticking to your prescribed OAT regimen is essential. Use smartphone apps like “Medisafe” to remind you to take your medication on time.
- Utilize Reminders: Daily reminders, whether on your phone or written in a planner, can help ensure you don’t miss doses, especially if you have a busy schedule.
- Coping Skills Development
- Develop Healthy Coping Mechanisms: Cravings and stress can be overwhelming. Instead of turning to opioids, focus on healthy coping strategies such as physical activity, creative hobbies, or spending time with loved ones.
- Avoid High-Risk Situations: Stay away from places or people associated with past drug use. For instance, individuals living in densely populated urban centers like New York may find it helpful to map out “safe zones” where they feel less tempted or pressured.
- Seek Professional Help
- Engage in Counseling: Therapy can help you address underlying psychological issues that contribute to opioid use. In therapy, cognitive-behavioral techniques may help reframe negative thought patterns.
- Regular Check-Ins: Follow-ups with healthcare providers allow you to adjust treatment plans as needed, ensuring your treatment meets your needs.
- Self-Advocacy
- Communicate Needs: Be proactive in discussing any issues with your medication, emotional state, or treatment plan with healthcare providers. If you experience side effects, speak up.
- Research Resources: Staying informed about new treatment options and resources, such as state-specific programs (e.g., in California, Medi-Cal offers addiction treatment services), can help you make empowered decisions about your care.
- Personal Reflection
- Self-Assessment: Regularly reflecting on your journey helps you evaluate what’s working and where you might need to make changes. Recovery is rarely linear, and understanding setbacks as part of the process is crucial.
- Emotional Awareness: Learning to recognize early signs of emotional distress—feeling overwhelmed, anxious, or disconnected—allows for timely intervention, such as seeking support from friends or professionals.
By adopting these self-management strategies, individuals in OAT can take control of their recovery, enhance treatment outcomes, and ultimately improve their quality of life. Each step forward is integral to the healing process, and with the right strategies in place, long-term recovery is within reach.
The Power of Family Support in Opioid Agonist Therapy (OAT)
Family support is a critical component for individuals undergoing Opioid Agonist Therapy (OAT) for opioid use disorder (OUD). The journey to recovery can be challenging, and having a solid support system can significantly enhance treatment outcomes. Here are some effective strategies that families can adopt to support their loved ones during OAT.
Effective Family Support Strategies for Individuals in OAT
- Education and Understanding
- Learn About OAT: Family members should take the time to educate themselves about Opioid Agonist Therapy, including how it works and the benefits it offers for treating OUD. Understanding the medications used, such as methadone and buprenorphine, can empower families to provide informed support.
- Understand the Recovery Process: Familiarity with it is essential. Family members should recognize the challenges and milestones of recovery, including the importance of medication adherence and potential side effects.
- Open Communication
- Foster a Supportive Environment: Create a safe space for open dialogue where individuals feel comfortable sharing their feelings, experiences, and challenges during treatment. This supportive atmosphere encourages honesty and vulnerability.
- Active Listening: Practice active listening to understand the individual’s needs and concerns without judgment. This fosters a sense of trust and support, making it easier for them to express themselves.
- Encouragement and Motivation
- Offer Emotional Support: Provide consistent encouragement and positive reinforcement throughout the recovery journey. This emotional backing can boost morale and confidence.
- Celebrate Achievements: Acknowledge and celebrate milestones, no matter how small. Recognizing progress reinforces motivation and shows family members are invested in their loved one’s recovery.
- Involvement in Treatment
- Attend Appointments: When appropriate, accompany the individual to therapy sessions or medical appointments. This involvement demonstrates active participation in their recovery process and can enhance accountability.
- Participate in Family Therapy: If recommended, engage in family therapy sessions to address family dynamics, improve communication skills, and strengthen relationships. This can benefit both the individual in treatment and their family members.
