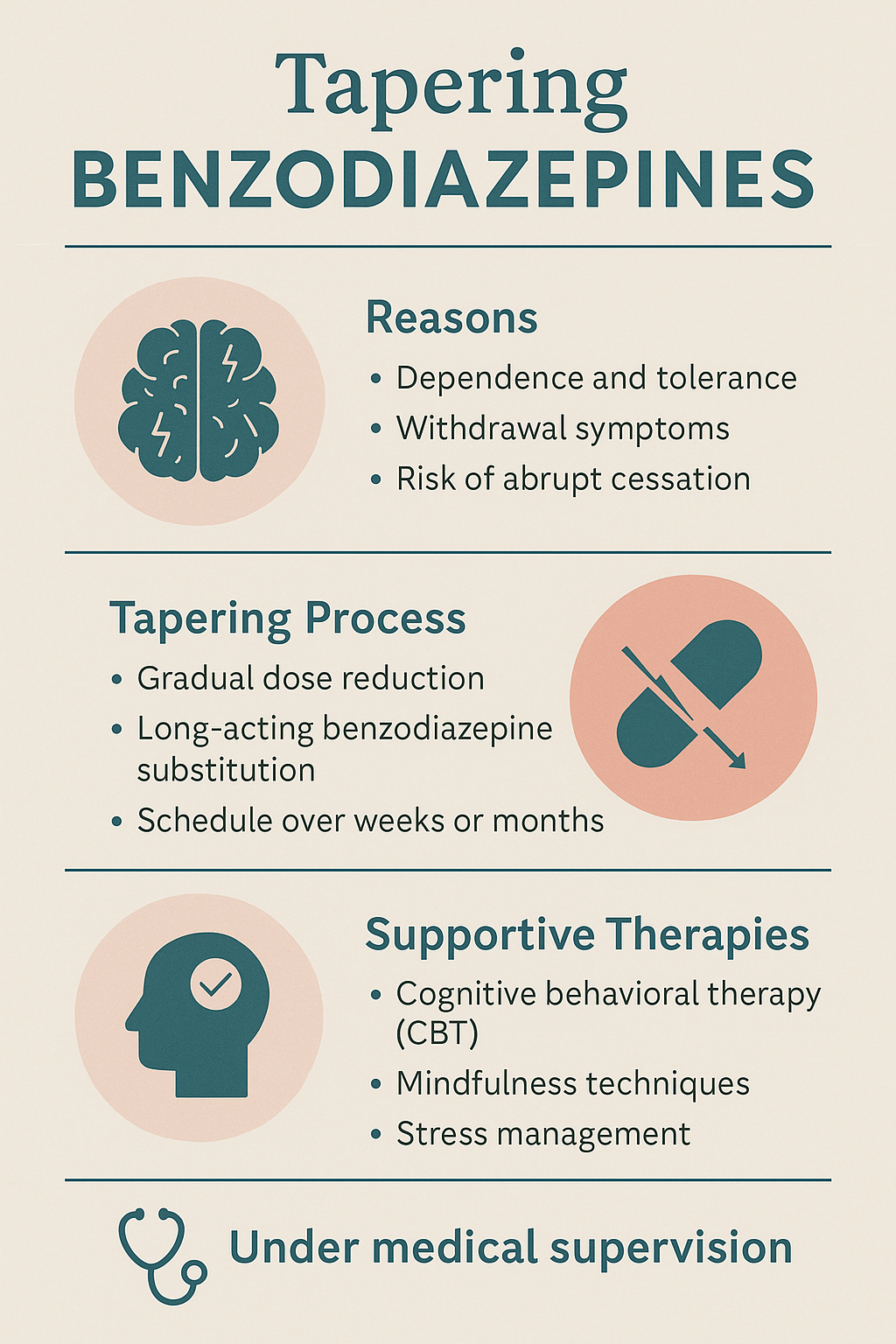
Tapering off benzodiazepines slowly is essential due to the drug’s strong effects on the central nervous system and the serious risks of abrupt withdrawal, including seizures, panic attacks, and rebound anxiety. A gradual reduction allows the brain to readjust safely while minimizing withdrawal symptoms. However, this process is not without its disadvantages—it can be prolonged, emotionally taxing, and requires ongoing support. Ethical dilemmas may also arise, especially when patient autonomy conflicts with medical judgment or when access to proper tapering care is unequal. Successful benzodiazepine tapering depends on effective self-management strategies, compassionate family involvement, and well-coordinated community resources such as mental health clinics, peer support, and counseling services. Together, these supports help individuals navigate withdrawal safely and rebuild their lives without dependence.
