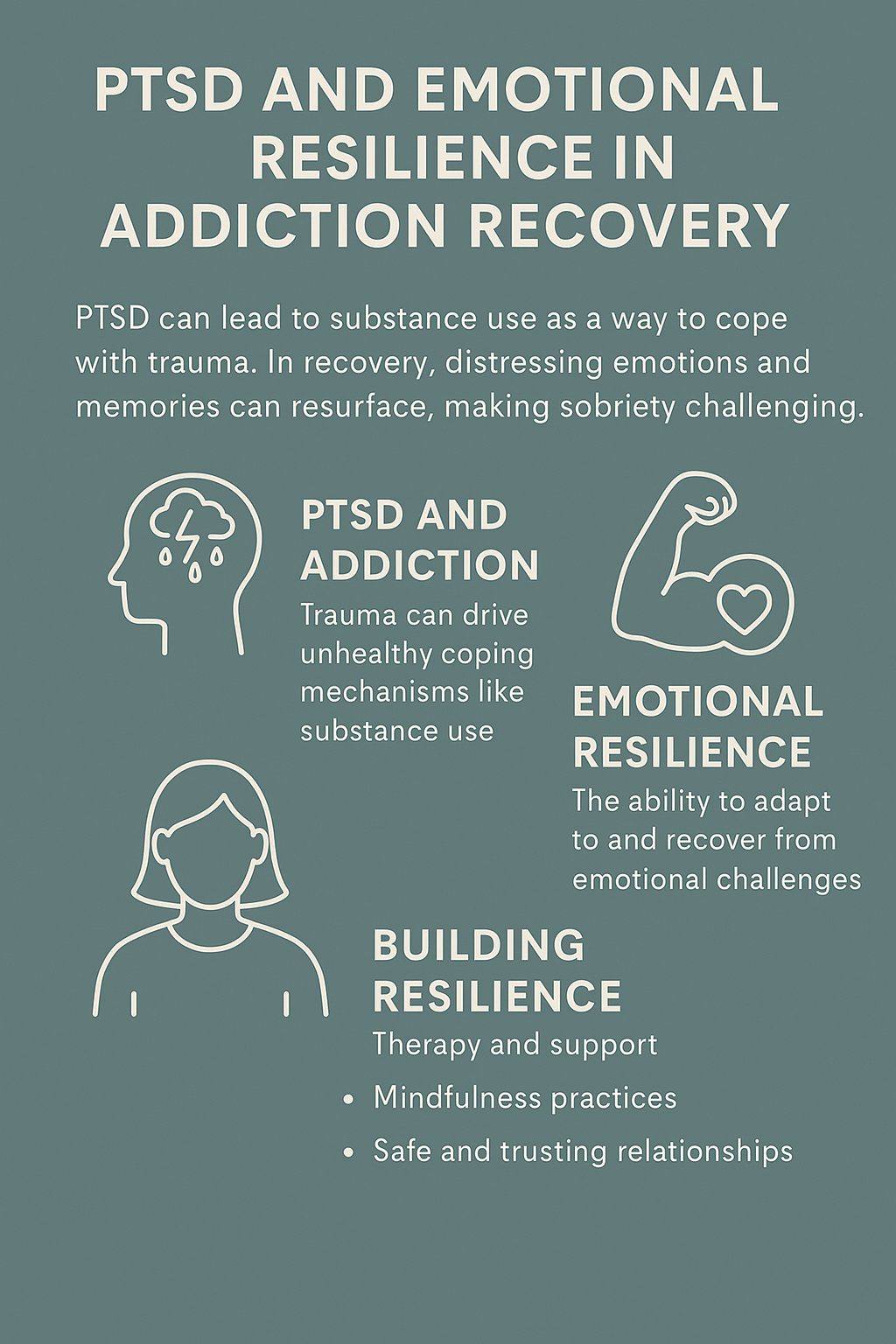
Living with PTSD and addiction can feel like fighting two battles at once—one in your mind and one in your body. The constant waves of anxiety, flashbacks, or emotional numbness can drive a person to seek relief in substances, creating a cycle that’s hard to break. However, emotional resilience—the ability to adapt, heal, and move forward—can be a powerful tool in the recovery process. I’ve seen how understanding the deep connection between trauma and substance use helps people find compassion for themselves instead of shame. Recognizing that addiction often begins as a way to cope with pain opens the door to healthier ways of managing emotions. Through therapy, support groups, mindfulness, and honest connection, it’s possible to rebuild stability and strength. If you’re trying to understand how PTSD and addiction overlap—or want guidance on how to bounce back—I’ve gathered practical insights and supportive strategies to help you or someone you love start that journey toward healing.
