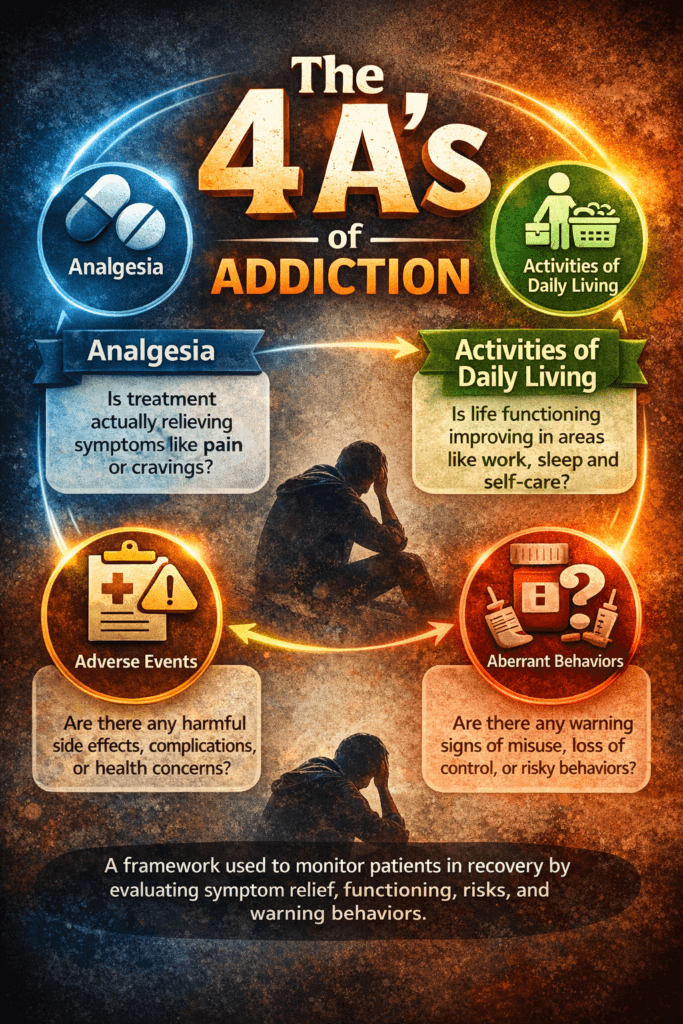
The 4 A’s framework—Analgesia, Activities of Daily Living, Adverse Events, and Aberrant Drug-Taking Behaviors—provides a structured, multidimensional approach to understanding addiction and monitoring recovery. Originally used in clinical settings to evaluate medication safety and effectiveness, it has evolved into a practical model that can guide individuals, families, and communities in recognizing both progress and warning signs. By examining symptom relief, daily functioning, risks, and behavioral patterns together, the 4 A’s move addiction care beyond guesswork and toward objective, compassionate assessment. This framework supports early intervention, informed decision-making, and personalized recovery strategies grounded in real-world outcomes rather than assumptions.
The 4 A’s in Addiction Monitoring: A Clinical Framework for Safe and Effective Care
The **4 A’s—Analgesia, Activities of Daily Living, Adverse Events, and Aberrant Drug-Taking Behaviors—**form a structured clinical framework for evaluating patients receiving controlled substances, especially opioids. Originally developed for pain-management monitoring, this model has become highly valuable in addiction medicine because it balances symptom relief with safety, function, and risk assessment. Rather than focusing solely on medication doses or lab results, the 4 A’s provide a multidimensional view of how treatment affects a person’s life, behavior, and health outcomes. This approach aligns with modern addiction care principles emphasizing functional recovery, patient-centered monitoring, and early detection of misuse patterns.
Analgesia — Is the Treatment Actually Helping?
Analgesia evaluates whether treatment is effectively reducing pain or the target symptom. In addiction-sensitive prescribing, symptom improvement must be measurable and clinically meaningful. Providers assess pain scores, symptom diaries, and patient-reported relief. Lack of improvement despite dose escalation may indicate tolerance, hyperalgesia, or misuse rather than undertreatment. In addiction medicine, this domain reinforces a key principle: medications should improve health, not simply be continued out of habit or fear of withdrawal.