Why Benzodiazepines Must Be Tapered Slowly: Protecting the Brain and Supporting Recovery
Benzodiazepines are powerful medications used to treat anxiety, insomnia, seizures, and more. While effective in the short term, long-term use can lead to physical dependence. Tapering benzodiazepines gradually is essential to avoid serious risks and support a safe transition off the medication.
⚠️ The Science Behind Dependence
Benzodiazepines work by enhancing the action of GABA-A receptors, which help calm the central nervous system (CNS). Over time, the brain adapts to this external calming effect and reduces its own natural GABA activity. Abruptly stopping benzodiazepines after regular use disrupts this balance, leading to potentially dangerous withdrawal symptoms.
🔄 Key Reasons Benzodiazepines Must Be Tapered Slowly
1. Prevent Severe Withdrawal Symptoms
A sudden stop can trigger intense symptoms, including:
- Rebound anxiety and insomnia
- Irritability and restlessness
- Nausea and muscle cramps
- Panic attacks
These symptoms can be distressing and may lead to reinstating the medication or seeking emergency care.
2. Avoid Life-Threatening Complications
In some cases, abrupt withdrawal may lead to:
- Seizures
- Delirium
- Psychosis
These are medical emergencies that may require hospitalization and intensive care.
3. Allow the Brain to Rebalance Gradually
A slow taper gives the brain’s GABA system time to recalibrate. This:
- Reduces withdrawal intensity
- Supports mood stability
- Helps restore natural sleep patterns
4. Improve Success and Reduce Relapse
Gradual tapering increases the chance of:
- Completing the taper
- Avoiding relapse
- Staying engaged in care and recovery
A smooth, tolerable withdrawal experience makes long-term success more achievable.
🕒 What Does a Typical Taper Look Like?
- Reduce the current dose by 10–25% every 1–2 weeks
- Adjust speed based on symptom response
- Switch to a longer-acting benzodiazepine (like diazepam) if needed for smoother transitions
✅ Summary: Tapering Is a Medical Necessity
Benzodiazepine withdrawal is not just uncomfortable—it can be life-threatening if done improperly. A slow, medically supervised taper helps protect your brain, improve comfort, and support long-term recovery.
Always consult your healthcare provider before making any changes to your medication. You’re not alone—safe tapering is possible with the right plan and support.
The Challenges of Tapering Benzodiazepines: What Patients Should Know
Tapering benzodiazepines is the safest way to discontinue their use—but it’s not without its challenges. For people who have used these medications long-term or at high doses, tapering can bring physical, emotional, and logistical difficulties. Understanding these disadvantages helps patients and healthcare providers better prepare for a safe and successful withdrawal process.
🚫 Disadvantages of Tapering Benzodiazepines
1. Withdrawal Symptoms (Even During a Taper)
Even with a slow reduction, many people still experience uncomfortable symptoms, such as:
- Anxiety or panic attacks
- Insomnia
- Irritability or mood swings
- Muscle tension or tremors
- Nausea, dizziness, or headaches
These symptoms may last for weeks or even months, a phenomenon known as protracted withdrawal.
