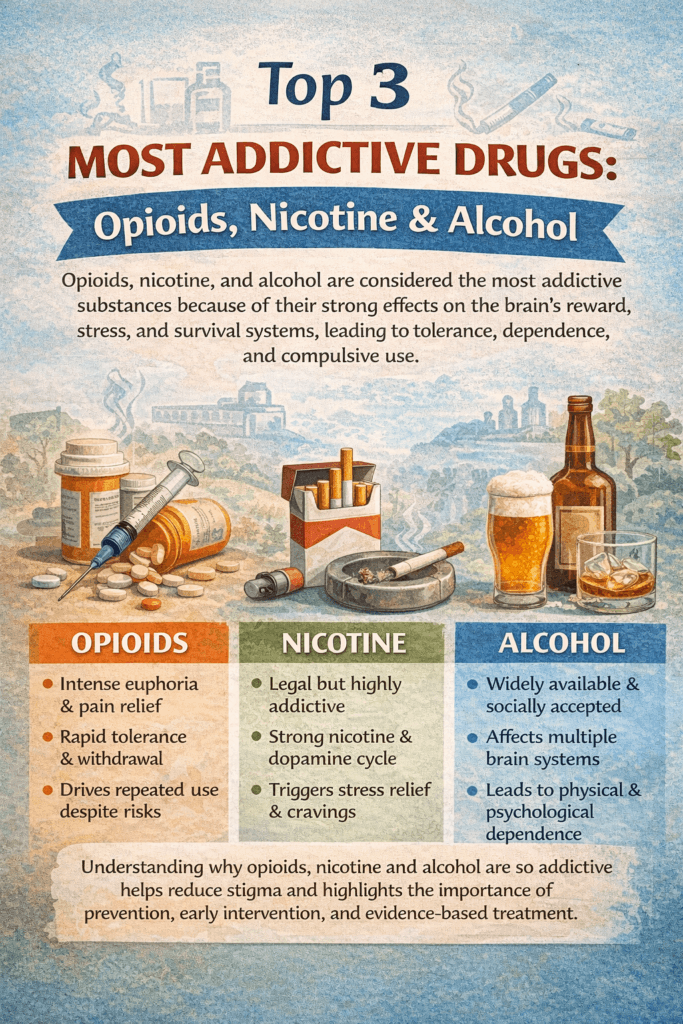
Opioids, nicotine, and alcohol are widely recognized as the three most addictive substances due to their powerful effects on the brain’s reward, stress, and dependence systems. Despite differences in legality and social acceptance, each substance can rapidly lead to tolerance, cravings, and compulsive use. Understanding why these drugs are so addictive helps shift the conversation away from blame and toward awareness, prevention, and effective support.
Top 3 Most Addictive Drugs: Opioids, Nicotine, and Alcohol
Addiction is driven by how powerfully a substance affects the brain’s reward, motivation, and stress systems. While many drugs can be habit-forming, opioids, nicotine, and alcohol consistently rank among the most addictive substances due to their widespread availability, strong effects on brain chemistry, and the severity of dependence and withdrawal they produce. Each of these substances alters the brain in distinct ways, but all can lead to compulsive use that is difficult to stop without support.
Opioids are often considered the most addictive class of drugs. They include prescription pain medications as well as illicit substances and work by binding to opioid receptors in the brain, producing intense relief, euphoria, and emotional numbing. Over time, the brain adapts by reducing its natural opioid production, leading to tolerance and physical dependence. Withdrawal symptoms—such as severe pain, nausea, anxiety, and cravings—can be overwhelming, driving continued use. The combination of powerful euphoria and painful withdrawal makes opioids especially difficult to quit without medical treatment.
Nicotine is one of the fastest-acting and most reinforcing addictive substances. It reaches the brain within seconds, stimulating dopamine release while reducing stress and increasing focus. Although the immediate effects may seem mild compared to other drugs, nicotine’s frequent use throughout the day rapidly strengthens dependence. Withdrawal symptoms like irritability, anxiety, restlessness, and difficulty concentrating make quitting challenging. Its legal status and social normalization further reinforce long-term addiction.
Alcohol is another highly addictive substance, despite its cultural acceptance. Alcohol affects multiple brain systems, including reward, inhibition, and stress regulation. Repeated use leads to tolerance, requiring more alcohol to achieve the same effect. Dependence develops as the brain adapts to alcohol’s presence, and withdrawal can range from anxiety and tremors to seizures and life-threatening complications. Because alcohol is widely available and socially encouraged, problematic use often goes unnoticed until significant harm occurs.
What makes opioids, nicotine, and alcohol especially addictive is not just their chemical impact, but their integration into daily life—through pain management, stress relief, social rituals, or routine habits. Addiction to these substances is not a moral failure, but a predictable biological and behavioral response to repeated exposure.
Understanding why these three substances are so addictive helps reduce stigma and emphasizes the need for prevention, early intervention, and evidence-based treatment. With medical care, behavioral support, and strong social and community resources, recovery from even the most addictive substances is possible.