Activities of Daily Living — Is Function Improving?
Activities of Daily Living (ADLs) measure functional outcomes, including work performance, mobility, sleep, self-care, and relationships. Functional improvement is often more meaningful than symptom reduction alone. For example, a patient reporting less pain but remaining socially withdrawn or unable to work may not truly be improving. In addiction treatment, restored functioning is a core recovery indicator. Monitoring ADLs shifts the clinical focus from symptom suppression to life restoration.
Adverse Events — Are There Harms or Risks?
Adverse Events include side effects, complications, or safety concerns related to treatment. These may range from mild sedation or constipation to serious outcomes such as respiratory depression, overdose risk, or medication interactions. In addiction-informed care, clinicians also evaluate psychological effects like mood changes, impulsivity, or cognitive slowing. Monitoring harms ensures that the benefits of treatment outweigh the risks—an ethical cornerstone of prescribing controlled medications.
Aberrant Drug-Taking Behaviors — Are There Warning Signs?
Aberrant behaviors refer to patterns suggesting misuse, diversion, or loss of control. Examples include early refill requests, dose escalation without approval, lost prescriptions, multiple prescribers, or using medication for reasons other than prescribed. Importantly, these behaviors are not automatic proof of addiction—they may signal undertreated pain, misunderstanding, or psychological distress. However, identifying them early allows clinicians to intervene with assessment, education, treatment adjustment, or referral to addiction services.
Why the 4 A’s Matter in Addiction-Informed Care
This framework is powerful because it integrates symptom relief, functional outcomes, safety monitoring, and behavioral assessment into one clinical model. Instead of labeling patients prematurely, it promotes structured observation and objective decision-making. It also supports collaborative care: patients understand what clinicians are monitoring and why, which strengthens trust and accountability.
From a systems perspective, the 4 A’s help standardize documentation, reduce prescribing bias, and guide ethical treatment decisions. For clinicians, they function as a quick mental checklist; for patients, they provide transparent treatment goals; and for healthcare systems, they create measurable quality indicators.
Clinical Takeaway
The 4 A’s framework transforms addiction-sensitive prescribing from guesswork into evidence-guided monitoring. When applied consistently, it helps clinicians answer four essential questions:
- Is the medication helping?
- Is life functioning improving?
- Are there harms?
- Are there warning signs?
When all four domains are evaluated together, treatment becomes safer, more individualized, and more aligned with long-term recovery outcomes—ultimately supporting both effective symptom management and responsible addiction prevention.
Self-Management Strategies Using the 4 A’s in Addiction Recovery
The **4 A’s framework—Analgesia, Activities of Daily Living, Adverse Events, and Aberrant Drug-Taking Behaviors—**is not just a clinical monitoring tool for providers; it can also be transformed into a powerful self-management system for individuals in recovery or receiving controlled medications. When used personally, the model helps people track how substances or medications affect their body, behavior, and life functioning. This structured awareness promotes insight, accountability, and early intervention—three pillars of sustainable recovery. Instead of relying on vague feelings about progress, individuals can use the 4 A’s to objectively evaluate whether their current treatment or coping strategies are helping or harming their long-term goals.
Analgesia — Track Symptom Relief Honestly
Self-management begins with honest monitoring of symptom relief or craving intensity. Ask yourself daily:
Is what I’m using actually helping me feel better—or just temporarily numbing discomfort?
Keep a simple log of pain levels, cravings, stress, or emotional triggers. If symptoms don’t improve over time—or worsen despite increasing use—it may signal tolerance, dependence risk, or ineffective coping strategies. Awareness prevents escalation and supports timely adjustments such as therapy, medication review, or behavioral interventions.
Activities of Daily Living — Measure Real-Life Progress
Recovery success is best measured by function, not just abstinence. Evaluate whether your daily life is improving:
- Are you sleeping regularly?
- Are relationships stabilizing?
- Is work or school performance improving?
- Do you feel more motivated and present?
Tracking these indicators weekly shows whether your recovery plan is translating into real-world stability. If functioning declines, it’s a signal to reassess stressors, triggers, or treatment supports.
