Sexual misconduct in addiction treatment facilities is a serious issue that targets vulnerable individuals in recovery. Patients may face trauma, power imbalances, and emotional instability, increasing their risk. Prevention relies on self-management strategies like boundary-setting, strong family advocacy and communication, and community resources such as oversight agencies and reporting systems. These combined efforts help ensure a safe and ethical treatment environment.
Sexual Misconduct in Addiction Treatment Centers: A Hidden Threat to Recovery
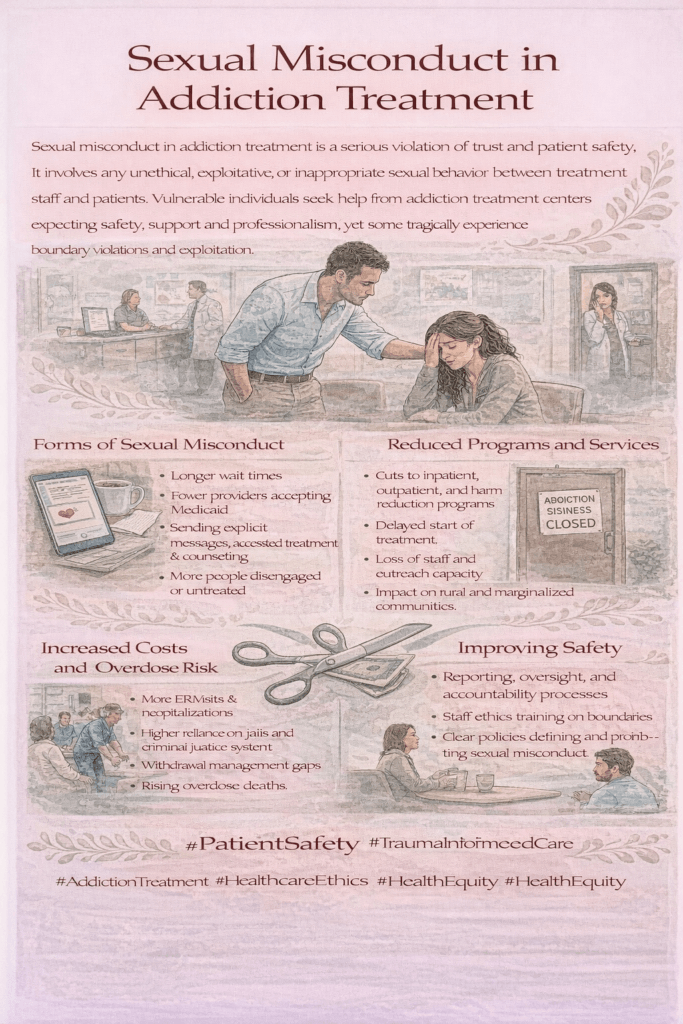
Sexual misconduct in addiction treatment centers refers to any inappropriate, unethical, or non-consensual sexual behavior committed by staff, fellow patients, or visitors within the treatment setting. This misconduct can cause deep harm—undermining recovery, damaging mental health, and shattering trust in the healthcare system.
Types of Sexual Misconduct
- Staff-to-Patient Misconduct
- Unwanted sexual advances or comments
- Inappropriate physical contact
- Sexual relationships (even if they appear “consensual”)—unethical due to power imbalances
- Exploiting a patient’s vulnerability for sexual gain
- Patient-to-Patient Misconduct
- Non-consensual touching or harassment
- Sexual coercion or manipulation during treatment
- Exploiting someone impaired by withdrawal, medications, or trauma
- Abuse of Authority or Privilege
- Threatening to withhold treatment or support unless sexual favors are granted
- Offering special privileges in exchange for sexual activity
Why It’s Especially Harmful in Addiction Treatment
- Patients are vulnerable—often dealing with withdrawal, trauma, mental health struggles, or dependency on care providers.
- Misconduct can trigger past abuse or trauma, which is tragically common among people with substance use disorders.
- It violates ethical standards and can lead to relapse, dropping out of treatment, or long-term psychological harm.
Prevention and Accountability
- Facilities must enforce strict policies, require staff training, and provide clear reporting procedures.
- Licensing boards and accrediting bodies (such as The Joint Commission) mandate zero-tolerance policies.
- Survivors need trauma-informed care, legal advocacy, and emotional support to heal.
💡 Bottom line: Recovery spaces should be the safest environments possible. Sexual misconduct not only violates human dignity but also threatens the very purpose of treatment—healing, trust, and hope.
Why People in Addiction Treatment Are Especially Vulnerable to Sexual Misconduct
People in addiction treatment face a unique set of risks when it comes to sexual misconduct within treatment facilities. A combination of psychological, social, and situational factors can weaken their ability to protect themselves or advocate for their rights—making strong safeguards essential.
1. Power Imbalances
- Staff and authority figures—such as counselors, doctors, and nurses—control vital aspects of patients’ treatment, housing, and daily routines.
- This imbalance can be exploited, especially if patients fear losing access to care or support.
2. Psychological Vulnerability
- Many enter treatment during an emotional crisis, often coping with withdrawal, trauma, shame, or low self-worth.
- Such distress can make it harder to set healthy boundaries or recognize manipulative behavior.
3. Histories of Trauma
- A large number of people with substance use disorders have experienced sexual, physical, or emotional abuse in the past.
- Without proper safeguards, these histories can make them more susceptible to being victimized again.
4. Impaired Decision-Making
- Early recovery and detox can impair judgment, making it harder to identify red flags or assert personal boundaries.
- Withdrawal symptoms, medications, and mental health challenges can further cloud awareness and the ability to consent.
5. Isolation and Dependency
- Residential treatment often separates patients from family, friends, and outside support systems.
- This isolation can lead to dependency on staff or peers—something that can be exploited by individuals with harmful intentions.
6. Shame and Fear of Retaliation
- Survivors may fear disbelief, retaliation, or being blamed for the abuse.
- This fear often keeps misconduct hidden, allowing it to persist without consequences.
In summary, the heightened vulnerability of people in addiction treatment comes from a mix of emotional fragility, past trauma, and reliance on caregivers. That’s why treatment centers must maintain strict professional boundaries, mandatory staff training, and strong patient protection protocols—not only to prevent misconduct but to ensure a safe environment where proper recovery is possible.

Self-Management Strategies to Stay Safe from Sexual Misconduct in Addiction Treatment
Self-management strategies can help individuals in addiction treatment recognize, avoid, and respond to sexual misconduct—even in vulnerable situations. While it is never the victim’s fault, learning these skills can help protect personal boundaries and promote safety.
1. Know Your Rights
- Understand your rights as a patient, including the right to respectful, non-exploitative care and to report concerns without retaliation.
- Most treatment facilities are required by law and accreditation standards to maintain zero-tolerance policies for abuse or harassment.
2. Understand Professional Boundaries
- Staff should never engage in personal or sexual relationships with patients—no matter how “consensual” it might appear.
- Watch for early warning signs, such as private contact information, gifts, or unnecessary physical touch.
3. Build Assertiveness Skills
- Practice saying “no” clearly and confidently when someone crosses a boundary.
- Consider assertiveness training or peer role-playing in group therapy to strengthen this skill.
4. Report Early Warning Signs
- Document and report uncomfortable behaviors immediately—such as inappropriate jokes, touching, or private invitations.
- Use both internal facility reporting systems and external hotlines if needed.
5. Stay Connected to Outside Supports
- Keep in touch with trusted family members, friends, or outside sponsors.
- These connections can help you process concerns and take action if something feels wrong.
6. Use Peer Allies and Group Support
- Share concerns with peers or patient advocates—others may have noticed similar issues and can help validate or report them.
7. Be Informed and Observant
- Notice how staff interact with other patients. Patterns of favoritism, secrecy, or repeated rule-breaking may be signs of misconduct.
8. Keep a Personal Journal (If Safe)
- Record concerning interactions with dates, times, and details. This documentation can be vital for formal complaints or investigations.
In summary, it is never a patient’s responsibility to prevent abuse. The duty to provide a safe environment lies with the treatment facility. However, self-management strategies can empower individuals to recognize risks, set boundaries, and speak up—helping protect their recovery journey.
Family Support: A Key Safeguard Against Sexual Misconduct in Addiction Treatment
Family involvement is one of the most effective ways to protect loved ones in addiction treatment facilities from sexual misconduct. When families remain engaged, informed, and proactive, they can act as advocates, protectors, and watchdogs—helping ensure a safe recovery environment.
1. Stay Involved in the Treatment Process
- Participate in family therapy sessions, visitation days, and treatment planning meetings whenever possible.
- Maintain regular contact through calls, check-ins, or video visits to stay aware of your loved one’s emotional and physical well-being.
2. Educate Yourself on Patient Rights and Facility Policies
- Learn the facility’s code of conduct, grievance procedures, and ethical standards.
- Understand how to report concerns both internally and to outside oversight agencies.
3. Encourage Open, Judgment-Free Communication
- Create a safe space where your loved one can share concerns without fear of blame or disbelief.
- Use open-ended questions such as, “How are you feeling about the staff and other residents?” or “Do you feel safe there?”
4. Watch for Red Flags
- Be alert to sudden mood changes, withdrawal from communication, reluctance to discuss treatment, or vague comments suggesting discomfort.
- Take these signs seriously, even if your loved one minimizes them.
5. Advocate for Transparency and Accountability
- Speak up if something feels wrong—contact facility leadership or licensing boards.
- Request staff credentials and ask how boundaries and safety protocols are enforced.
6. Encourage Self-Advocacy
- Support your loved one in knowing their rights, setting boundaries, and reporting inappropriate behavior.
- Reassure them that they are not alone and that they have the right to speak up.
7. Utilize Outside Resources
- Reach out to patient advocacy groups, legal aid organizations, or local ombudsmen if you suspect abuse.
- Suggest confidential support hotlines for immediate, private assistance.
8. Choose Accredited and Reputable Facilities
- Whenever possible, select centers that are licensed, accredited (e.g., by CARF or The Joint Commission), and known for enforcing strict patient safety policies.
In summary, families are powerful allies in preventing sexual misconduct in addiction treatment. By staying informed, observant, and supportive, you can help ensure your loved one’s recovery takes place in a safe and respectful environment—free from harm and grounded in dignity.
Community Strategies to Prevent Sexual Misconduct in Addiction Treatment
Community resources play a crucial role in preventing sexual misconduct in addiction treatment facilities. By promoting accountability, oversight, education, and support, these strategies help ensure treatment environments are safe, ethical, and trauma-informed for every patient.
1. Licensing and Accreditation Oversight
- State health departments and licensing boards monitor facilities to ensure compliance with safety and ethical standards.
- Accreditation bodies such as The Joint Commission and CARF require clear policies to prevent abuse and maintain professional boundaries.
2. Patient Advocacy Organizations
- Groups such as NAMI, SAMHSA grantees, and local ombudsman programs provide confidential resources for patients and families to report misconduct and seek support.
- They also help educate the public about patient rights and assist with navigating complaints or legal processes.
3. Community Education and Provider Training
- Local organizations can deliver staff training on sexual harassment prevention, trauma-informed care, and ethical boundaries.
- Community programs can also educate clients and families about recognizing, preventing, and reporting sexual misconduct.
4. Hotlines and Reporting Systems
- Anonymous or third-party hotlines allow patients and families to report misconduct without fear of retaliation.
- Reports can trigger external investigations and facility audits to address concerns quickly.
5. Peer and Recovery Support Networks
- Recovery groups and sober living coalitions create safe peer spaces for survivors to share concerns and receive support.
- Peer mentors can guide individuals through treatment systems, helping them navigate safely and confidently.
6. Collaboration with Legal and Advocacy Services
- Legal aid organizations and civil rights groups can provide representation and ensure that facilities are held accountable when misconduct occurs.
7. Community-Based Monitoring Programs
- Oversight committees or ethics review boards can conduct unannounced visits and review patient grievance records to ensure safety and transparency.
In summary, community resources serve as critical safeguards against sexual misconduct in addiction treatment. By enforcing standards, empowering patients, educating staff, and providing safe reporting channels, these external systems strengthen transparency, accountability, and trust—ensuring recovery environments are built on respect and safety.
Frequently Asked Questions
Here are some common questions:
Question: How do addiction treatment facilities prevent sexual misconduct?
Answer: Addiction treatment facilities can prevent sexual misconduct by creating a layered system of protections that address safety from multiple angles—policies, training, monitoring, and culture.
Here’s a breakdown of standard prevention measures:
1. Clear Policies and Zero-Tolerance Rules
- Written codes of conduct outlining prohibited behaviors, boundaries, and consequences.
- Explicit zero-tolerance policy for sexual harassment, abuse, or exploitation by staff or residents.
- Rules apply to all staff, contractors, and patients, with signed acknowledgment upon intake or hiring.
2. Thorough Screening and Hiring Practices
- Background checks on all employees, volunteers, and contractors.
- Verification of professional licenses and certifications.
- Reference checks that specifically ask about prior misconduct.
3. Comprehensive Staff Training
- Mandatory training on sexual misconduct prevention, trauma-informed care, and maintaining professional boundaries.
- Education on recognizing grooming behaviors and power imbalances.
- Annual refreshers to keep staff aware and accountable.
4. Safe Facility Design and Supervision
- Security cameras in common areas (not in bathrooms or private therapy rooms).
- Adequate staffing ratios to prevent isolation of vulnerable patients.
- Policies require two staff members to be present in specific situations, such as patient transport or physical assistance.
5. Patient Education and Empowerment
- Orientation sessions explaining patient rights and how to report concerns safely.
- Posters, pamphlets, or hotline numbers are placed in visible areas.
- Encouragement to speak up without fear of retaliation.
6. Reporting and Grievance Systems
- Multiple reporting options: an anonymous hotline, a suggestion box, a direct supervisor, or an external agency.
- Clear, prompt procedures for investigating allegations.
- Written communication of outcomes when possible.
7. Continuous Oversight and Audits
- Regular unannounced visits from state licensing boards or accreditation agencies like CARF or The Joint Commission.
- Internal compliance checks and ethics reviews.
8. Culture of Safety and Respect
Open-door policies that encourage feedback from patients and staff.
Leadership models professional behavior and sets the tone for staff interactions.
Strong emphasis on boundaries, dignity, and confidentiality.
Question: What are the signs of sexual misconduct in addiction treatment facilities?
Answer: Signs of sexual misconduct in addiction treatment facilities can be subtle or overt, and they may come from either staff or other patients. Because people in treatment are often in a vulnerable state, even minor boundary violations can escalate if not addressed.
Here’s a detailed list of warning signs to look for:
1. Behavioral Changes in the Patient
- Withdrawal or isolation from group activities or specific staff members.
- Sudden loss of trust in the treatment process or refusal to participate.
- Mood swings, anxiety, depression, or increased irritability.
- Reluctance to talk during family visits or calls.
- Sudden requests to leave treatment early without clear reasons.
2. Concerning Staff or Peer Interactions
- Staff or peers spending excessive one-on-one time with a specific patient without a clinical reason.
- Flirtatious, sexualized, or overly personal comments.
- Unnecessary touching or physical contact.
- Offering special privileges or favors to one patient.
- Breaking confidentiality without cause.
3. Boundary Violations
- Staff sharing personal sexual history or asking about the patient’s sexual history outside of clinical relevance.
- Private meetings in locations that are not designated for therapy.
- Staff giving or receiving gifts from patients.
- Ignoring rules about male/female dorms or unsupervised mixed-gender activities.
4. Physical and Emotional Indicators
- Unexplained injuries or physical marks.
- Changes in sleeping or eating patterns.
- Frequent nightmares or signs of PTSD.
- Sudden drop in self-esteem or self-worth statements (“I’m worthless,” “I don’t matter”).
5. Reports, Rumors, or “Jokes.”
- Patients making offhand sexual comments about staff or peers that seem too specific to be random.
- Whispered rumors among residents about inappropriate relationships.
- “Jokes” from staff or peers that normalize sexual behavior in a treatment setting.
6. Red Flags in Facility Operations
- Lack of security cameras in public areas.
- Staff are not being supervised or monitored during patient contact.
- No clear or accessible reporting procedure.
- Retaliation or shaming when concerns are raised.
Important:
In a treatment setting, power dynamics complicate consent. Even if a patient “agrees,” sexual contact with staff is always unethical and often illegal. Peer-to-peer misconduct must also be taken seriously because of the vulnerability and trauma history common in recovery populations.
Question: How can a family member research the facility if it has a history of sexual misconduct incidents in the past?
Answer: If a family member wants to research whether an addiction treatment facility has a history of sexual misconduct incidents, they should use a combination of official records, oversight agencies, and independent resources. Here’s a step-by-step guide:
1. Check State Licensing and Regulatory Agencies
- State Health Department or Behavioral Health Licensing Board
- Most states keep public disciplinary records for licensed facilities and staff.
- Look for “disciplinary actions,” “inspection reports,” or “complaints database” on the agency’s website.
- The State Department of Health and Human Services (DHHS) often posts facility inspection reports and investigations.
- You can also call directly to ask whether there have been any substantiated incidents in the past.
2. Search Accreditation Organizations
- The Joint Commission and CARF International
- Accreditation bodies may revoke or suspend accreditation for misconduct or safety violations.
- Check their public directory and contact them to request any information on investigations.
3. Look at Court and Legal Records
- County Court Records (often available online for free) can show lawsuits against the facility or staff.
- Use keywords like the facility name + “sexual misconduct,” “abuse,” or “harassment” in court record databases.
- PACER (Public Access to Court Electronic Records) can be used for federal cases, though it may have a small fee.
4. Review News and Media Reports
- Search Google News, local news websites, or newspaper archives with:
"facility name" + "sexual misconduct""facility name" + "lawsuit"
- Local journalism often uncovers misconduct before it shows in official databases.
5. Check Advocacy and Watchdog Groups
- National Alliance on Mental Illness (NAMI), National Center on Elder Abuse, and state-level patient advocacy groups may have reports or alerts.
- Some nonprofit watchdogs maintain searchable databases of abuse in care facilities.
6. Contact the Local Ombudsman or Patient Advocate
- Ombudsman programs (especially for residential care) can tell you if there have been complaints or investigations.
- They also guide on how to file a complaint if you suspect a risk.
7. Ask the Facility Directly
Facilities with nothing to hide should answer transparently.
Request written copies of:
Code of Conduct
Safety & Boundary Policy
Incident Reporting Policy
Staff Credential Verification
Ask if they have ever had staff terminated or disciplined for boundary violations.
Conclusion
Preventing sexual misconduct in addiction treatment facilities requires recognizing patient vulnerability and addressing it through a multi-layered approach. Empowering individuals with self-management skills, engaging families in advocacy and oversight, and leveraging community resources for education, regulation, and reporting are all essential. Together, these strategies help create a safer, more respectful environment where recovery can truly take place.
Video: The Hidden DANGER of Sexual Abuse in Recovery Programs