Stimulant use, including drugs like methamphetamine and cocaine, is increasingly linked to overdoses due to its dangerous effects on the body, such as cardiovascular strain and seizures. Overdose risks rise when stimulants are used in high doses or mixed with opioids like fentanyl. Stimulants are often used for energy and euphoria, but the risks are severe. Government interventions and community strategies focus on harm reduction, treatment access, and education to address this growing issue and reduce overdose rates.
Understanding the Rise in Fatal Stimulant Overdoses: Contributing Factors and Solutions
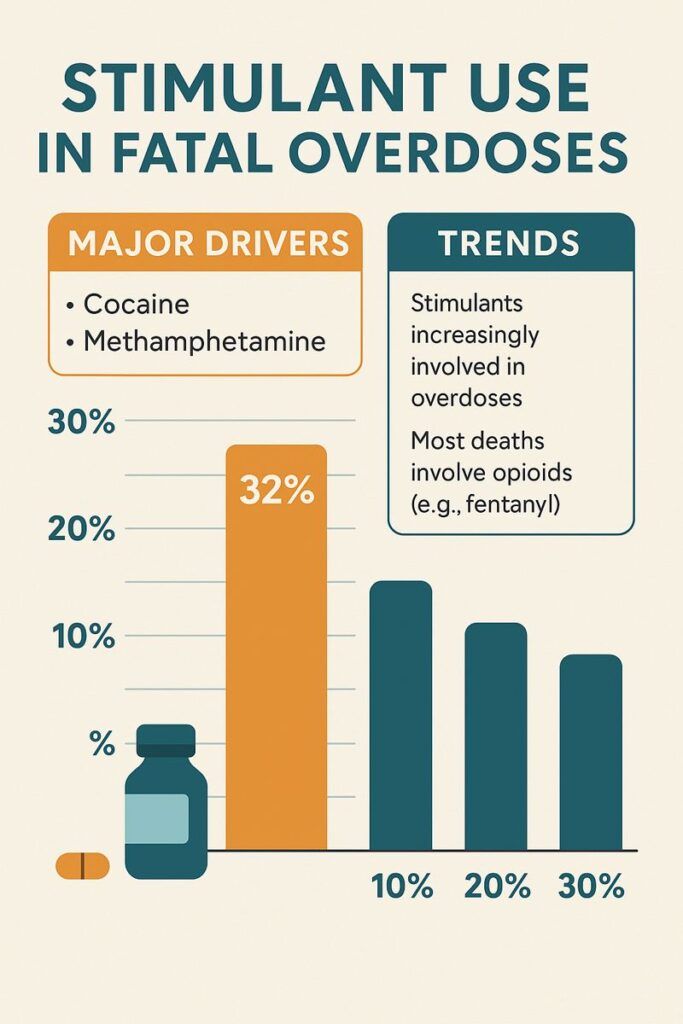
The alarming increase in fatal drug overdoses involving stimulants, particularly methamphetamine and cocaine, has become a growing public health concern. Understanding the factors driving this trend is crucial for developing effective prevention and intervention strategies. Here are the key contributors to the rise in stimulant-related overdose deaths:
1. Polydrug Use
- Combination with Opioids: Stimulants are frequently used alongside opioids, creating a dangerous combination that significantly raises the risk of overdose. The stimulating effects of drugs like cocaine or methamphetamine can mask the sedative effects of opioids, delaying the recognition of an overdose and intervention.
- Increased Potency: Stimulants can amplify the effects of other substances. When combined with opioids, the euphoric effects may be enhanced, leading users to take higher doses, further increasing the risk of overdose.
2. Changes in Drug Purity and Potency
- Unregulated Markets: Illicit stimulants vary widely in purity and potency, creating unpredictable effects. An increase in stimulant purity or unexpectedly high doses can quickly lead to fatal overdoses.
- Contamination with Fentanyl: One of the most alarming trends is the contamination of stimulants with synthetic opioids like fentanyl. Even trace amounts of fentanyl can be lethal, and many users may be unaware that the stimulant they are using is tainted, leading to accidental overdoses.
3. Physiological Effects
- Cardiovascular Risks: Stimulants place extreme stress on the cardiovascular system, increasing the risk of heart attacks, strokes, and other fatal conditions. High doses or chronic use of methamphetamine or cocaine can significantly heighten these risks.
- Neurotoxicity: Chronic stimulant use can lead to neurotoxicity, causing irreversible damage to the brain and nervous system. This can result in severe neurological and psychological complications, contributing to long-term health risks and fatal outcomes.
4. Lack of Treatment and Support
- Limited Access to Treatment: Unlike opioid use disorder, for which medication-assisted treatment (MAT) is well-established and effective, treatments for stimulant use disorder are less available. This lack of comprehensive treatment options means fewer individuals receive the help they need, increasing the likelihood of continued use and overdose.
- Stigma: Stimulant use is heavily stigmatized, often discouraging individuals from seeking help. This stigma, combined with limited treatment options, leaves many individuals without the support needed to overcome their addiction.
5. Behavioral and Psychological Factors
- Risky Behaviors: Stimulant use is associated with increased risky behaviors, such as engaging in unsafe practices, taking other drugs, or using excessive amounts. These behaviors pose a risk of dangerous or fatal outcomes.
- Mental Health Issues: Stimulants can exacerbate or trigger severe mental health issues, including paranoia, psychosis, or extreme anxiety. These mental health challenges complicate treatment and increase the likelihood of overdose and fatal outcomes.
6. Inadequate Harm Reduction
- Lack of Harm Reduction Resources: Harm reduction initiatives, such as needle exchange programs and supervised consumption sites, have been more focused on opioid use. Fewer resources exist specifically for stimulant users, leaving a significant gap in efforts to prevent overdose and provide support.
7. Evolving Drug Markets
- Drug Market Changes: The rapid evolution of the drug market presents additional challenges. The emergence of new synthetic stimulants and the increasing potency of traditional drugs like methamphetamine complicate efforts to reduce overdoses. These market changes make it more difficult for users and healthcare providers to predict the risks of specific substances.
The rise in fatal drug overdoses involving stimulants is the result of a complex interplay of factors, including polydrug use, unregulated drug purity, significant physiological effects, and inadequate treatment and harm reduction resources. To address this growing crisis, a multifaceted approach is needed, which includes expanding treatment options, improving harm reduction strategies, and raising public awareness about the risks of stimulant use. By tackling these issues, communities can help reduce overdose deaths and offer better support to individuals struggling with stimulant addiction.
Understanding Stimulants Linked to Increased Risk of Fatal Drug Overdoses
Several stimulants are commonly associated with a heightened risk of fatal drug overdoses, each posing unique dangers. Below is an overview of these stimulants and the risks they carry:
1. Methamphetamine
- Description: Methamphetamine is a potent, highly addictive stimulant that affects the central nervous system. Known for its intense and long-lasting effects, it is often associated with severe physical and mental health consequences.
- Risks: Methamphetamine use can lead to critical cardiovascular issues like heart attacks and strokes, as well as significant neurological damage. Overdoses may result in seizures, hyperthermia (dangerously high body temperature), and organ failure.
2. Cocaine
- Description: Derived from coca leaves, cocaine is a powerful stimulant. It is used in various forms, including powder cocaine and crack cocaine, both of which carry severe risks.
- Risks: Cocaine use is closely linked to cardiovascular issues such as heart attacks, arrhythmias (irregular heartbeats), and strokes. Overdose symptoms can include seizures, extremely high blood pressure, and hyperthermia, all of which can be fatal without immediate intervention.
3. Ecstasy (MDMA)
- Description: MDMA, commonly known as ecstasy, is a synthetic stimulant often used recreationally for its mood-enhancing and empathogenic effects.
- Risks: MDMA can cause severe dehydration, hyperthermia, and dangerous electrolyte imbalances, which may lead to organ failure. Additionally, users often combine MDMA with other substances, increasing the likelihood of overdose and fatal complications.
4. Synthetic Stimulants (e.g., Bath Salts)
- Description: Synthetic stimulants, often marketed as “bath salts,” are chemically similar to amphetamines but have highly unpredictable and dangerous effects.
- Risks: These substances can cause extreme agitation, hallucinations, and violent behavior, as well as severe cardiovascular and neurological issues such as heart attacks, strokes, and seizures. The unpredictable potency and effects make overdose a significant risk.
5. Prescription Stimulants (e.g., Amphetamines)
- Description: Prescription stimulants like amphetamines and methylphenidate are typically prescribed to treat ADHD, but are sometimes misused for their stimulating effects.
- Risks: Misuse of these medications can lead to cardiovascular problems, including high blood pressure and increased heart rate. Overdose can cause severe agitation, paranoia, and life-threatening seizures. Long-term misuse also increases the risk of addiction and fatal outcomes.
6. Ephedrine and Pseudoephedrine
- Description: Found in certain over-the-counter medications, ephedrine and pseudoephedrine are stimulants that can also be used to manufacture methamphetamine.
- Risks: Misuse of these substances can lead to cardiovascular complications such as hypertension and tachycardia (rapid heart rate), as well as strokes. Overdose can cause hyperthermia and seizures, contributing to fatal outcomes if untreated.
Stimulants like methamphetamine, cocaine, ecstasy (MDMA), synthetic stimulants, prescription stimulants, and substances like ephedrine are associated with a heightened risk of fatal drug overdoses. These drugs pose severe cardiovascular and neurological risks, and their misuse—especially in combination with other medications—dramatically elevates the chance of overdose and death. Addressing the rising overdose crisis requires prevention strategies, expanded treatment options, and harm reduction initiatives to mitigate the risks associated with these powerful and often dangerous substances.
Why Stimulants Are Used in Substance Use Disorders: Key Factors and Challenges
Stimulants are frequently used or misused in the context of substance use disorders (SUDs) for a variety of reasons. These include pursuing pleasurable effects, self-medication, and social influences. Here’s a breakdown of the critical factors driving stimulant use in SUDs:
1. Euphoria and Reward
- Desired Effects: Stimulants produce intense euphoria, increased energy, and heightened alertness. For individuals struggling with negative emotions or depression, these effects can be highly appealing as a way to improve their mood or escape daily struggles.
- Reinforcement: The pleasurable effects of stimulants can reinforce their continued use, eventually leading to addiction as individuals chase the same highs.
2. Self-Medication
- Coping Mechanism: Some individuals use stimulants as a form of self-medication to manage underlying mental health conditions such as anxiety or depression. They may find that stimulants temporarily improve their mood or help them feel more in control.
- Managing Fatigue: Stimulants are often misused to counteract fatigue or lethargy, especially when these symptoms are the result of other substance use, mental health conditions, or lifestyle factors.
3. Social and Recreational Use
- Peer Influence: Social settings often play a significant role in stimulant use, particularly among younger individuals. Stimulants can enhance social experiences by making users feel more energized and sociable, which may lead to misuse in social circles.
- Party and Club Scenes: Drugs like MDMA (ecstasy) are famous in party or club environments due to their stimulating effects, which heighten sensory perceptions and increase enjoyment in social or recreational settings.
4. Performance Enhancement
- Academic or Work Performance: Prescription stimulants, such as amphetamines, are sometimes misused by students or professionals to boost focus, cognitive function, and productivity, especially under pressure to meet academic or work-related demands. This misuse can lead to dependence and substance use disorders.
5. Polydrug Use
- Combination with Other Substances: Many individuals combine stimulants with other drugs, such as opioids or alcohol, to either alter or enhance the effects of the primary drug. This polydrug use can be dangerous and increase the risk of overdose.
- Synergistic Effects: When stimulants are combined with depressants or other substances, the effects of one drug may mask the symptoms of overdose from another, leading to dangerous and potentially fatal interactions.
6. Addiction and Dependence
- Tolerance and Dependence: Regular stimulant use can lead to tolerance, requiring individuals to take higher doses to achieve the same effects. Over time, this can contribute to addiction and exacerbate the substance use disorder.
- Withdrawal Symptoms: Individuals dependent on stimulants often experience withdrawal symptoms such as fatigue, depression, and intense cravings when they try to stop, which can prompt further use to avoid discomfort.
7. Availability and Accessibility
- Illicit Market: Stimulants like methamphetamine and cocaine are widely available on the illicit market, making them more accessible to individuals at risk of substance use disorders. Easy access increases the likelihood of misuse and dependence.
8. Psychological and Social Factors
- Mental Health Issues: Many individuals with underlying mental health conditions are drawn to stimulants as a way to self-manage their symptoms, which can complicate their substance use disorder.
- Social Environment: A person’s social and environmental context, including community norms and peer behavior, can significantly influence the likelihood of using stimulants and developing a substance use disorder.
Stimulants are commonly used in substance use disorders due to their euphoric effects, self-medication appeal, and social and performance-related pressures. The interplay between psychological, social, and environmental factors, along with the dangers of polydrug use, makes addressing stimulant misuse a complex challenge. To effectively combat stimulant use disorders, interventions must consider these varied influences and the unique challenges they present in the context of addiction.
How Stimulants Contribute to Drug Overdoses: Understanding the Risks
Stimulants can lead to fatal drug overdoses through various mechanisms that impact both the body and the brain. Here’s how stimulant use increases the risk of overdose:
1. Cardiovascular Strain
- Increased Heart Rate and Blood Pressure: Stimulants like methamphetamine, cocaine, and amphetamines significantly elevate heart rate and blood pressure, placing immense strain on the cardiovascular system. This can result in heart attacks, strokes, and cardiac arrest, especially with chronic use or high doses.
- Arrhythmias: Stimulants can disrupt normal heart rhythm, leading to dangerous arrhythmias. When combined with other substances, such as alcohol or opioids, the risk of fatal heart complications increases.
2. Hyperthermia (Overheating)
- Elevated Body Temperature: Stimulants raise core body temperature, and excessive use can lead to hyperthermia (dangerous overheating). In situations like parties or crowded environments where users are active, this can result in organ failure, brain damage, or even death.
3. Seizures
- Overstimulation of the Brain: High doses of stimulants can cause seizures by overstimulating the brain. These seizures can be life-threatening, especially when combined with cardiovascular strain or dehydration, which is common in stimulant users.
4. Respiratory Failure
- The strain on the Respiratory System: Stimulants can strain the respiratory system. At high doses or when mixed with depressants like opioids or alcohol, this can lead to breathing difficulties, hypoxia (lack of oxygen to the brain), and potentially fatal respiratory failure.
5. Polydrug Use
- Mixing with Opioids: Combining stimulants with opioids, such as heroin or fentanyl, is extremely dangerous. Stimulants speed up the body’s systems, while opioids depress them. This can mask overdose symptoms, leading to unintentional overdoses and death from respiratory depression after the stimulant wears off.
- Delayed Recognition of Overdose: Stimulants can hide the sedative effects of opioids, slowing recognition of overdose symptoms and increasing the risk of fatal outcomes.
6. Impaired Judgment and Risky Behavior
- Higher Doses Due to Impaired Judgment: Stimulants can impair decision-making, causing users to take higher doses than intended, which increases the risk of accidental overdose.
- Risk-Taking Behavior: Stimulants often promote risky behavior, such as dangerous drug combinations or unintentional high doses, heightening the chance of overdose.
7. Drug Potency and Contamination
- Unpredictable Potency: The strength of illicit stimulants like methamphetamine or cocaine can vary significantly, leading to accidental overdoses when users encounter unexpectedly potent batches.
- Fentanyl Contamination: Illicit stimulant drugs are often contaminated with fentanyl, a powerful opioid responsible for many overdose deaths. Users may not realize this contamination, leading to unintentional opioid overdoses.
8. Chronic Use and Tolerance
- Increasing Tolerance: Chronic users develop tolerance to stimulants, requiring higher doses to feel the same effects. This escalates the risk of overdose as users push their bodies beyond safe limits.
- Binge Use: Some users engage in binge use, consuming large quantities of stimulants in a short time. This overwhelms the body’s ability to cope with the drug’s effects, significantly increasing the likelihood of overdose.
Stimulants contribute to overdoses through cardiovascular strain, hyperthermia, seizures, and respiratory failure. The risks are magnified when stimulants are used in combination with other substances, such as opioids, or when users face unpredictable drug potency. Understanding these mechanisms is crucial for prevention and harm reduction efforts aimed at reducing stimulant-related overdose deaths.
Government Strategies to Combat Stimulant-Related Overdoses: A Comprehensive Approach
The rising crisis of stimulant-related drug overdoses demands a multifaceted approach from governments, focusing on regulation, harm reduction, treatment access, and public health education. Here are key strategies that governments can implement to tackle the growing stimulant overdose issue:
1. Expanding Access to Harm Reduction Services
- Safe Consumption Spaces: Governments can establish or support safe consumption spaces where individuals can use stimulants under medical supervision. These spaces can provide immediate intervention in the event of an overdose and reduce the risks associated with unsupervised drug use.
- Syringe Exchange Programs: By offering sterile syringes, these programs help reduce the transmission of diseases like HIV and hepatitis C among stimulant users. They also serve as crucial touchpoints for overdose prevention information.
- Fentanyl Testing Kits: Given the increasing contamination of stimulants with fentanyl, providing fentanyl testing kits allows users to check for opioid contamination, thus mitigating the risk of accidental overdose.
2. Public Health Campaigns and Education
- Public Awareness Campaigns: Government-led campaigns can educate the public on the risks of stimulant use, including overdose and polydrug use. These campaigns should emphasize recognizing overdose signs, safe use practices, and the availability of naloxone for opioid overdoses.
- Stigma Reduction Initiatives: Reducing stigma around stimulant use encourages individuals to seek treatment without fear of judgment. Government-supported programs can help shift societal attitudes toward addiction as a medical condition rather than a moral failing.
3. Increasing Access to Treatment for Stimulant Use Disorder
- Expanding Treatment Programs: Investing in evidence-based treatment options, such as cognitive-behavioral therapy (CBT) and contingency management, can improve access to adequate care for stimulant use disorders.
- Funding for Research: Increased funding for research can drive the development of new pharmacological treatments for stimulant addiction, addressing the current treatment gap compared to opioid addiction.
- Telemedicine Access: Expanding telemedicine options can improve accessibility to addiction treatment for individuals in rural or underserved areas, preventing the escalation of drug use to dangerous levels.
4. Addressing Polydrug Use
- Naloxone Distribution: Providing naloxone widely can help reverse opioid overdoses, especially in cases where stimulants are contaminated with fentanyl. This can prevent fatal outcomes from polydrug use.
- Integrated Polydrug Use Programs: Promoting integrated treatment programs that address both stimulant and opioid use disorders can more effectively support individuals who use multiple substances.
5. Strengthening Law Enforcement and Regulation
- Targeting Trafficking: Governments can intensify law enforcement efforts to disrupt the supply of illegal stimulants through international cooperation, more robust border controls, and cracking down on trafficking operations.
- Regulating Precursor Chemicals: Implementing stricter regulations on chemicals used to manufacture stimulants, such as pseudoephedrine, can help prevent their illicit production and distribution.
- Enhanced Drug Surveillance: Improving drug surveillance systems can help identify new, potent stimulant drugs and track drug-use trends, enabling timely responses.
6. Expanding Mental Health and Social Support
- Dual Diagnosis Treatment: Investing in programs that offer both mental health care and addiction treatment can address co-occurring disorders, which are common among stimulant users.
- Social Support Programs: Increasing access to housing, employment, and social services can tackle underlying issues like poverty and homelessness, which contribute to stimulant misuse. These programs can support long-term recovery and reduce relapse rates.
7. Monitoring and Early Intervention
- Screening in Healthcare Settings: Encouraging or mandating screening for stimulant use in primary care and emergency settings can lead to early identification and intervention before misuse escalates to overdose.
- Public Health Monitoring: Enhancing data collection on stimulant-related overdoses can help identify emerging trends, at-risk populations, and geographical hotspots, guiding targeted interventions.
8. Legal and Policy Reforms
- Decriminalization of Drug Use: Exploring the decriminalization of small amounts of drug possession can shift the focus to public health approaches rather than criminalization. This can reduce stigma and encourage users to seek treatment.
- Good Samaritan Laws: Strengthening Good Samaritan laws ensures that individuals who seek help during an overdose are not penalized, encourages timely emergency assistance, and saves lives.
Addressing stimulant-related overdoses requires a comprehensive, multi-pronged approach from governments. By expanding harm reduction services, improving treatment access, addressing polydrug use, and promoting public education, governments can mitigate the risks associated with stimulant use. A combined focus on social, legal, and healthcare aspects will be crucial in reducing stimulant-related overdose deaths and improving public health outcomes.
Community Resource Strategies for Decreasing Stimulant Use and Preventing Overdoses
Addressing stimulant use and preventing overdose requires a community-driven approach that combines harm reduction, education, and accessible treatment. By implementing comprehensive strategies, communities can create supportive environments that reduce stimulant misuse and improve public health. Here’s an overview of effective community resource strategies:
1. Harm Reduction Programs
- Syringe Exchange Programs: These programs provide clean needles to reduce the spread of diseases among stimulant users who inject drugs. They also offer crucial services such as HIV and hepatitis testing and referrals to treatment resources.
- Fentanyl Testing Kits: To combat the increasing contamination of stimulants with fentanyl, communities can distribute fentanyl test strips. These kits help users identify the presence of fentanyl in their stimulant supply, reducing the risk of accidental overdose.
- Naloxone Distribution: While primarily used to reverse opioid overdoses, naloxone is essential for stimulant users who may encounter fentanyl. Ensuring widespread availability of naloxone can save lives in the event of a polydrug overdose.
2. Peer Support Networks
- Peer Recovery Coaches: Implementing programs where individuals who have successfully recovered from stimulant addiction serve as peer recovery coaches can provide valuable guidance and emotional support to those currently struggling.
- Support Groups: Community-based support groups like Narcotics Anonymous (NA) or Crystal Meth Anonymous (CMA) offer safe spaces for individuals to share experiences, learn coping strategies, and find accountability in their recovery journey.
3. Education and Outreach Initiatives
- Public Awareness Campaigns: Educational campaigns can raise awareness about the risks of stimulant use, overdose prevention, and safer drug use practices. These campaigns should target high-risk populations through schools, social media, and community events.
- Workshops for At-Risk Groups: Hosting educational workshops in schools, community centers, and shelters can inform vulnerable populations about the dangers of stimulant use and the available resources for prevention and treatment.
4. Accessible Treatment and Counseling Services
- Low-Barrier Treatment Programs: Offering low-barrier access to evidence-based therapies for stimulant use disorder, such as contingency management and cognitive-behavioral therapy (CBT), ensures that treatment is available to those in need, regardless of financial constraints.
- Telehealth Services: Expanding telehealth services allows individuals in rural or underserved areas to access addiction counseling and mental health services remotely, improving treatment accessibility.
5. Mental Health and Dual Diagnosis Services
- Integrated Mental Health Care: Many stimulant users have co-occurring mental health disorders. Integrating mental health services with addiction treatment can address both conditions simultaneously and enhance overall recovery outcomes.