Adverse Events — Watch for Physical and Emotional Side Effects
Self-monitoring for negative consequences helps prevent relapse and medical harm. Adverse effects may include fatigue, mood swings, anxiety, isolation, poor concentration, or physical symptoms. Many people ignore early warning signs because they develop gradually. Recording them makes patterns visible. If negative effects outweigh benefits, it’s time to seek professional guidance or modify your strategy. Recovery thrives when individuals learn to respond early rather than waiting for crises.
Aberrant Behaviors — Identify Warning Signs of Loss of Control
Aberrant behaviors are early indicators of relapse risk, not moral failures. Examples include:
- Using more than intended
- Hiding use
- Making excuses for use
- Obsessive thoughts about substances
- Breaking personal rules
Self-management means recognizing these signals quickly and responding with support strategies—such as calling a sponsor, attending a meeting, adjusting routines, or reaching out to a clinician. Early response prevents small slips from becoming full relapses.
Integrating the 4 A’s Into a Daily Recovery System
To apply the model practically, many individuals create a simple daily check-in template:
| Domain | Daily Question |
|---|---|
| Analgesia | Did my coping method actually help? |
| ADLs | Did my life function improve today? |
| Adverse Events | Did anything negative happen because of my choices? |
| Aberrant Behaviors | Did I notice warning signs of loss of control? |
Answering these questions takes less than two minutes but builds powerful self-awareness. Over time, patterns emerge that guide smarter decisions and strengthen recovery insight.
Why This Framework Works
The 4 A’s succeed as a self-management strategy because they integrate biology, behavior, psychology, and lifestyle into one structured reflection tool. Many relapse episodes occur not because people lack motivation, but because warning signs go unnoticed. This model trains individuals to observe themselves like a clinician would—objectively, compassionately, and consistently.
Final Insight
Recovery is not just about stopping a behavior; it’s about learning how to evaluate your own well-being. The 4 A’s transform self-reflection into a measurable skill. When individuals regularly monitor relief, functioning, risks, and behaviors, they gain control over patterns that once felt automatic. Over time, this awareness becomes one of the strongest protective factors against relapse and one of the most reliable guides toward lasting stability.
Family Support Strategies Using the 4 A’s Framework in Addiction Recovery
Families play a powerful role in addiction recovery—not by controlling outcomes, but by creating an environment that supports stability, accountability, and healing. The **4 A’s framework—Analgesia, Activities of Daily Living, Adverse Events, and Aberrant Drug-Taking Behaviors—**can guide families in providing structured, compassionate support. When applied thoughtfully, this model helps loved ones observe progress objectively, respond early to warning signs, and encourage recovery-oriented behaviors without judgment or enabling. Instead of reacting emotionally to crises, families can use the 4 A’s as a calm, practical checklist for supporting long-term recovery.
Analgesia — Support What Truly Helps
Families can help assess whether treatment or coping strategies are genuinely relieving symptoms such as pain, cravings, anxiety, or distress. Supportive questions include:
Do you feel better using this strategy?
Is it helping in the long term or just in the moment?
Rather than criticizing or policing, families act as mirrors—reflecting patterns the individual may not see. Encouraging honest discussion helps distinguish true therapeutic benefit from temporary relief that may reinforce dependence.
Activities of Daily Living — Reinforce Functional Progress
Functional improvement is one of the strongest indicators of recovery. Families can support this domain by noticing and reinforcing progress, such as improved sleep, consistent routines, better hygiene, stable employment, or renewed hobbies. Positive reinforcement matters—acknowledging small steps builds confidence and motivation. Instead of focusing solely on setbacks, families who highlight growth help shift recovery from a problem-focused to a strengths-based approach.
Adverse Events — Watch for Early Warning Signs
Loved ones are often the first to notice subtle changes that signal trouble, such as mood swings, isolation, excessive sleep, irritability, or physical decline. Observing these changes early allows families to respond with concern rather than alarm. Instead of accusations, supportive language works best:
“I’ve noticed you seem more tired lately—how are you feeling?”
This approach reduces defensiveness and encourages open dialogue, making it easier for individuals to accept help before problems escalate.