- Setting Boundaries
- Establish Healthy Boundaries: Set clear, healthy substance-use boundaries to ensure the individual understands family expectations. Boundaries can help maintain a healthy environment.
- Avoid Enabling Behaviors: Refrain from behaviors that may enable substance use, such as providing financial support for drugs or covering up negative consequences. Instead, focus on supporting recovery.
- Practical Support
- Assist with Daily Responsibilities: Offer help with daily tasks, such as household chores, meal preparation, or transportation to appointments. This reduces stress and allows the individual to focus on their recovery.
- Financial Guidance: Help manage finances, especially if the individual faces economic challenges due to their condition. Helping with budgeting can alleviate financial stress.
- Promotion of Healthy Lifestyle Changes
- Encourage Healthy Habits: Support healthy lifestyle changes, such as regular exercise, balanced nutrition, and adequate sleep. These habits can positively impact both recovery and overall well-being.
- Engage in Activities Together: Participate in enjoyable, constructive activities to reinforce positive behavior and strengthen family bonds. Shared experiences can create lasting memories.
- Empowerment and Respect
- Support Autonomy: Involve the individual in decision-making regarding their treatment plan, respecting their preferences and empowering them to take an active role in their recovery.
- Avoid Judgment: Approach the individual with empathy and understanding, clarifying criticism or negative comments about past behavior or challenges. This respectful approach fosters a positive atmosphere.
- Encourage Self-Care
- Promote Self-Care Practices: Encourage family members to prioritize their self-care, recognizing that supporting someone in recovery can be emotionally taxing.
- Seek Support for Themselves: Family members can benefit from their own support groups or counseling. Processing their feelings and learning coping strategies is vital for maintaining their well-being.
By actively implementing these family support strategies, families can create a nurturing environment that fosters recovery and enhances the effectiveness of Opioid Agonist Therapy. Such an environment not only supports the individual in their treatment journey but also improves the overall well-being of the entire family. With education, open communication, and a commitment to healthy practices, families can play a pivotal role in recovery.
Strengthening Recovery: Community Resource Strategies for Opioid Agonist Therapy (OAT)
Community resource strategies are crucial for supporting individuals undergoing Opioid Agonist Therapy (OAT) and enhancing their recovery journey. These strategies create a supportive environment, promote access to care, and address the social determinants of health that affect recovery. Here are some effective community resource strategies designed to bolster the success of OAT.
Effective Community Resource Strategies for OAT
- Access to Treatment Facilities
- Establish OAT Clinics: Ensure the availability of specialized clinics that provide Opioid Agonist Therapy, counseling, and comprehensive addiction treatment services. These clinics should be easily accessible to those in need.
- Integrate Services: Create integrated care models offering OAT alongside mental health and primary care services. This holistic approach improves overall health outcomes and facilitates coordinated care.
- Education and Awareness Programs
- Community Workshops: Organize workshops to educate community members about OAT, its benefits, and the importance of treating opioid use disorder (OUD). This can help reduce stigma and increase understanding.
- School and Workplace Programs: Implement educational programs in schools and workplaces to raise awareness about opioid addiction and recovery resources and foster a culture of support and understanding.
- Support Groups and Peer Networks
- Facilitate Support Groups: Create peer-led support groups for individuals in OAT to share experiences, challenges, and successes. These groups foster a sense of community and belonging, which is vital for recovery.
- Online Support Platforms: Establish online forums and virtual support groups to connect individuals who may face barriers to attending in-person meetings, ensuring that support is accessible regardless of location.
- Counseling and Mental Health Services
- Expand Access to Counseling: Collaborate with local counseling centers to provide affordable mental health services, including therapy and behavioral counseling specifically for individuals in OAT.
- Telehealth Services: Offer telehealth options for counseling and therapy sessions to increase accessibility for individuals in remote or underserved areas and to make it easier for them to receive the support they need.