2. Emotional and Psychological Stress
Tapering can intensify or unmask underlying mental health issues, including:
- Generalized anxiety
- Depression
- Post-Traumatic Stress Disorder (PTSD)
Without the numbing or calming effects of benzodiazepines, many people feel emotionally raw and vulnerable.
3. Time-Consuming and Prolonged Process
A careful, slow taper may last months to over a year, depending on the individual’s dose, length of use, and sensitivity to withdrawal.
This extended timeline requires ongoing support, patience, and planning.
4. Functional Impairment During Taper
Symptoms during tapering can affect daily life. Some individuals may struggle with:
- Returning to work
- Managing relationships
- Handling everyday stress
These challenges can create frustration and may increase the urge to stop tapering or return to prior doses.
5. Relapse Risk
Withdrawal-related distress and psychological dependency may cause some individuals to relapse—either by resuming benzodiazepine use or turning to other substances like alcohol or opioids for relief.
6. Need for Close Monitoring and Specialized Care
Safe tapering often requires:
- Frequent follow-ups with healthcare providers
- Psychological therapy or counseling
- Use of other medications (e.g., antidepressants, beta blockers, or non-benzodiazepine anxiolytics)
This level of care can be difficult for some patients to access and may strain healthcare systems.
✅ Summary Table: Disadvantages of Benzodiazepine Tapering
| Challenge | Impact |
|---|---|
| Withdrawal symptoms | Anxiety, insomnia, physical discomfort |
| Emotional distress | Worsening of underlying mental health conditions |
| Time commitment | Taper may take several months or longer |
| Functional limitations | Trouble with work, relationships, or daily tasks |
| Risk of relapse | May return to benzodiazepines or other substances |
| Need for support | Requires coordinated medical and psychological care |
Ethical Dilemmas in Tapering Benzodiazepines: Balancing Patient Rights and Clinical Duty
Tapering benzodiazepines—especially long-term medications like diazepam—presents complex ethical questions. Healthcare providers must weigh the patient’s right to choose against clinical responsibility to reduce harm. These decisions are guided by core ethical principles: autonomy, beneficence, nonmaleficence, justice, and informed consent.
Below are the most common ethical dilemmas faced in benzodiazepine tapering.
1. Autonomy vs. Medical Responsibility
Dilemma: What happens when a patient wants to stay on benzodiazepines, but the provider recommends tapering due to health risks?
- Providers must respect patient autonomy while upholding their duty not to harm.
- Long-term use is associated with risks like dependence, cognitive decline, and falls.
- Ethical question: When is it appropriate to override a patient’s preference for their own safety?
2. Risk of Harm vs. Potential Benefit
- Tapering may cause distress, withdrawal, and relapse, but continuing the medication can cause long-term harm.
- Providers must weigh whether the risks of tapering outweigh the risks of continued use.
- This is especially challenging in patients with trauma histories or older adults.
3. Informed Consent and Shared Decision-Making
- Many patients were started on benzodiazepines without a complete understanding of the long-term consequences.
- Providers now face the task of rebuilding trust and ensuring patients receive updated, honest information to make a truly informed decision.
4. Coercion in Healthcare Settings
- Some systems enforce tapering policies without patient input, such as:
- Automatic discontinuation
- Tying tapering to access to other care services
- These approaches may be experienced as coercive, damaging trust, and limiting patient agency.
5. Disparities in Access to Support
- Successful tapering often requires:
- Access to therapy (e.g., CBT)
- Non-benzodiazepine medications
- Frequent provider follow-ups
- Patients with limited access face greater suffering, raising issues of equity and justice in care.
6. Fear of Abandonment and Stigma
- Patients may feel rejected or punished when a taper is suggested.
- If the taper is not framed as compassionate care, but as a response to stigma or policy, it can violate the principle of beneficence—acting in the patient’s best interest.
✅ Summary Table: Common Ethical Conflicts in Benzodiazepine Tapering
| Risk of stigma, coercion, or the patient feeling dismissed or abandoned | Dilemma |
|---|---|
| Autonomy | Patient wants continued use vs. provider recommends tapering |
| Nonmaleficence | Risk of withdrawal symptoms and suffering during taper |
| Beneficence | Need to promote long-term well-being without causing short-term harm |
| Justice | Unequal access to taper support (therapy, continuity, insurance) |
| Informed consent | Patients unaware of long-term risks when first prescribed medication |
| Respect and dignity | Risk of stigma, coercion, or patient feeling dismissed or abandoned |
This ethical landscape highlights why benzodiazepine tapers must be collaborative, compassionate, and informed. It’s not just about medical safety—it’s about honoring patient dignity and delivering ethical, person-centered care.
Tapering Benzodiazepines: 8 Essential Self-Management Strategies for a Safer, Smoother Withdrawal
Tapering benzodiazepines is a gradual, often challenging process that requires more than just a dosage plan—it calls for self-management strategies that empower individuals to manage withdrawal symptoms, reduce anxiety, and build long-term resilience without relying on the medication. These strategies are essential for preventing relapse and improving emotional and physical well-being during and after tapering.
✅ Self-Management Strategies to Taper Benzodiazepines
🧠 1. Educate Yourself About the Tapering Process
- Understand how benzodiazepines affect the brain and what to expect during withdrawal.
- Learn about protracted withdrawal symptoms and how long they may last.
- Track your taper schedule and symptoms in a journal.
📘 Tip: Use reputable sources like the Ashton Manual or consult a provider experienced in tapering.
🧘 2. Practice Daily Stress Reduction Techniques
- Engage in relaxation strategies to manage anxiety, such as:
- Deep breathing exercises (e.g., 4-7-8 technique)
- Progressive muscle relaxation
- Guided imagery or meditation apps (e.g., Calm, Insight Timer)
💡 These practices support the body’s nervous system as it adjusts to lower medication levels.
🛌 3. Establish a Regular Sleep Routine
- Benzodiazepine withdrawal often affects sleep. Promote better rest by:
- Going to bed and waking up at the same time daily
- Avoiding screens, caffeine, and heavy meals before bed
- Creating a calming bedtime ritual (e.g., herbal tea, light stretching)
🌙 Even if sleep is disrupted, consistency helps the brain restore natural sleep rhythms.
🍎 4. Maintain a Balanced Diet and Stay Hydrated
- Eat nutrient-rich meals to support brain and nervous system function.
- Stay hydrated to help regulate body systems affected by withdrawal.
- Limit sugar, caffeine, and alcohol, which can worsen anxiety and withdrawal symptoms.
🏃 5. Stay Physically Active
- Regular exercise releases endorphins and reduces stress.
- Even short walks, yoga, or gentle stretching can help.
- Movement supports detoxification and naturally improves mood.
📅 6. Follow a Structured Daily Routine
- Having structure gives your day purpose and stability.
- Schedule meals, exercise, hobbies, and rest periods.
- This helps reduce the mental fog and emotional instability that may arise during tapering.
📓 Use planners or habit trackers to stay organized and motivated.
👥 7. Build a Support System
- Stay connected with friends, family, peer support groups, or online communities (e.g., BenzoBuddies).
- Share your progress and challenges regularly with someone you trust.
- Consider finding a therapist with experience in anxiety or substance withdrawal.
💬 You don’t have to taper alone—connection reduces isolation and discouragement.
🧾 8. Communicate with Your Provider
- Report symptoms regularly and adjust the taper speed if needed.
- Ask about medications or supplements (e.g., melatonin, magnesium) that may ease specific symptoms.
- Keep a list of questions and concerns for appointments.
✅ Summary: Key Self-Management Strategies
| Communication with the provider | Purpose |
|---|---|
| Education & journaling | Stay informed and track symptoms |
| Stress-reduction techniques | Manage anxiety and physical discomfort |
| Sleep hygiene | Promote rest and brain recovery |
| Healthy nutrition | Support nervous system and emotional stability |
| Exercise | Improve mood and reduce tension |
| Daily structure | Enhance focus and reduce feelings of chaos |
| Social support | Provide encouragement and accountability |
| Communication with provider | Ensure safe, personalized taper adjustments |
Supporting a Loved One Tapering Benzodiazepines: 8 Key Family Strategies for Compassionate Care
Supporting a loved one who is tapering off benzodiazepines can be emotionally complex and demanding—but families play a vital role in ensuring safety, motivation, and long-term recovery. Effective family involvement combines empathy, education, consistency, and healthy boundaries to reduce anxiety and promote healing.
💞 Family Support Strategies for Benzodiazepine Tapering
🧠 1. Get Educated Together
- Learn about:
- Benzodiazepine dependence and withdrawal
- The importance of slow tapering
- Possible physical and emotional symptoms
- This helps the family respond with understanding rather than fear or frustration.
📘 Use trusted resources like the Ashton Manual, NIDA, or speak with a medical provider.
💬 2. Open Non-Judgmental Communication
- Create space for your loved one to talk about what they’re feeling without shame.
- Avoid pushing, criticizing, or minimizing their experience.
- Validate the difficulty of the process, and ask how you can help.
What to say:
“This seems really tough—I’m here if you need to talk or just sit quietly.”
📆 3. Support Structure and Daily Routine
- Help them:
- Keep regular sleep and meal times
- Schedule activities, exercise, or appointments
- Stick to the taper plan (without policing)
📅 Example: Offer to go for a walk together every morning to create a routine and reduce anxiety.
🙌 4. Be Present During Challenging Moments
- Withdrawal may cause:
- Panic attacks, insomnia, mood swings, or fatigue
- Offer reassurance and calming strategies, such as grounding exercises or distraction (e.g., listening to music, simple tasks).
- Know when to encourage professional support or call for help.
🚨 Tip: Understand signs of medical emergencies like seizures or extreme disorientation.
🚧 5. Respect Their Pace and Autonomy
- Tapering needs to be gradual and person-led.
- Don’t pressure them to speed up or quit “cold turkey.”
- Support their goals and help them speak with their provider if adjustments are needed.
🎯 Your role is to encourage, not to control.
👥 6. Encourage Mental Health and Peer Support
- Help find:
- A therapist or counselor experienced in benzo withdrawal
- Peer support groups (in-person or online)
- Attend family sessions or groups if available to learn how to support without enabling.
💡 Tip: Family therapy or Al-Anon-style support may help you process your own emotions, too.
🧠 7. Promote Healthy Lifestyle Choices
- Join them in:
- Cooking healthy meals
- Reducing screen time or stimulants (e.g., caffeine)
- Practicing mindfulness or relaxation techniques together
🏃 Shared routines strengthen bonds and boost both of your well-being.
🧾 8. Track Progress and Celebrate Small Wins
- Help them track milestones (e.g., dose reductions, better sleep).
- Celebrate successes—even tiny ones—with praise or positive reinforcement.
- This builds confidence and keeps motivation high.
🎉 “You’ve made it another week—look how far you’ve come!”
✅ Summary Table: Family Support for Benzodiazepine Tapering
| Stay calm during challenging moments | How It Helps |
|---|---|
| Educate yourselves | Reduces fear, improves empathy and confidence |
| Communicate openly | Builds trust and emotional safety |
| Support daily structure | Lowers stress and supports stability |
| Stay calm during tough moments | Provides reassurance and reduces escalation |
| Respect the pace of taper | Encourages autonomy and prevents power struggles |
| Promote support services | Builds a broader recovery team |
| Encourage healthy habits | Improves mood and physical resilience |
| Celebrate progress | Boosts motivation and self-esteem |
Community Resource Strategies to Support Safe and Successful Benzodiazepine Tapering
Tapering benzodiazepines safely and successfully often requires more than individual or family support—it also depends on accessible and coordinated community resources. These strategies help address withdrawal symptoms, mental health needs, housing or employment issues, and long-term recovery support, especially for those tapering in high-risk or underserved settings.
🏥 Community Resource Strategies to Support Benzodiazepine Tapering
🧑⚕️ 1. Community-Based MAT and Mental Health Clinics
- Local health centers and behavioral clinics can:
- Offer medically supervised tapers
- Monitor withdrawal symptoms and co-occurring disorders
- Provide alternatives like SSRIs, CBT, or trauma therapy
🏥 Look for clinics that integrate substance use and mental health treatment under one roof.
👩⚕️ 2. Primary Care Provider Collaboration
- Some communities use integrated care models where primary care providers work closely with behavioral health specialists.
- Patients can receive:
- Medication management
- Sleep or anxiety care
- Referrals to psychiatry or counseling
🩺 These settings reduce stigma and make tapering part of routine care.
🧘 3. Access to Supportive Therapies
- Community wellness centers, nonprofits, or county programs may offer:
- Cognitive Behavioral Therapy (CBT)
- Mindfulness-Based Stress Reduction (MBSR)
- Art, music, or movement therapy to reduce anxiety during tapering
💡 Complementary therapies are valuable during the emotional ups and downs of withdrawal.
🚶 4. Peer Recovery and Support Groups
- Peer-led groups reduce isolation, build accountability, and offer tips from lived experience.
- Examples: SMART Recovery, BenzoBuddies (online), recovery cafés
- Some mental health-focused peer groups are benzo-aware and nonjudgmental.
🤝 Peer mentors can help bridge the gap between clinical care and everyday life.
🏘️ 5. Recovery Housing or Sober Living Programs
- Structured environments that support medication tapers and relapse prevention.
- Important for those with unstable housing, co-occurring substance use, or social stressors.
🏡 Look for homes that welcome individuals tapering medications—not just abstinence-only programs.
📚 6. Workshops and Community Education Programs
- Libraries, community colleges, or health departments may offer:
- Health literacy classes about benzodiazepines
- Stress management workshops
- Tapering support seminars
🎓 Education builds empowerment, especially for those who weren’t informed about long-term benzo risks.
🚌 7. Transportation and Access Assistance
- Local nonprofits or Medicaid programs may provide:
- Rides to appointments
- Help with insurance, sliding scales, or medication costs
🚐 Transportation and financial support reduce drop-off during the tapering process.
🧾 8. Crisis and Emergency Resources
- Community crisis lines, mobile crisis units, or mental health urgent care can step in if:
- Withdrawal symptoms escalate
- Suicidal thoughts or panic episodes occur
📞 Knowing where to go in a crisis can prevent emergency room visits or unsafe situations.
✅ Summary: Community Resources for Benzo Tapering
| Resource Strategy | Purpose |
|---|---|
| Community mental health clinics | Supervised tapering, therapy, and medical support |
| Primary care integration | Low-barrier access to coordinated care |
| Supportive therapies | Emotional regulation and stress reduction |
| Peer recovery networks | Encouragement and guidance from lived experience |
| Recovery housing | Stability and structure during vulnerable periods |
| Education programs | Knowledge and self-empowerment |
| Transportation/insurance support | Reducing barriers to consistent treatment |
| Crisis intervention services | Safety and de-escalation when symptoms worsen |
Frequently Asked Questions
Here are some common questions:
Question: Provide a guideline for providers on how to taper Benzodiazepines safely for the patients?
Answer:
✅ Benzodiazepine Tapering Guideline for Providers
1. Initial Assessment
- Indications for tapering:
- Long-term use (>4 weeks)
- Dependence or tolerance
- Adverse effects (e.g., cognitive impairment, falls)
- Patient request
- Evaluate:
- Duration and dosage
- Type of benzodiazepine (short vs. long-acting)
- Psychiatric comorbidities (anxiety, depression, PTSD)
- Substance use history
- Medical status and risk factors (e.g., seizures, liver disease)
- Support system availability
2. Patient Education & Shared Decision-Making
- Explain:
- Risks of long-term use (dependence, sedation, memory issues)
- Benefits of tapering (improved function, reduced risk of falls/cognitive decline)
- Withdrawal symptoms (e.g., anxiety, insomnia, tremors)
- Expectation of a slow, supportive taper process
- Encourage patient input and agreement on pace and method
3. Taper Plan Design
🧠 General Principles:
- Slow, individualized taper
- Longer tapers = higher success & fewer withdrawals
- Adjust taper speed based on patient response and withdrawal symptoms
📉 Taper Rate:
- Reduce the dose by 5–10% every 1–2 weeks
- In some cases (long-term/high-dose use), start at a 10–25% reduction every 2–4 weeks, then slow down
- Pause or slow taper if withdrawal symptoms worsen
⏳ Switch to Long-acting Agent (if needed):
- For patients on short-acting BZDs (e.g., alprazolam, lorazepam), convert to diazepam equivalent
- Diazepam has a long half-life and easier dosing
- Use the conversion chart carefully to avoid over- or under-dosing
4. Monitoring During Taper
- Schedule regular follow-ups (weekly to biweekly early in taper)
- Assess for:
- Withdrawal symptoms (anxiety, irritability, insomnia, panic, tremors)
- Psychiatric symptoms (depression, suicidal ideation)
- Drug cravings or relapse to other substances
- Use symptom rating scales if needed (e.g., CIWA-B for withdrawal)
5. Supportive Measures
- Psychosocial support:
- Cognitive behavioral therapy (CBT) for anxiety/insomnia
- Mindfulness, relaxation techniques
- Peer support groups (e.g., SMART Recovery)
- Sleep hygiene counseling
- Address underlying disorders (GAD, PTSD, insomnia, depression)
- Consider non-benzodiazepine alternatives:
- SSRIs/SNRIs for anxiety
- Hydroxyzine, pregabalin, gabapentin for anxiety (with caution)
- Melatonin, CBT-I for insomnia
6. Manage Withdrawal Symptoms
- Mild/moderate symptoms: reassurance, slowing taper
- Severe symptoms:
- Consider pausing the taper
- Short-term adjunct meds (e.g., beta-blockers for tremors, trazodone for sleep)
- Rarely, hospitalization may be needed (especially for seizures or suicidal ideation)
7. After Taper Completion
- Monitor for protracted withdrawal symptoms (can last weeks–months)
- Reinforce:
- Lifestyle interventions
- Continued psychiatric care
- Relapse prevention plans
- Avoid restarting benzodiazepines unless medically necessary
🔎 Conversion Example: Diazepam Equivalents (approx.)
| Drug | Approx. Equivalent to 10 mg Diazepam |
|---|---|
| Alprazolam (Xanax) | 0.5 mg |
| Lorazepam (Ativan) | 1 mg |
| Clonazepam (Klonopin) | 0.5 mg |
| Oxazepam | 15 mg |
| Temazepam | 20 mg |
Continuously individualize based on patient response.
📝 Sample Taper Example (Clonazepam 1 mg/day):
- Week 1–2: 0.75 mg/day
- Week 3–4: 0.5 mg/day
- Week 5–6: 0.375 mg/day
- Week 7–8: 0.25 mg/day
- Week 9–10: 0.125 mg/day
- Week 11–12: Discontinue
Question: Provide a patient guide for tapering Benzodiazepine dosages.
Answer: “Understanding Benzodiazepine Tapering: A Patient’s Guide to Safe Discontinuation”
🧠 What Are Benzodiazepines?
Benzodiazepines (also called “benzos”) are medications often prescribed for:
- Anxiety or panic disorders
- Sleep problems
- Seizures or muscle spasms
- Alcohol withdrawal
Examples: Alprazolam (Xanax), Lorazepam (Ativan), Diazepam (Valium), Clonazepam (Klonopin)
⚠️ Why Taper Off Benzodiazepines Slowly?
Stopping suddenly can lead to:
- Anxiety or panic attacks
- Insomnia
- Tremors or muscle cramps
- Seizures (in rare cases)
- Strong drug cravings
Tapering allows your body to adjust and helps prevent uncomfortable or dangerous withdrawal symptoms.
🕒 What to Expect in a Taper Plan
- Gradual Dose Reductions: Typically 5–25% every 1–2 weeks
- Customized Schedule: Based on your dose, how long you’ve taken it, and your health
- Medical Supervision: Your provider will adjust the plan based on your symptoms
🛠️ Tips for a Successful Taper
✅ Stick to your schedule
✅ Attend all medical appointments
✅ Track your symptoms daily
✅ Communicate openly with your provider
✅ Practice relaxation techniques (e.g., deep breathing, gentle exercise)
🧘♀️ Coping with Withdrawal Symptoms
You may feel:
- Restless or anxious
- Trouble sleeping
- Irritable or moody
- Tired or mentally foggy
Strategies:
- Use sleep hygiene practices (cool, dark room, no screens before bed)
- Avoid caffeine and alcohol
- Stay active during the day
- Reach out to supportive friends or groups
📞 When to Call Your Provider
Call if you experience:
- Severe anxiety or panic attacks
- Confusion or hallucinations
- Thoughts of self-harm or suicide
- Seizures
❤️ You Are Not Alone
Tapering is a journey toward better health. It’s okay to ask for help. You’re taking a brave step—keep going!
Question: What are the most common symptoms when tapering benzodiazepine dosages?
Answer: When tapering off benzodiazepines, patients may experience a range of withdrawal symptoms. These vary depending on the dose, duration of use, type of benzodiazepine, and individual factors (such as anxiety sensitivity and overall mental health). Here are the most common symptoms:
🔄 Psychological Symptoms
- Anxiety (often worse than before treatment)
- Irritability or agitation
- Insomnia or disturbed sleep
- Panic attacks
- Depression or low mood
- Restlessness
- Poor concentration or memory problems (“brain fog”)
😰 Physical Symptoms
- Tremors or muscle twitching
- Sweating
- Headaches
- Heart palpitations
- Nausea or stomach upset
- Dizziness or lightheadedness
- Blurred vision
👂 Sensory Disturbances
- Tinnitus (ringing in the ears)
- Numbness or tingling
- “Crawling skin” sensations (paresthesia)
- Increased sensitivity to light, sound, or touch
🧠 Severe or Rare Symptoms (usually with abrupt cessation or rapid tapering)
- Seizures
- Hallucinations
- Delirium or confusion
- Psychosis
⏳ When Do Symptoms Occur?
- Short-acting benzos (e.g., alprazolam, lorazepam): symptoms may start within 24–48 hours.
- Long-acting benzos (e.g., diazepam, clonazepam): symptoms may begin several days later.
Symptoms usually peak in the first 1–2 weeks, but milder symptoms (especially anxiety or insomnia) can last weeks to months, known as protracted withdrawal.
Conclusion
Tapering off benzodiazepines slowly is a medically necessary and ethically responsible approach to reducing dependence while minimizing withdrawal risks. Though the process can be challenging—marked by discomfort, emotional strain, and limited access to specialized care—it remains the safest path toward recovery. Addressing the ethical dilemmas of patient autonomy, informed consent, and equitable support requires thoughtful collaboration between providers, individuals, and families. By combining informed self-management, consistent family involvement, and strong community resource networks, individuals are better equipped to complete a safe taper and maintain long-term wellness beyond benzodiazepine use.
Video: Tapering Benzodiazepines