Aberrant Behaviors — Respond Early and Calmly
Aberrant behaviors—such as secrecy, missed obligations, frequent crises, or inconsistent stories—can indicate loss of control or relapse risk. Families should respond early but calmly. Effective strategies include:
- Setting clear, consistent boundaries
- Avoiding enabling behaviors
- Encouraging professional support
- Maintaining accountability agreements
The goal is not punishment but protection—protecting the individual, the family system, and the recovery process. Calm consistency is far more effective than emotional confrontation.
Putting the 4 A’s Into Practice as a Family Tool
Families can hold weekly check-ins using simple questions:
| Domain | Family Reflection Question |
|---|---|
| Analgesia | Does their current plan seem to truly help them? |
| ADLs | Are they functioning better in daily life? |
| Adverse Events | Have we noticed concerning changes? |
| Aberrant Behaviors | Are there warning signs we should address? |
This structured approach keeps conversations focused on observable patterns rather than blame or assumptions.
Why Family Use of the 4 A’s Works
Families often struggle because they want to help but don’t know how. The 4 A’s provide a clear roadmap that replaces guesswork with observation and supportive action. It also shifts the role of family members from “fixers” to “supportive partners in recovery.” When loved ones focus on measurable signs of progress and risk, they foster trust, reduce conflict, and strengthen long-term recovery outcomes.
Final Thought
Addiction recovery is rarely successful in isolation. Families who use structured strategies like the 4 A’s create environments where growth is noticed, risks are addressed early, and accountability is balanced with compassion. Over time, this consistent, informed support becomes one of the strongest protective factors against relapse—and one of the greatest sources of hope for lasting recovery.
Community Resource Strategies Using the 4 A’s Framework in Addiction Recovery
Recovery is strengthened when communities provide structured, accessible systems of support. The **4 A’s framework—Analgesia, Activities of Daily Living, Adverse Events, and Aberrant Drug-Taking Behaviors—** offers a practical model for designing community programs that are not only compassionate but also measurable and effective. When community resources use this framework, they shift from simply offering services to delivering outcome-focused recovery support. Instead of asking “Are services available?” communities begin asking, “Are services improving lives, functioning, safety, and stability?” This shift transforms recovery systems into proactive networks that identify risks early and reinforce progress consistently.
Analgesia — Community Programs That Actually Help
At the community level, Analgesia means evaluating whether programs truly reduce distress, cravings, withdrawal symptoms, or emotional suffering. Effective community strategies include:
- Access to counseling and therapy services
- Medication-assisted treatment programs
- Peer recovery groups
- Crisis hotlines
Communities that measure symptom improvement—not just attendance—ensure resources are making a real difference. Data such as reduced emergency visits, decreased cravings, or improved mood scores can help determine whether services are working.
Activities of Daily Living — Supporting Functional Recovery
Recovery success is strongly tied to improved functioning. Communities can support Activities of Daily Living (ADLs) by providing programs that rebuild life stability:
- Job training and employment services
- Transportation assistance
- Housing programs
- Education and life-skills training
When these services are integrated with addiction treatment, individuals are more likely to maintain recovery because they gain purpose, structure, and independence. Measuring outcomes such as employment rates, housing stability, or school completion provides tangible indicators of success.
Adverse Events — Community Safety and Harm Reduction
Communities play a critical role in identifying and reducing harm. Monitoring Adverse Events means tracking overdoses, hospitalizations, medication complications, and mental health crises. Effective strategies include:
- Overdose prevention education
- Naloxone distribution programs
- Mobile health clinics
- Integrated mental health services
These interventions don’t just treat addiction—they prevent tragedies. Communities that prioritize harm reduction demonstrate a public-health approach rather than a punishment-focused one.
Aberrant Behaviors — Early Identification Systems
Community organizations are often the first to notice warning signs such as frequent crises, repeated relapses, legal trouble, or disengagement from services. Structured monitoring systems help detect aberrant behaviors early. Strategies include:
- Case management programs
- Coordinated care networks
- Outreach teams
- School and workplace screening initiatives
Early identification allows communities to intervene before patterns escalate into medical, legal, or social emergencies.
Implementing the 4 A’s as a Community Model
Communities can use a simple evaluation matrix:
| Domain | Community Question |
|---|---|
| Analgesia | Are our services reducing distress and symptoms? |
| ADLs | Are people functioning better in daily life? |
| Adverse Events | Are harms and crises decreasing? |
| Aberrant Behaviors | Are we identifying risks early? |
This framework helps leaders allocate funding, improve programs, and measure real outcomes rather than relying on assumptions.