Top 3 Most Addictive Drugs: Opioids, Nicotine, and Alcohol — Self-Management Strategies to Avoid Abuse
Among all substances, opioids, nicotine, and alcohol consistently rank as the three most addictive due to how powerfully they affect the brain’s reward, stress, and survival systems. While each substance works differently, they share a common ability to create tolerance, dependence, and compulsive use. Understanding their addictive nature—and learning practical self-management strategies—can help reduce the risk of misuse and long-term harm.
Opioids are highly addictive because they directly activate opioid receptors that control pain relief, pleasure, and emotional regulation. Over time, the brain reduces its natural opioid production, leading to tolerance and intense withdrawal symptoms such as pain, anxiety, nausea, and cravings.
Self-management strategies include using medications only as prescribed, avoiding dose escalation without medical guidance, tracking pain and emotional triggers, and using non-opioid pain management tools such as physical therapy, relaxation techniques, movement, and behavioral coping skills. Early communication with healthcare providers is essential to prevent dependence.
Nicotine is one of the most rapidly reinforcing substances. It elicits rapid dopamine release while temporarily reducing stress and improving focus, thereby encouraging frequent, repeated use. Withdrawal symptoms—irritability, restlessness, anxiety, and difficulty concentrating—often drive continued use.
Self-management strategies focus on breaking habitual patterns. These include identifying trigger routines (such as stress, driving, or social cues), using nicotine replacement or tapering strategies when appropriate, practicing stress-management skills, and replacing nicotine use with healthier habits like walking, breathing exercises, or hydration.
Alcohol affects multiple brain systems at once, including reward, inhibition, and stress regulation. With repeated use, tolerance develops, and the brain becomes dependent on alcohol to maintain balance. Withdrawal can be physically dangerous, making alcohol especially risky when misused.
Self-management strategies include setting clear limits on drinking, scheduling alcohol-free days, tracking intake, avoiding high-risk situations, and developing alternative coping strategies for stress, boredom, or social pressure. Removing alcohol from the home and prioritizing sleep, nutrition, and routine also reduces risk.
Across all three substances, effective self-management shares common principles: awareness, planning, routine, and support. Recognizing early warning signs, preparing for high-risk situations, and building healthier coping skills reduce reliance on substances as emotional or physical regulators. Self-management does not mean handling addiction alone—it means taking proactive steps while using medical, social, and community support when needed.
Ultimately, opioids, nicotine, and alcohol are not addictive because of weak willpower, but because of how they alter the brain over time. By applying intentional self-management strategies early, individuals can reduce the risk of abuse, protect their long-term health, and maintain greater control over their well-being.
Top 3 Most Addictive Drugs: Opioids, Nicotine, and Alcohol — Family Support Strategies to Prevent Abuse
Opioids, nicotine, and alcohol are widely recognized as the three most addictive substances due to how strongly they affect the brain’s reward, stress, and dependence systems. While these substances differ in form and social acceptance, all can quietly progress from use to misuse and addiction. Families play a critical role in preventing abuse by shaping environments, communication patterns, and coping behaviors long before substance use becomes severe.
Opioids often enter families through legitimate medical use, making early family involvement especially important. Family support strategies include learning about prescription safety, proper dosing, and the risks of long-term use. Families can encourage open conversations about pain, stress, and emotional well-being rather than focusing only on medication use. Monitoring prescriptions, safely storing medications, and disposing of unused opioids reduce access and misuse. Supportive check-ins help identify early warning signs such as increased reliance, mood changes, or withdrawal from daily activities.
Nicotine dependence is frequently driven by habit, stress relief, and social normalization. Families can support prevention by modeling tobacco-free lifestyles and having honest discussions about how nicotine affects the brain and body. Encouragement, rather than criticism, is key. Families can help by identifying shared stressors, supporting healthier coping strategies, and reinforcing progress during quit attempts. Reducing exposure to nicotine products in the home and celebrating small milestones strengthens motivation and confidence.
Alcohol is often the most challenging substance for families because of its cultural acceptance. Family strategies focus on setting clear expectations around alcohol use, especially during gatherings and stressful times. Creating alcohol-free activities, limiting alcohol availability at home, and modeling balanced coping skills send powerful messages. Families can also address underlying stress, trauma, or mental health challenges that may contribute to drinking, rather than focusing solely on alcohol itself.
Across all three substances, effective family support relies on education, communication, and boundaries. Families that understand addiction as a health issue—not a moral failure—are better equipped to respond with empathy and consistency. Open dialogue reduces secrecy, while clear boundaries promote accountability without shame. Encouraging professional help when concerns arise further strengthens prevention efforts.
Ultimately, family support strategies to prevent abuse of opioids, nicotine, and alcohol emphasize connection over control. When families create safe environments, model healthy coping, and respond early to risk, they become a powerful protective factor. These supportive dynamics can significantly reduce the likelihood of substance abuse and promote long-term health and resilience for everyone involved.