- Trauma-Informed Care: Providing trauma-informed care in community health centers helps address underlying trauma, which often contributes to substance use, and creates a supportive environment for recovery.
6. Employment and Housing Support
- Job Training and Employment Services: Economic instability is often linked to stimulant use. Offering job training programs and employment services can help individuals find stable work, reduce the risk of relapse, and support long-term recovery.
- Housing First Programs: Stable housing is crucial for recovery. Housing First programs provide housing without preconditions, allowing individuals to focus on their recovery while securing a safe living environment.
7. Youth and Prevention Programs
- School-Based Prevention Programs: Implementing early intervention and prevention programs in schools can educate young people about the risks of stimulant use and prevent initiation. Programs like DARE or evidence-based models can be effective.
- After-School and Community Activities: Providing recreational and extracurricular activities for youth can offer positive alternatives to drug use and engage at-risk individuals in constructive behaviors.
8. Legal and Advocacy Efforts
- Advocating for Decriminalization: Communities can support decriminalizing small amounts of drug possession, focusing on treatment rather than punishment. This approach can reduce stigma and encourage users to seek help without fear of legal consequences.
- Good Samaritan Policies: Promoting and enforcing Good Samaritan laws ensures that individuals who seek medical help during an overdose are protected from legal repercussions, encouraging more people to call for emergency assistance.
9. Community-Based Policing and Diversion Programs
- Law Enforcement and Treatment Diversion: Instead of arresting individuals for stimulant possession, law enforcement can collaborate with community health services to divert them into treatment programs. Initiatives like Law Enforcement Assisted Diversion (LEAD) connect individuals with resources rather than the criminal justice system.
- Community Engagement: Strengthening connections among law enforcement, community organizations, and residents can build trust and ensure that individuals who use stimulants receive care and support rather than punishment.
10. Collaboration with Healthcare Providers
- Early Screening and Intervention: Community health centers and clinics can screen for stimulant use and provide early intervention, particularly for high-risk populations like those experiencing homelessness or mental health issues.
- Training for Healthcare Workers: Training healthcare workers to recognize stimulant use disorders and respond to crises can improve the quality of care and ensure that patients are connected to appropriate resources.
Community resource strategies for decreasing stimulant use and preventing overdoses require a holistic approach that combines harm reduction, accessible treatment, mental health services, and education. By fostering strong peer networks, providing support services, and advocating for policy changes, communities can create environments that promote recovery and reduce the risk of stimulant-related overdoses. These efforts are crucial in building a supportive network that empowers individuals to seek help and achieve long-term recovery.
Frequently Asked Questions
Here are some common questions:
Q: Can stimulants alone cause fatal overdoses?
A: Yes. High doses of stimulants can cause fatal heart rhythm disturbances, strokes, hyperthermia, and organ failure, even without opioids present.
Q: What is polysubstance use, and why is it dangerous?
A: Polysubstance use means using more than one drug at a time, such as stimulants with opioids or alcohol. Combined effects significantly increase overdose risk and complicate treatment.
Q: Are overdose signs different for stimulants?
A: Yes. Stimulant overdoses may include chest pain, agitation, overheating, seizures, or irregular heartbeat. When fentanyl is involved, slowed breathing or unconsciousness may occur.
Conclusion
Stimulants such as methamphetamine and cocaine are commonly used for their energizing and euphoric effects. Still, they carry significant overdose risks, mainly when used in high doses or mixed with other substances like fentanyl. These drugs cause severe strain on the cardiovascular system, leading to life-threatening conditions like seizures and heart failure. To combat the rising stimulant-related overdoses, government interventions focus on harm reduction, improved access to treatment, and public education. Community resource strategies, including support networks and mental health care, are essential in preventing stimulant misuse and fostering healthier, safer environments for individuals at risk.
Video: Stimulant Use in Fatal Overdoses