Why Community Application Matters
Addiction is not only an individual challenge—it is shaped by social conditions such as housing, employment, healthcare access, stigma, and education. Community systems that apply structured frameworks, such as the 4 A’s, can coordinate services across sectors, reduce duplication, and ensure resources address real needs. This approach strengthens collaboration between healthcare providers, social services, schools, employers, and peer networks.
Final Insight
Communities that adopt the 4 A’s framework move from reactive crisis response to proactive recovery support. By measuring relief, functioning, safety, and behavioral risk across programs, they create environments where individuals are more likely to stabilize, grow, and sustain recovery. In this way, the 4 A’s become more than a clinical checklist—they become a blueprint for building healthier, safer, recovery-ready communities.
Frequently Asked Questions
Here are some common questions:
1. What are the 4 A’s in addiction?
The **4 A’s—Analgesia, Activities of Daily Living, Adverse Events, and Aberrant Drug-Taking Behaviors—**are a structured framework for evaluating how a treatment or substance use pattern affects a person’s symptoms, functioning, safety, and behavior. It is commonly used in clinical monitoring but can also guide personal recovery tracking.
2. Why is the 4 A’s model important?
It provides a balanced assessment rather than focusing on a single factor, such as abstinence or symptom relief. Evaluating relief, functioning, risks, and behavior together helps detect early warning signs and supports safer, more effective recovery planning.
3. Is the 4 A’s framework only for clinicians?
No. While healthcare professionals often use it, individuals, families, and community programs can apply it as a self-reflection or monitoring tool to track progress and identify concerns early.
4. What does “Analgesia” mean in addiction monitoring?
It refers to whether treatment or coping strategies are actually relieving symptoms such as pain, cravings, or emotional distress. If relief is minimal or short-lived, it may indicate the need for a different approach.
5. Why are Activities of Daily Living included?
Functioning is one indicator of recovery. Improvements in sleep, relationships, work, hygiene, and motivation often show real progress more accurately than symptom scores alone.
6. What counts as an Adverse Event?
Adverse events include negative physical, emotional, or behavioral consequences such as medication side effects, mood instability, cognitive problems, overdoses, or worsening mental health symptoms.
7. What are Aberrant Drug-Taking Behaviors?
These are warning signs of possible misuse or loss of control. Examples include taking more than prescribed, seeking early refills, hiding use, or using substances for unintended reasons. They signal the need for evaluation—not judgment.
8. Does noticing aberrant behaviors mean someone is addicted?
Not necessarily. Such behaviors can stem from many causes, including unmanaged pain, stress, misunderstanding instructions, or mental health challenges. They should prompt assessment and support rather than assumptions.
9. How often should the 4 A’s be evaluated?
Frequency depends on risk level. Clinically, high-risk patients may be monitored weekly, while stable individuals may be assessed monthly or quarterly. For personal use, brief daily or weekly check-ins work well.
10. How can families use the 4 A’s?
Families can observe changes in functioning, mood, and behavior while encouraging open communication. The framework helps them discuss concerns objectively and support recovery without blaming or enabling.
11. Can the 4 A’s help prevent relapse?
Yes. Because it emphasizes early detection of changes in symptoms, functioning, or behaviors, the model helps identify relapse risk before it escalates into crisis.
12. What makes this framework effective?
Its strength lies in simplicity and completeness. The 4 A’s cover the four essential questions of addiction monitoring:
Is it helping? Is life improving? Is it safe? Are there warning signs?
Conclusion
The strength of the 4 A’s lies in their simplicity and completeness: they capture the essential indicators of whether a recovery plan is working, safe, and sustainable. When consistently applied, this model helps transform addiction management into a proactive process that prioritizes stability, accountability, and well-being. Whether used by clinicians, individuals in recovery, or support systems, the 4 A’s provide a reliable compass for navigating complex treatment decisions and preventing relapse. Ultimately, they reinforce a core principle of modern addiction care—lasting recovery is achieved not just by reducing symptoms, but by improving life function, minimizing harm, and supporting healthy behavioral patterns over time.
Video: