Seasonal mental health conditions can lead to substance abuse as individuals seek relief from depression or anxiety. Self-care, family support, and community resources, along with healthy routines, therapy, and emotional stability from loved ones, can help, while mental health services and support groups provide essential guidance. Together, these strategies reduce substance use and promote well-being during seasonal changes.
Understanding Seasonal Mental Health Disorders and Their Impact
Seasonal mental health issues refer to mental health conditions that fluctuate or worsen depending on the time of year or specific seasonal changes. These conditions are typically linked to environmental factors, such as changes in daylight, temperature, or social activities. Some of the most common seasonal mental health issues include:
1. Seasonal Affective Disorder (SAD)
- What it is: SAD is a type of depression that typically occurs during the fall and winter months when there is less natural sunlight. It is believed to be related to changes in sunlight exposure, which can affect mood-regulating neurotransmitters like serotonin.
- Symptoms: Low energy, irritability, social withdrawal, changes in appetite (often cravings for carbohydrates), weight gain, difficulty concentrating, and sleep disturbances (typically oversleeping).
2. Winter Blues
- What it is: Similar to SAD, but less severe, the “winter blues” refers to mild mood disturbances that can occur when the days shorten in the fall and winter. While not a full-blown disorder, it may still lead to feelings of sadness or lethargy.
- Symptoms: Feeling down, lack of motivation, tiredness, and reduced interest in activities that are usually enjoyable.
3. Summer Depression
- What it is: While less common than SAD, some individuals experience depression during the warmer months, often referred to as summer depression or reverse SAD. This may be related to factors such as increased social pressure, higher temperatures, or a lack of a structured routine.
- Symptoms: Insomnia, agitation, anxiety, irritability, and a general sense of restlessness or discomfort.
4. Post-Vacation Syndrome
- What it is: A temporary form of depression or anxiety that can occur after returning from a vacation or break. The transition from relaxation back to routine, stress, or returning to an overwhelming workload can trigger these feelings.
- Symptoms: Low mood, fatigue, increased stress, difficulty concentrating, and feelings of dread about returning to everyday life.
5. Mood Changes with Weather
- What it is: Some individuals are susceptible to weather patterns, including prolonged cloudy or rainy days, or very hot or cold weather. These changes can influence mood and energy levels.
- Symptoms: Mild depression, irritability, low energy, or feeling “off” due to weather conditions.
Contributing Factors:
Lack of Sunlight
- Reduced exposure to sunlight, particularly in the winter months, can disrupt circadian rhythms and affect vitamin D levels, which may impact mood and overall mental health.
Change in Routine
- Seasonal changes can lead to disruptions in daily routines, which can contribute to mental health challenges.
Social and Cultural Factors
- Holidays, family dynamics, or changes in social activities during different seasons can either positively or negatively affect mental health.
Management and Treatment:
Light Therapy
- Particularly for SAD, light therapy using a specialized bright light box can help simulate natural sunlight and improve mood.
Exercise
- Regular physical activity can boost mood by increasing endorphin production.
Cognitive Behavioral Therapy (CBT)
- This can help individuals cope with the symptoms of seasonal mental health issues, particularly for those dealing with SAD or winter blues.
Social Support
- Staying connected with friends, family, or support groups can help prevent isolation, especially during the winter months.
Vitamin D Supplements
- Since sunlight exposure can lower vitamin D levels, supplementation may be recommended to improve mood during darker months.
Understanding these seasonal changes and how they affect mental health can help individuals take proactive steps to manage symptoms and seek appropriate treatment.
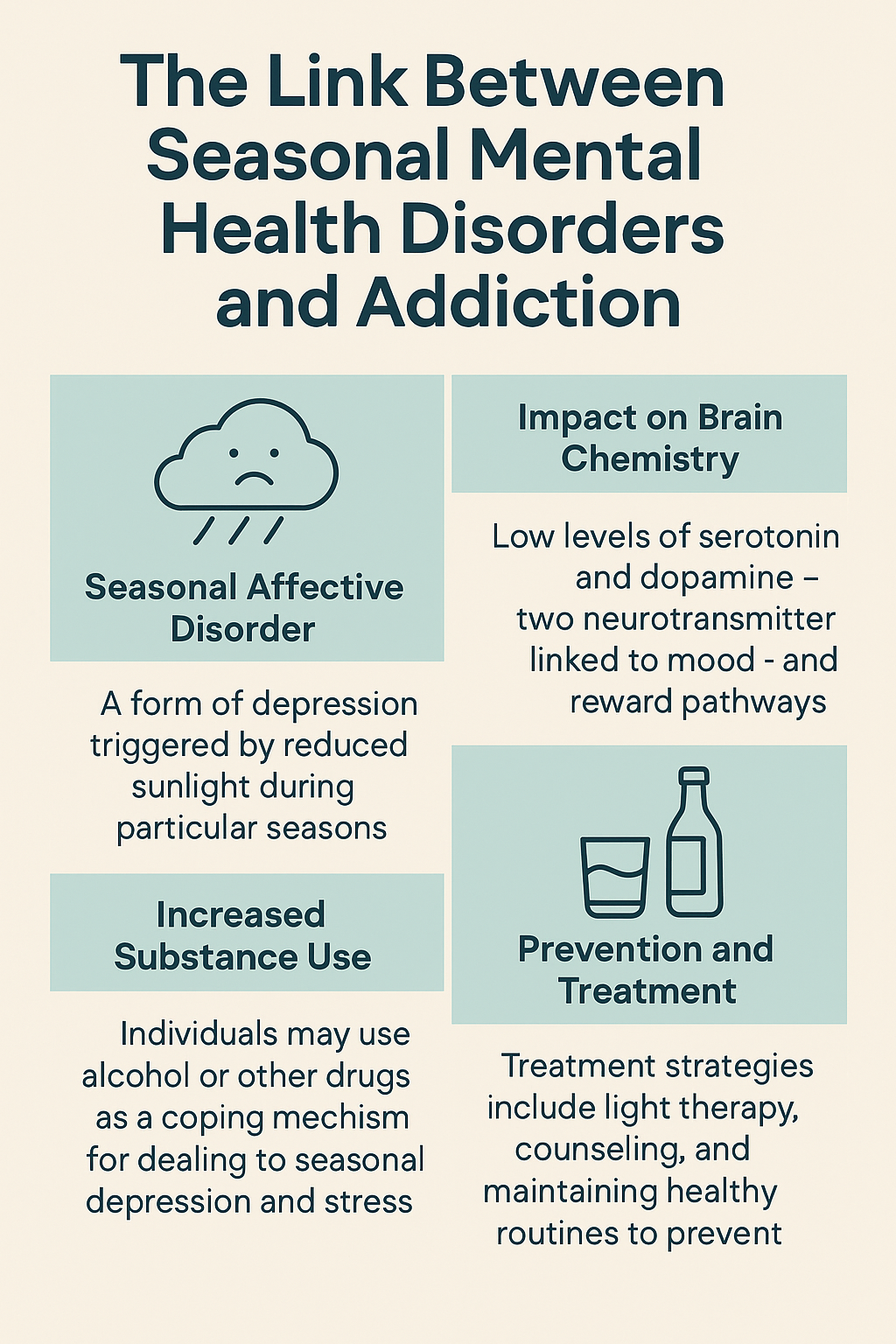
The Link Between Seasonal Mental Health Disorders and Addiction
Seasonal mental health issues, such as Seasonal Affective Disorder (SAD) or the “winter blues,” can have a significant impact on addiction in several ways. The changes in mood, energy levels, and overall mental health that occur during different seasons can influence a person’s relationship with substances, either by exacerbating existing addictive behaviors or triggering relapse. Here’s how seasonal mental health issues can affect addiction:
1. Increased Substance Use as a Coping Mechanism
Self-Medicating
- People with seasonal mental health issues, especially during the fall and winter months, may turn to alcohol, drugs, or other substances as a way to self-medicate and cope with feelings of depression, anxiety, or low energy. This self-medication can lead to or exacerbate addiction.
Escaping Emotional Pain
- Seasonal affective disorder, with its symptoms of sadness, irritability, and lack of motivation, might lead individuals to use substances to numb their emotional pain temporarily or to escape negative feelings. This can become a cycle of dependency, where the substance use amplifies the underlying mental health issue.
2. Increased Risk of Relapse
Darker Months and Isolation
- In the winter months, reduced daylight and colder weather can contribute to social isolation and withdrawal, which may increase the risk of relapse for individuals in recovery. If someone is already struggling with feelings of sadness or loneliness, they may turn to substances as a way to deal with these emotions.
Stress and Pressure of the Holidays
- The holiday season can bring up complex emotions, including stress, anxiety, and sadness, especially for individuals with a history of substance abuse. The pressure to attend social events or the emotional strain from family dynamics may lead someone to relapse if they haven’t fully developed healthy coping mechanisms.
3. Mood Fluctuations and Addiction Vulnerability
Impaired Judgment and Decision-Making
- Seasonal mood disorders can cause cognitive and emotional impairment, making it harder for individuals to resist the temptation to use substances. For example, those who feel depressed, anxious, or fatigued during the winter months may be less able to exercise self-control and may find it easier to give in to cravings.
Heightened Sensitivity to Triggers
- People with seasonal mood changes may be more sensitive to specific triggers that lead to substance use, such as social pressures or environmental factors (e.g., holidays, lack of sunlight, etc.). These triggers can be more complex to manage when mental health is compromised, increasing vulnerability to addiction.
4. Disruption of Recovery and Treatment Plans
Lack of Motivation and Energy
- Individuals struggling with seasonal mental health issues may experience a lack of motivation, which can affect their commitment to recovery. Treatment plans, support meetings, or self-care routines may be neglected during times of low energy or when symptoms of depression set in.
Difficulty Accessing Support
- Seasonal factors can also make it more challenging to access support, particularly in areas with harsh winters. In-person therapy sessions, support groups, or treatment programs may become harder to attend due to weather, leading to disruptions in treatment or recovery support systems.
5. Changes in Lifestyle and Coping Mechanisms
Disrupted Routines
- Seasonal changes often affect daily routines, which can interfere with healthy habits that support recovery. For example, changes in diet, sleep patterns, or exercise routines can lead to physical and mental instability, increasing susceptibility to addiction.
Lack of Outdoor Activities
- During the winter months, people may be less likely to engage in outdoor physical activities like walking or hiking, which are often used to improve mood and reduce stress. The absence of these activities can lead to a lack of healthy outlets for managing mental health and emotional regulation.
6. Increased Substance Use in Certain Seasons
Alcohol Use During Holidays
- In many cultures, alcohol consumption is a central part of holiday celebrations. This increase in social drinking during holidays like Christmas and New Year’s can be a trigger for those in recovery, especially if they have a history of alcohol dependence.
Increased Accessibility of Substances
- During the colder months, people may spend more time indoors in social settings where drugs or alcohol are more readily available. Increased availability and pressure to socialize can encourage substance use, particularly for those who are vulnerable to addiction.
7. Changes in Sleep Patterns
Sleep Disturbances
- Seasonal changes, particularly in winter when there is less sunlight, can disrupt sleep patterns and lead to issues like insomnia or oversleeping. Sleep deprivation or irregular sleep can worsen mental health symptoms, making it harder to manage addiction triggers and cravings.
Management Strategies
Light Therapy
- For those affected by SAD or winter blues, light therapy can help regulate mood and sleep patterns, potentially reducing the need to self-medicate with substances.
Cognitive Behavioral Therapy (CBT)
- CBT can help individuals address negative thought patterns associated with both seasonal depression and addiction, providing healthier coping mechanisms for managing emotions.
Exercise and Social Support
- Regular exercise, even in winter months, can boost mood and reduce cravings for substances. Additionally, maintaining strong social support networks can help individuals stay engaged in recovery and avoid isolation.
Mindfulness and Stress Management
- Practices like mindfulness, meditation, and yoga can help manage stress and mood fluctuations associated with seasonal changes, reducing the likelihood of turning to substances for relief.
In summary, seasonal mental health issues can have a profound effect on addiction, making individuals more vulnerable to substance use, relapse, and other complications. Recognizing the link between seasonal mood changes and addiction can help in developing strategies to address both issues, improving overall mental health, and promoting recovery.
Self-Management Strategies for Seasonal Mental Disorders
Managing seasonal mental health conditions to prevent addiction involves adopting self-management strategies that promote mental well-being and reduce the risk of using substances as a coping mechanism. Here are some self-management strategies that can help individuals with seasonal mental health issues avoid turning to addiction:
1. Light Therapy
- What it is: Light therapy involves exposure to bright light, usually through a specialized light box, to simulate natural sunlight. This is particularly effective for Seasonal Affective Disorder (SAD), which is triggered by reduced sunlight during the fall and winter months.
- How it helps: Regular light exposure can help regulate circadian rhythms, improve mood, and reduce symptoms of depression, making individuals less likely to resort to substances to alleviate negative feelings.
2. Regular Physical Activity
- What it is: Engaging in regular exercise, such as walking, jogging, or yoga, can boost mood and energy levels.
- How it helps: Physical activity increases the production of endorphins (natural mood boosters) and reduces stress and anxiety, which can lower the risk of using substances to cope with seasonal mental health challenges. Exercise can also help regulate sleep, which can be disrupted during seasonal changes.
3. Maintaining a Routine
- What it is: Establishing a consistent daily routine, including regular sleep, meal, and activity schedules.
- How it helps: A structured routine helps maintain stability and predictability, reducing feelings of unpredictability or emotional instability during the changing seasons. A routine can also reduce the temptation to engage in unhealthy coping mechanisms, such as substance use.
4. Mindfulness and Stress Management
- What it is: Mindfulness practices, including meditation, deep breathing, and yoga, help individuals stay grounded and focused on the present moment.
- How it helps: Mindfulness can reduce stress, anxiety, and depressive symptoms that may arise during certain seasons. By developing these practices, individuals can improve their emotional regulation, which lowers the likelihood of turning to substances as a form of escape.
5. Social Engagement and Support
- What it is: Staying connected with friends, family, or support groups during difficult times.
- How it helps: Social support is crucial for maintaining mental health and combating isolation, which can worsen seasonal mental health issues. Engaging in social activities or support groups, like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), can provide connection and accountability, reducing the urge to self-medicate with substances.
6. Healthy Nutrition
- What it is: Eating a balanced diet that includes plenty of whole foods, fruits, vegetables, and lean proteins.
- How it helps: A healthy diet can stabilize mood by providing essential nutrients and supporting overall physical health. Nutritional imbalances can exacerbate mental health issues, and poor eating habits may increase cravings for substances or comfort food. Ensuring that nutrient needs are met can prevent this cycle.
7. Sleep Hygiene
- What it is: Practicing good sleep habits, including maintaining a consistent sleep schedule, avoiding caffeine and electronics before bed, and creating a calm sleeping environment.
- How it helps: Proper sleep is critical for managing both mental health and addiction recovery. Lack of sleep can worsen mood disorders and make it harder to resist substance use. Maintaining sleep hygiene helps regulate sleep patterns and supports emotional stability.
8. Avoiding Triggers
- What it is: Identifying and avoiding situations, environments, or people that may trigger cravings or temptations to use substances.
- How it helps: During periods of seasonal mental health issues, individuals may be more vulnerable to addiction triggers. By recognizing potential triggers (e.g., stressful family gatherings, negative thought patterns), individuals can develop strategies to avoid or cope with them, reducing the risk of relapse or substance use.
9. Cognitive Behavioral Therapy (CBT) Techniques
- What it is: CBT is a form of therapy that helps individuals identify and change negative thought patterns and behaviors. Individuals can also apply some CBT techniques to their daily lives.
- How it helps: By addressing negative thoughts, such as those that may arise during seasonal mental health struggles, individuals can challenge and reframe these thoughts before they lead to substance use. This promotes healthier coping mechanisms and reduces the likelihood of using substances as a way to cope.
10. Setting Goals and Planning for Difficult Seasons
- What it is: Setting achievable, realistic goals and planning for seasons that may trigger mental health issues, such as winter or the holiday season.
- How it helps: Planning allows individuals to anticipate difficulties and put support systems in place, such as therapy, exercise routines, or additional social engagements. Having goals in place gives individuals something positive to focus on, which can help counteract feelings of hopelessness or despair.
11. Seeking Professional Help
- What it is: Reaching out to a therapist or mental health professional for support when seasonal mental health issues become overwhelming.
- How it helps: Therapy, primarily cognitive behavioral therapy or other therapeutic modalities, can help individuals address the underlying causes of their mental health struggles. Professionals can also offer strategies and tools to prevent substance use during difficult times.
12. Engaging in Hobbies and Activities
- What it is: Staying involved in hobbies and activities that bring joy and fulfillment, whether it’s reading, crafting, or spending time outdoors.
- How it helps: Engaging in enjoyable activities helps divert attention away from negative feelings or cravings for substances. Hobbies provide a positive outlet for energy and can improve mood, particularly when used as a distraction during challenging seasons.
In summary, by adopting self-management strategies such as light therapy, physical activity, mindfulness, and strong social support, individuals can better manage seasonal mental health issues and reduce the risk of addiction. These strategies help address both the psychological and physical factors that contribute to seasonal mood changes, providing healthier ways to cope and promoting overall well-being.
The Role of Family Support in Managing Seasonal Mental Disorders and Preventing Addiction
Family support plays a crucial role in managing seasonal mental health conditions and preventing the development or escalation of addiction. Strong family involvement can provide emotional stability, accountability, and resources for individuals experiencing seasonal mental health challenges. Here are some family support strategies that can help manage seasonal conditions and reduce the risk of addiction:
1. Open Communication
- What it is: Encouraging honest and open conversations about feelings, challenges, and mental health concerns.
- How it helps: Family members can create a safe space where individuals feel comfortable expressing their struggles. Open communication reduces isolation, one of the key factors that can contribute to both seasonal depression and substance use.
2. Encouraging Healthy Routines
- What it is: Supporting the individual in maintaining a consistent daily routine, including sleep, meals, and exercise.
- How it helps: Family members can help establish and stick to a healthy routine, which is essential for managing both seasonal mental health issues and preventing the temptation to turn to substances. This structure can provide stability during times of emotional vulnerability.
3. Participating in Physical Activities Together
- What it is: Engaging in physical activities as a family, such as walking, hiking, exercising, or even taking part in outdoor winter activities.
- How it helps: Regular physical activity is a proven way to combat symptoms of depression and anxiety, especially during the colder, darker months. Family involvement makes it more enjoyable and provides additional motivation to stay active, which can reduce the risk of using substances to cope.
4. Providing Emotional Support
- What it is: Offering unconditional emotional support and encouragement, especially during tough seasonal changes.
- How it helps: A family that provides emotional support allows individuals to feel valued and understood, reducing feelings of isolation or inadequacy. Emotional support can help manage negative thoughts or feelings that may arise during seasonal transitions, preventing self-medication with substances.
5. Recognizing Warning Signs
- What it is: Helping family members become aware of the signs of worsening mental health or potential substance misuse, such as withdrawal, changes in mood, irritability, or substance use triggers.
- How it helps: Being proactive in recognizing early signs of seasonal depression or addiction can allow for early intervention, such as seeking professional help or providing additional emotional support before things escalate.
6. Setting Healthy Boundaries
- What it is: Encouraging the establishment of boundaries with respect to substance use and unhealthy coping behaviors.
- How it helps: Family members can help individuals recognize and set boundaries around situations or behaviors that might trigger substance use, such as avoiding parties where alcohol or drugs are present. Clear, healthy boundaries are crucial for maintaining long-term recovery and managing seasonal mental health conditions.
7. Encouraging Treatment and Professional Help
- What it is: Supporting the individual in seeking professional help when needed, such as therapy, counseling, or psychiatric care.
- How it helps: Family members can play an essential role in encouraging therapy or medical treatment, especially if seasonal mental health issues become severe. Whether it’s seeking treatment for Seasonal Affective Disorder (SAD) or addiction counseling, family support can facilitate access to appropriate care.
8. Promoting Social Connection
- What it is: Encouraging involvement in social activities, both within the family and outside it, to reduce isolation.
- How it helps: Social connection is essential for mental health, particularly in the winter months when individuals may experience social withdrawal due to seasonal changes. By promoting positive social interactions, families can help reduce feelings of loneliness or depression that may lead to substance use.
9. Providing Structure During Holidays or Stressful Seasons
- What it is: Offering support during potentially stressful times, such as the holidays, when individuals may feel more isolated or overwhelmed.
- How it helps: Holidays can be tough for those experiencing seasonal depression or mental health struggles. Families can create a structured, supportive environment by planning activities, offering reassurance, and creating a calm atmosphere that helps reduce stress and prevents substance use as a coping mechanism.
10. Supporting Healthy Coping Mechanisms
- What it is: Teaching and encouraging healthier ways to cope with seasonal mood changes, such as mindfulness, journaling, or creative hobbies.
- How it helps: Family members can model and support the development of healthier coping mechanisms that help manage stress or depressive feelings. By offering alternative activities to substance use, families can help individuals navigate seasonal challenges without turning to addiction.
11. Celebrating Small Wins
- What it is: Acknowledging and celebrating small achievements, such as getting outside for a walk or successfully sticking to a routine.
- How it helps: Positive reinforcement from family members can help build confidence and improve self-esteem, especially when managing mental health struggles. Recognizing progress, no matter how small, boosts motivation and can prevent relapse into unhealthy behaviors like substance use.
12. Education on Seasonal Mental Health and Addiction
- What it is: Educating family members about the impact of seasonal mental health conditions and how they can contribute to addiction.
- How it helps: Education helps families better understand the mental health issues their loved ones are facing and how to offer more informed support. It can also help in identifying effective strategies to reduce the risk of substance use and better navigate seasonal challenges.
In summary, family support is essential in helping individuals manage seasonal mental health conditions and avoid the path to addiction. By providing emotional support, promoting healthy routines, recognizing warning signs, and encouraging professional help, families can play a proactive role in preventing substance use and fostering long-term mental well-being. By actively supporting one another during difficult seasons, families can reduce the risk of self-medication and improve overall recovery and mental health outcomes.
Community Resource Strategies for Managing Seasonal Mental Disorders
Community resources can play a vital role in managing seasonal mental health conditions and preventing the development or escalation of addiction. By leveraging local services, support networks, and wellness programs, individuals struggling with seasonal mood changes or mental health issues can receive the help they need to prevent self-medication with substances. Here are several community resource strategies that can help manage seasonal mental health conditions and reduce the risk of addiction:
1. Access to Mental Health Services What it is: Offering accessible and affordable mental health services, including therapy, counseling, and psychiatric care, especially during seasons when individuals are more likely to experience mood changes.
- How it helps: Communities can provide local mental health clinics, support groups, and hotlines that offer immediate support and long-term treatment for individuals struggling with Seasonal Affective Disorder (SAD) or other mental health conditions. These services provide an alternative to self-medicating with substances and ensure that individuals receive professional care.
2. Support Groups for Seasonal Affective Disorder (SAD) and Addiction Recovery What it is: Facilitating peer-led support groups that focus on both seasonal mental health struggles and addiction recovery, such as group therapy for depression or recovery-focused meetings (e.g., Alcoholics Anonymous, Narcotics Anonymous).
- How it helps: Support groups foster a sense of community, providing a safe space for individuals to share their experiences and coping strategies. The peer support fosters connection, reduces isolation, and encourages healthier ways to cope with mental health challenges, lowering the risk of substance abuse.
3. Workshops and Educational Programs What it is: Offering workshops or educational programs on managing seasonal mental health conditions, coping mechanisms, and addiction prevention.
- How it helps: Educating individuals on the signs of seasonal depression and addiction and providing strategies to manage them can empower people to seek help early. These programs may also offer stress management techniques, mindfulness practices, and information on healthy lifestyle habits that prevent substance abuse.
4. Accessible Light Therapy Centers What it is: Establishing community-based light therapy centers for individuals who experience Seasonal Affective Disorder (SAD), providing affordable access to light therapy.
- How it helps: Light therapy has been proven to be effective in treating SAD by mimicking natural sunlight. By offering this resource in the community, individuals can manage their seasonal mental health symptoms without resorting to substance use as a coping mechanism.
5. Exercise and Wellness Programs What it is: Providing community fitness programs, such as yoga classes, walking groups, or recreational sports leagues, designed to improve mental health and promote physical well-being.
- How it helps: Physical activity is a natural mood booster, reducing stress, anxiety, and depressive symptoms. Community wellness programs encourage individuals to stay active, which can help combat feelings of isolation and prevent substance use as a way to cope.
6. Crisis Hotlines and Emergency Mental Health Services What it is: Offering 24/7 crisis hotlines and emergency mental health services that individuals can reach out to in times of immediate need.
- How it helps: Crisis hotlines offer immediate emotional support and guidance during difficult seasons. For those experiencing overwhelming symptoms of depression or anxiety, these services can provide timely intervention and connect them with further treatment options, preventing substance abuse from escalating.
7. Community-Based Peer Mentoring What it is: Establishing peer mentoring programs where individuals with lived experience of managing seasonal mental health conditions or addiction recovery can offer guidance and support to others.
- How it helps: Peer mentors can provide valuable advice, encouragement, and motivation for individuals dealing with seasonal depression or the risk of addiction. Peer-led initiatives often make people feel less alone, increasing the likelihood of seeking help early and using healthier coping mechanisms.
8. Mobile Outreach and Telehealth Services What it is: Offering mobile outreach services and telehealth options for individuals who may have difficulty accessing in-person care, especially during the colder months or in rural areas.
- How it helps: Telehealth makes it easier for individuals to access mental health care from home, particularly when physical mobility or weather conditions prevent travel. Mobile outreach can bring services to those in need, ensuring that support is available even when in-person visits are not feasible.
9. Community Mental Health Awareness Campaigns What it is: Launching public awareness campaigns to educate the community about seasonal mental health conditions, such as SAD, and the link between mental health and addiction.
- How it helps: Awareness campaigns help reduce stigma around mental health and addiction, encouraging individuals to seek help sooner. These campaigns can also highlight available local resources, ensuring that people know where to turn for support during difficult seasons.
10. Social and Recreational Events What it is: Organizing community social events, such as holiday dinners, outdoor activities, or community gatherings, to reduce social isolation during difficult seasons.
- How it helps: Social connection is key to mental health. These events can foster a sense of belonging, alleviate feelings of loneliness, and provide opportunities for people to engage in healthy, substance-free social interactions. This can reduce the temptation to turn to substances during moments of emotional vulnerability.
11. Nutrition and Wellness Programs What it is: Providing community nutrition programs that focus on mental health, such as workshops on healthy eating or offering meals to low-income individuals.
- How it helps: Good nutrition is closely linked to mental health. Communities can offer programs that educate individuals on how to maintain a balanced diet during seasonal changes, which can help stabilize mood and reduce the urge to self-medicate with alcohol or drugs.
12. Access to Safe and Supportive Housing What it is: Providing supportive housing options for individuals struggling with seasonal mental health issues and addiction, particularly in times of crisis.
- How it helps: For individuals facing both mental health challenges and addiction, having a safe and supportive place to live can significantly reduce stress and provide a stable environment for recovery. Housing programs can also connect individuals with other essential services, including mental health treatment and substance abuse counseling.
In summary, community resources offer a multifaceted approach to managing seasonal mental health conditions and preventing addiction. By providing access to mental health services, support groups, educational programs, exercise opportunities, and emergency care, communities can help individuals navigate seasonal changes without resorting to substances. The availability of these resources fosters a supportive environment that encourages healthier coping mechanisms, reduces isolation, and ensures that individuals have the tools they need to manage both seasonal mood fluctuations and addiction risks.
Frequently Asked Questions
Here are some common questions:
Question: What are the signs of seasonal mental disorder?
Answer: Seasonal mental disorders, such as Seasonal Affective Disorder (SAD) and other mood fluctuations linked to seasonal changes, can manifest in various ways. The most common form, winter-pattern SAD, occurs in the fall and winter months due to reduced sunlight, while summer-pattern SAD is less common but can occur in warmer months. Here are the key signs:
Emotional Symptoms
- Persistent sadness or low mood – Feeling down or hopeless for extended periods.
- Irritability or agitation – Easily frustrated, anxious, or moody.
- Loss of interest – No longer enjoying hobbies, socializing, or usual activities.
- Increased stress or anxiety – Feeling overwhelmed without clear reasons.
- Feelings of worthlessness or guilt – Negative self-perception or excessive self-criticism.
Physical Symptoms
- Changes in sleep patterns – Sleeping too much (winter-pattern) or experiencing insomnia (summer-pattern).
- Low energy or fatigue – Feeling sluggish, lethargic, or physically drained.
- Changes in appetite – Craving carbohydrates and gaining weight (winter-pattern) or losing appetite and weight (summer-pattern).
- Difficulty concentrating – Struggling with focus, decision-making, or memory.
- Physical aches and pains – Unexplained headaches, muscle pain, or general discomfort.
Behavioral Symptoms
- Social withdrawal – Avoiding friends, family, or responsibilities.
- Decreased motivation – Difficulty completing tasks, even routine ones.
- Engaging in unhealthy coping mechanisms – Increased use of alcohol, drugs, or binge-eating to manage mood.
- Reduced productivity – Struggling to keep up with work, school, or daily responsibilities.
When to Seek Help
If symptoms last for more than two weeks and interfere with daily life, relationships, or work, it’s essential to seek professional help. Seasonal mental health issues can be managed with therapy, light therapy, lifestyle changes, and sometimes medication.
Question: Why is it essential to treat seasonal mental disorders?
Answer: Why Is It Important to Treat Seasonal Mental Disorders?
Seasonal mental disorders, such as Seasonal Affective Disorder (SAD) and other seasonal mood fluctuations, can have significant effects on an individual’s mental, emotional, and physical health. Without proper treatment, these conditions can worsen over time and lead to more serious complications. Here’s why it’s essential to address and manage seasonal mental disorders:
1. Prevents Symptoms from Worsening
- If left untreated, seasonal mental disorders can escalate, leading to more severe depression, anxiety, or mood instability.
- Over time, untreated SAD can increase the risk of developing major depressive disorder (MDD) or generalized anxiety disorder (GAD).
2. Reduces the Risk of Substance Abuse
- People experiencing seasonal mood changes may turn to alcohol, drugs, or overeating as a way to cope.
- Treating SAD can reduce reliance on unhealthy coping mechanisms, preventing addiction or substance dependence.
3. Improves Daily Functioning
- SAD can interfere with work, school, and relationships, making it difficult to concentrate, stay motivated, or complete tasks.
- Treatment helps restore energy levels, focus, and productivity, improving quality of life.
4. Supports Emotional and Social Well-Being
- Many people with seasonal disorders withdraw from friends and family, leading to loneliness and isolation.
- Proper treatment encourages social engagement and emotional stability, strengthening relationships and support systems.
5. Enhances Physical Health
- Seasonal depression is linked to poor sleep, weight gain, and weakened immune function.
- Addressing it can lead to better sleep patterns, healthier eating habits, and improved overall wellness.
6. Prevents Long-Term Mental Health Complications
- If untreated, seasonal mental health issues can lead to chronic depression, anxiety disorders, or suicidal thoughts.
- Early intervention can prevent long-term psychological distress and reduce the risk of hospitalization.
7. Encourages the Development of Healthy Coping Mechanisms
- Treating seasonal mental disorders helps individuals develop positive coping strategies, such as:
- Light therapy
- Regular exercise
- Mindfulness and stress management
- Healthy sleep and nutrition habits
8. Increases Overall Life Satisfaction
- Seasonal disorders can take away motivation, enjoyment, and engagement in life.
- Effective treatment helps restore emotional balance, allowing individuals to feel happier, more fulfilled, and in control.
Final Thoughts
Ignoring seasonal mental health issues can have serious emotional, psychological, and physical consequences. By seeking therapy, lifestyle changes, light therapy, or medication if needed, individuals can manage their symptoms and prevent long-term complications.
Question: How effective are the treatments for seasonal mental disorders?
Answer: Effectiveness of Treatments for Seasonal Mental Disorder
The treatments for Seasonal Affective Disorder (SAD) and other seasonal mental health conditions are generally effective, especially when tailored to the individual’s symptoms and needs. The best results often come from a combination of therapies. Here’s an overview of the most common treatments and their effectiveness:
1. Light Therapy (Phototherapy)
- Effectiveness: ⭐⭐⭐⭐⭐ (Highly Effective)
- How It Works: Light therapy involves using a lightbox that mimics natural sunlight to help regulate mood and energy levels.
- Research Findings: Studies show that light therapy improves symptoms in 60–80% of people with SAD, often within 1–2 weeks.
- Best For: People with winter-pattern SAD, as it helps reset the body’s circadian rhythm and boost serotonin levels.
2. Cognitive Behavioral Therapy (CBT)
- Effectiveness: ⭐⭐⭐⭐⭐ (Highly Effective)
- How It Works: CBT helps individuals recognize and change negative thought patterns and behaviors that contribute to seasonal depression.
- Research Findings: Studies suggest CBT is as effective as light therapy for SAD, with longer-lasting benefits.
- Best For: Those seeking a long-term, non-medication approach to managing seasonal mental health challenges.
3. Antidepressant Medications (SSRIs & Bupropion)
- Effectiveness: ⭐⭐⭐⭐☆ (Very Effective)
- How It Works: Selective serotonin reuptake inhibitors (SSRIs) like fluoxetine (Prozac) or sertraline (Zoloft) help regulate mood. Bupropion (Wellbutrin) is also approved for the prevention of SAD.
- Research Findings: Antidepressants are effective for many individuals, but they may take 4–6 weeks to show full benefits.
- Best For: People with moderate to severe seasonal depression, primarily if other treatments don’t provide enough relief.
4. Vitamin D Supplementation
- Effectiveness: ⭐⭐⭐☆☆ (Moderately Effective)
- How It Works: Many individuals with SAD have low Vitamin D levels, and supplementation may help boost mood.
- Research Findings: Some studies show that Vitamin D helps improve symptoms, while others find only minor benefits.
- Best For: People with Vitamin D deficiency or mild SAD.
5. Lifestyle Changes (Exercise, Diet, Social Engagement)
- Effectiveness: ⭐⭐⭐⭐☆ (Very Effective)
- How It Works: Regular exercise, a healthy diet, and maintaining social connections can significantly boost mood and reduce SAD symptoms.
- Research Findings: Exercise, particularly outdoor activities, can be as effective as medication for mild to moderate depression.
- Best For: Anyone experiencing mild-to-moderate SAD, especially those who prefer a natural approach.
6. Mindfulness, Meditation, and Stress Management
- Effectiveness: ⭐⭐⭐☆☆ (Moderately Effective)
- How It Works: Practices such as mindfulness meditation, journaling, and breathing exercises help manage stress and improve mood.
- Research Findings: Mindfulness-based interventions reduce symptoms of depression and improve emotional resilience.
- Best For: People looking for a holistic approach or an adjunct to other treatments.
Which Treatment is Best?
The most effective approach depends on the severity of symptoms:
✅ Mild SAD: Lifestyle changes, Vitamin D, light therapy
✅ Moderate SAD: Light therapy + CBT
✅ Severe SAD: Light therapy + CBT + Antidepressants
Final Verdict
Most people experience relief from seasonal depression with proper treatment. A combination of light therapy, therapy, lifestyle changes, and sometimes medication can significantly improve mood and prevent seasonal depression from worsening.
Conclusion
Seasonal mental health conditions can significantly contribute to the development or worsening of addiction, but effective management through self-care, family support, and community resources can help mitigate this risk. Self-management strategies, such as maintaining healthy routines and seeking professional support, are key to coping with seasonal mood changes. Family involvement provides crucial emotional stability and encouragement, while community resources offer access to mental health services and support groups. By combining these strategies, individuals can better manage seasonal mental health challenges, reduce their reliance on substances, and maintain overall well-being during difficult times.
Video: Are Seasonal Changes Secretly Fueling Your Addiction Habits?