What is PTSD and How Does It Connect to Addiction?
PTSD (post-traumatic stress disorder) often follows a traumatic event, like an accident, abuse, or witnessing something terrifying. Symptoms can last for months or even years, showing up as flashbacks, nightmares, anxiety, or feeling stuck in survival mode. You might notice changes in mood, trouble sleeping, or a low sense of self-worth.
People sometimes turn to drugs or alcohol as a way to numb the pain or quiet their minds. While this short-term relief may seem helpful, it often exacerbates the problem. Substance use might offer a break from difficult memories, but it usually deepens the cycle of trauma and addiction. Recent research shows that about half of those seeking help for substance use disorder also meet the criteria for PTSD (source).
Understanding Emotional Resilience in Addiction Recovery
Emotional resilience isn’t about pretending that things don’t hurt. It’s really about adapting to stress, facing hard feelings, and bouncing back from setbacks without giving up. For people with PTSD and addiction, growing resilience means learning new ways to cope with triggers and building healthier habits over time.
I’ve noticed that resilience appears in different forms for each person. It might involve reaching out for help, practicing mindfulness, or connecting with supportive people. Even small steps can make a real impact on how you feel stronger and more hopeful during recovery.
Common Triggers and Their Impact on Recovery
Noticing and understanding triggers is one of the key steps to managing both PTSD and substance use challenges. These triggers can exist out in the world or within your own thoughts and feelings. Here are some of the most common ones:
- Anniversaries of trauma: Dates or seasons that bring up memories of past events
- Social situations: Crowds, loud places, or routines that feel tough to handle
- Loneliness or boredom: Empty time can cause your mind to get stuck on the past
- Difficult emotions: Uncomfortable feelings like guilt, shame, or anger
When these triggers show up, it can be tough to resist old habits or cravings. Starting to notice your own patterns helps you plan and protect your progress.
Building Emotional Resilience: Practical Everyday Strategies
Building up resilience is an ongoing process. Here are some ways many people facing PTSD and addiction have built their recovery skills:
- Self-awareness: Keeping a journal or using mood-tracking apps can help you identify patterns in your feelings and experiences.
- Grounding techniques: Simple methods, such as focusing on your breath, naming objects around you, or immersing yourself in cold water, can help you stay present.
- Social connections: Reaching out to friends, joining support groups, or spending time with pets can help you better handle challenging emotions. If you’re unsure where to start, please refer to the peer support resources listed below.
- Healthy habits: Getting enough sleep, incorporating regular physical activity, and eating balanced meals all help establish a strong foundation for recovery. The basics really matter when things get tough.
- Mindfulness and relaxation: Meditation, yoga, and deep breathing exercises help calm your nervous system and improve your stress tolerance over time.
- Setting boundaries: Learning how to say “no” and managing your exposure to triggers gives essential protection to your mental health and sobriety.
Things to Think About When Facing PTSD and Addiction
Managing PTSD and addiction at the same time brings its own set of challenges. These are some points to consider as you look for a solid recovery plan:
- Treatment options: Integrated care—where both PTSD and addiction are treated together—often works better than dealing with each one separately. Ask about trauma-informed therapies like EMDR, trauma-focused CBT, and group counseling.
- Medication support: Some people benefit from medications prescribed by a mental health provider who understands both PTSD and addiction recovery.
- Relapse risks: Setbacks are common. Remember, relapse isn’t a sign of failure but rather a signal to try a new approach or strategy. Learning from the experience is what counts.
- Stigma: Shame and social pressures can complicate recovery. Finding groups or spaces that feel safe and nonjudgmental really lightens this load.
- Your unique pace: Healing isn’t a race; it’s a deeply personal process. Give yourself time and avoid comparing your progress to others. Every step forward matters.
Common Barriers and How to Tackle Them
The path to recovery from PTSD and addiction is rarely smooth. These are typical hurdles, along with some tactics others have found helpful:
- Powerful cravings: Urges to use substances can spike under stress or after trauma reminders. Having a support person or getting some fresh air can help break the urge.
- Flashbacks or nightmares: These make it tough to stay grounded. Preparing calming tools or playlists now helps when you’re caught off guard later.
- Feeling isolated: Pulling away from others may feel easier during rough patches, but reaching out to even one supportive contact makes a difference.
- Expecting quick fixes: Wanting instant results is tempting, but real change happens step by step. Celebrate all progress—big and small—to keep motivation up.
Advanced Tips to Strengthen Emotional Resilience
Once the basics feel more under control, consider these ideas to deepen resilience and feel even more confident in your recovery:
Practicing self-compassion: Speak kindly to yourself when things get tough. Encouraging words and self-affirmation can enhance emotional resilience, enabling you to recover more quickly from setbacks.
Making routines fit your lifestyle: Not everyone enjoys journaling—maybe art, music, or outdoor activities help you process best. Personalize your routines to fit what works for you.
Setting up a crisis plan: Writing down steps and resources for challenging moments (like hotlines, supportive friends, or favorite distractions) can bring peace of mind when stress runs high.
Widening your support network: Get involved in peer recovery groups or trauma support lines to build stronger connections and accountability. Find options through resources like The National Center for PTSD and SAMHSA’s helpline.
Everyday Tools That Help with PTSD and Addiction
Every day, support tools can make a real difference. Keep these options ready for when you need them most:
- 5-4-3-2-1 Grounding Exercise: Refocus during challenging moments by naming five things you see, four things you feel, three things you hear, two things you smell, and one thing you taste. It’s simple but powerful.
- Quick self-checks: Set a reminder to pause once or twice daily. Breathe deeply, notice your mood, and consider what you need at this moment.
- Resource cards: Write out top coping strategies or emergency numbers on cards for easy access.
- Connection reminders: These could be a supportive text message, a favorite photo, or easy access to your go-to support app.
Frequently Asked Questions
Here are some questions people often have about PTSD, addiction, and resilience building:
Question: Is it common to have both PTSD and an addiction?
Answer: Yes. People with PTSD are more likely to struggle with substance use. Receiving help that addresses both aspects makes recovery more manageable and effective.
Question: What are the best first steps for tackling both issues?
Answer: Start by finding a provider who recognizes dual diagnosis—meaning care for both PTSD and addiction at once. Peer support groups and trauma-focused therapy are also highly recommended.
Question: How long does it take to build emotional resilience?
Answer: It’s a gradual process. Small daily actions—such as checking in with yourself and reaching out—eventually lead to more significant changes in how you cope.
Final Thoughts
Getting honest about the relationship between PTSD and addiction can give you new insight into what’s happening and what might help. Building emotional resilience means adding new tools to your recovery toolkit, making tough times more bearable and the good times even sweeter. Support from trusted people, routines that fit your life, and practical coping skills lighten the load and make progress possible. If you or someone you love is seeking support, trauma-informed care, or looking to connect with others who understand, this is a strong place to start. Every single effort counts on the path towards healing.
Video: Why Do PTSD and Addiction Go Together?