Top 3 Most Addictive Drugs: Opioids, Nicotine, and Alcohol — Community Resource Strategies to Prevent Abuse
Opioids, nicotine, and alcohol are widely recognized as the three most addictive substances due to their powerful effects on the brain’s reward and stress systems, combined with broad availability and social normalization. Preventing abuse of these substances requires more than individual effort—it depends on strong, accessible community resources that reduce risk, promote early intervention, and support long-term health.
For opioids, community strategies focus on prevention, safety, and treatment access. Prescription monitoring programs, safe prescribing education, and medication take-back events reduce misuse and diversion. Community health centers that integrate pain management, behavioral health, and medication-assisted treatment make early help more accessible. Overdose prevention initiatives, including education and emergency response resources, save lives and create pathways to recovery rather than punishment.
Nicotine prevention relies heavily on public health and community-based efforts. Tobacco-free policies in schools, workplaces, and public spaces reduce exposure and normalize healthier behavior. Community education campaigns, youth prevention programs, and accessible cessation services—including counseling and quitlines—help individuals avoid initiation and support quitting. Reducing marketing exposure and increasing access to evidence-based cessation tools strengthens community-wide protection.
For alcohol, effective community strategies include education, healthcare screening, and environmental approaches. Community-based screening and brief interventions in primary care identify risky use early. Public awareness campaigns challenge the normalization of excessive drinking, while alcohol-free community events provide inclusive alternatives. Policies that support responsible sales practices and reduce high-risk availability help lower alcohol-related harm without stigmatizing individuals.
Across all three substances, peer support and recovery services are essential. Recovery community organizations, peer coaches, and support groups reduce isolation and provide accountability grounded in lived experience. These services foster belonging and reinforce healthy norms—powerful protective factors against substance misuse.
Ultimately, community resource strategies to prevent abuse of opioids, nicotine, and alcohol emphasize access, education, and equity. When communities invest in prevention programs, integrated healthcare, peer support, and evidence-based policies, they create environments that support healthier choices. This shared responsibility approach reduces harm, strengthens resilience, and helps individuals and families thrive over the long term.
Frequently Asked Questions
Here are some common questions:
Why are opioids, nicotine, and alcohol considered the most addictive drugs?
These substances strongly affect the brain’s reward, motivation, and stress systems. They cause rapid dopamine release, lead to tolerance over time, and produce uncomfortable or dangerous withdrawal symptoms, which reinforce repeated use and dependence.
What makes opioids especially addictive?
Opioids bind directly to opioid receptors that regulate pain relief and pleasure. Repeated use reduces the brain’s natural opioid production, leading to physical dependence. Withdrawal symptoms—such as pain, nausea, anxiety, and cravings—can be severe, making opioids difficult to stop without medical support.
Why is nicotine considered highly addictive even though it’s legal?
Nicotine reaches the brain within seconds and reinforces frequent use by releasing dopamine and temporarily reducing stress. Because it is often used many times per day and socially normalized, dependence develops quickly and can last for years despite relatively mild short-term effects.
How does alcohol create addiction?
Alcohol affects multiple brain systems, including reward, inhibition, and stress regulation. Over time, the brain adapts to alcohol’s presence, leading to tolerance and dependence. Withdrawal can range from anxiety and tremors to seizures, making alcohol addiction medically serious.
Is alcohol addiction as dangerous as opioid addiction?
Yes. While opioids carry a high overdose risk, alcohol withdrawal can be life-threatening, and long-term alcohol misuse contributes to liver disease, heart problems, mental health disorders, and injuries. Alcohol’s social acceptance often delays recognition of harm.
Can someone become addicted to these substances without abusing them at first?
Yes. Many people begin using opioids for pain, nicotine for stress or social reasons, or alcohol casually. Dependence can develop gradually as tolerance increases and the brain adapts to repeated exposure.
Do these substances affect the brain in the same way?
They act on different receptors, but all ultimately hijack the brain’s dopamine system, reduce sensitivity to natural rewards, and increase cravings. Over time, decision-making and impulse control are impaired.
Is addiction to these drugs a lack of willpower?
No. Addiction is a medical and behavioral condition caused by predictable brain changes. Willpower alone is often insufficient because these substances alter motivation, stress response, and survival circuits in the brain.
Can people recover from addiction to opioids, nicotine, or alcohol?
Yes. Recovery is possible with the right combination of self-management strategies, medical care, behavioral therapy, family support, and community resources. Many people achieve long-term recovery with evidence-based treatment.
What helps prevent addiction to these substances?
Early education, safe prescribing practices, healthy coping skills, supportive family environments, and access to healthcare and community resources all reduce risk. Prevention is most effective when individuals, families, and communities work together.
Conclusion
Addiction to opioids, nicotine, and alcohol is not a failure of willpower, but a predictable response to repeated exposure that alters brain chemistry and behavior. Recognizing their addictive nature underscores the importance of early education, self-management strategies, family support, and community resources. With informed prevention and evidence-based care, the risks associated with these substances can be reduced, and long-term recovery is achievable.
Video: Opioids vs Nicotine vs Alcohol: Which Wins #addiction #comparison #facts