- Health Promotion and Wellness Programs
- Physical Activity Initiatives: Promote fitness and wellness programs, such as yoga classes or exercise groups, that support physical and mental health and aid recovery.
- Nutrition Workshops: Provide workshops on nutrition and healthy eating habits to assist recovery and improve overall well-being, emphasizing the connection between diet and mental health.
- Substance Use Prevention and Harm Reduction Initiatives
- Prevention Campaigns: Launch community campaigns aimed at preventing opioid misuse and educating the public about the risks associated with substance use, fostering a proactive approach to addiction.
- Harm Reduction Services: Implement harm reduction strategies, such as syringe exchange programs and naloxone distribution, to mitigate the risks associated with opioid use, ensuring that safety is prioritized.
- Collaboration with Social Services
- Coordinate with Social Service Agencies: Work with social services to address issues such as housing instability, unemployment, and access to healthcare, which can significantly impact recovery efforts.
- Legal Aid Services: Partner with legal aid organizations to assist individuals facing legal issues related to addiction, ensuring they receive holistic support that addresses all facets of their recovery.
- Cultural Competence and Language Access
- Culturally Sensitive Services: Ensure that OAT services are culturally competent and tailored to meet the diverse needs of community members, recognizing that different cultures may have unique approaches to health and recovery.
- Language Support: Provide translation and interpretation services to improve access for non-English-speaking individuals seeking treatment and enhance inclusivity in community resources.
- Peer Outreach and Community Engagement
- Train Peer Navigators: Develop programs that train individuals with lived experience to serve as peer navigators, helping others access OAT and community resources and thereby promoting a sense of solidarity.
- Community Events: Organize health fairs and community outreach activities to raise awareness about OAT and connect individuals with available resources, fostering community involvement and support.
- Evaluation and Feedback Mechanisms
- Assess Community Needs: Conduct regular assessments to understand the community’s needs regarding opioid use disorder and the effectiveness of OAT programs. This data-driven approach allows for informed decision-making.
- Feedback Loops: Establish channels for individuals in OAT to provide feedback on community resources, thereby improving services and addressing gaps in support.
By implementing these community resource strategies, communities can significantly enhance support for individuals undergoing Opioid Agonist Therapy. Promoting access to care, improving overall health, and addressing the social determinants of health can lead to better treatment outcomes and a more supportive environment for recovery. We can help individuals navigate their recovery journeys more effectively through education, collaboration, and community engagement.
Frequently Asked Questions
Here are some common questions:
Is OAT replacing one addiction with another?
No. OAT is a medical treatment that reduces harm and restores stability. It does not produce the highs and lows associated with addiction when taken as prescribed.
How long do people stay on OAT?
Treatment duration varies. Some individuals benefit from long-term or lifelong treatment, while others taper gradually under medical supervision. There is no fixed timeline.
What medications are used in OAT?
The most common medications are methadone and buprenorphine. Both are effective, and the choice depends on medical history, access, and individual needs.
Is OAT safe?
When properly prescribed and monitored, OAT is safe and effective. It significantly reduces the risk of fatal overdose and improves overall health outcomes.
Can someone function normally while on OAT?
Yes. Most people on OAT can work, care for family, and engage fully in daily life. Many report improved stability and quality of life.
Conclusion
Opioid Agonist Therapy (OAT) is a critical component in addressing opioid use disorder, offering significant advantages such as reduced cravings, decreased overdose risk, and improved quality of life. However, it is essential to acknowledge the disadvantages and ethical dilemmas associated with OAT, including concerns about dependency and equitable access to treatment. Effective implementation of OAT requires robust self-management strategies that empower individuals to take charge of their recovery, alongside strong family support that fosters understanding and encouragement. Moreover, community resource strategies are vital for creating a support network and providing access to necessary treatments and services. By integrating these elements, we can enhance the efficacy of OAT and promote sustainable recovery for individuals struggling with opioid use disorder.
Video: The Gold Standard Treatment Actually Works #opioids #recovery