Cocaine-related deaths have increased at an alarming rate in recent years, creating a growing public health crisis. A major factor driving this rise is the unpredictable drug supply, particularly cocaine contaminated with synthetic opioids such as fentanyl. This contamination has led to unexpected overdoses, even among individuals who do not regularly use opioids. While medical and public health systems work to address this emergency, preventing cocaine-related deaths also requires action at the personal, family, and community levels. Self-management strategies help individuals reduce risky behaviors; family support provides emotional safety; and community resources offer harm-reduction tools and treatment access. Together, these layers of support form a powerful defense against fatal outcomes.
Rising Cocaine-Related Deaths: Understanding a Growing Public Health Crisis
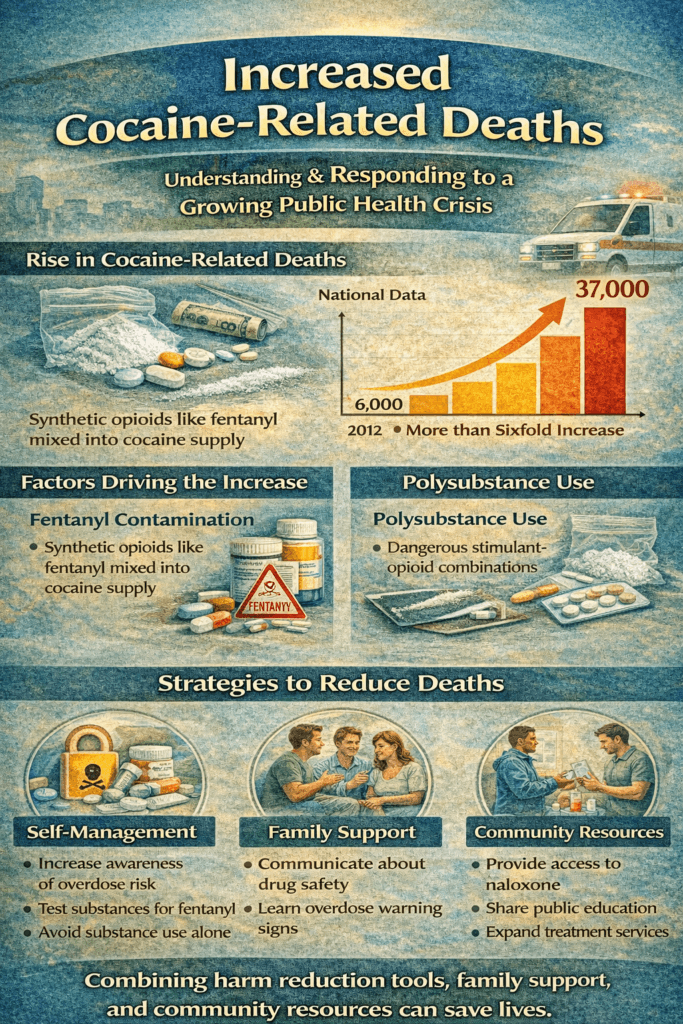
In recent years, cocaine-related deaths have surged, contributing to a growing public health crisis in the United States and beyond. Though overall drug overdose rates have shown some variability, deaths involving cocaine continue to rise, underscoring complex changes in drug markets and patterns of substance use. According to national mortality data, the number of overdose deaths involving cocaine increased sharply over the past decade, with tens of thousands of deaths recorded in recent years — a more than six-fold rise from previous counts.
Several key factors help explain this alarming trend. One is polysubstance use, particularly the mixing of cocaine with potent opioids such as fentanyl. Illicit drug supplies are increasingly contaminated, meaning individuals may unknowingly consume stimulant-opioid combinations, significantly increasing the risk of fatal overdose. Nearly 80% of cocaine poisonings now involve one or more opioids, according to recent state-level data. This dangerous combination overwhelms the body’s respiratory and cardiovascular systems, making overdose more likely even in people who have previously tolerated cocaine without fatal outcomes.
Changes in cocaine purity and availability also play a role. High-purity cocaine is widely available and often cheaper, which can lead to higher doses and increased risk of toxicity. Additionally, patterns of use have shifted geographically and demographically, with increases reported among older adults and various racial and ethnic groups, even as overall overdose rates fluctuate.
Public health responses to rising cocaine-related fatalities must address these multifaceted trends. Harm-reduction strategies — such as providing education about the risks of polysubstance use, expanding access to naloxone (a life-saving opioid antagonist), and offering drug-checking services to detect fentanyl contamination — are critical. Early intervention, linkage to treatment services (including behavioral therapies and support for stimulant use disorders), and community-level prevention efforts also play essential roles in reducing deaths. As the landscape of substance use evolves, comprehensive strategies that acknowledge the complexity of cocaine and polysubstance harms are more important than ever.
Self-Management Strategies to Reduce Cocaine-Related Deaths
Cocaine-related deaths have risen sharply in recent years, becoming a growing public health concern. One of the most dangerous factors driving this increase is the contamination of cocaine with synthetic opioids such as fentanyl. Many individuals are unaware that the substance they are using contains potent additives, dramatically raising the risk of fatal overdose. While community and medical interventions are essential, self-management strategies can also play a critical role in reducing harm and preventing death.
The first self-management strategy is increasing personal awareness of risk. Understanding that today’s illicit drug supply is unpredictable helps individuals make safer decisions. Recognizing early warning signs of overdose — such as sudden breathing difficulty, loss of consciousness, or extreme drowsiness — allows for faster emergency response and life-saving action.
Seeking drug-checking services is another important harm-reduction approach. Many communities now offer testing programs that detect fentanyl contamination. Knowing whether a substance contains unexpected additives can prevent accidental exposure to lethal doses.
Never using substances alone is also a key protective behavior. Having another person nearby who can recognize distress and call for emergency help greatly increases the chances of survival. Carrying naloxone, a medication that reverses opioid overdose, provides additional safety in environments where contamination risk exists.
Managing patterns of use is another self-protective strategy. Avoiding binge use, spacing time between use, and being mindful of mixing substances reduces strain on the heart and nervous system. Self-monitoring emotional triggers such as stress, loneliness, or trauma can also help individuals recognize when they are at higher risk for dangerous use.
Finally, engaging in treatment and support services strengthens long-term protection. Behavioral therapies, stimulant-use disorder programs, peer recovery groups, and mental health counseling help individuals reduce dependence and move toward stability. Reaching out to healthcare providers for screening and treatment planning creates a pathway toward safer, healthier living.
Cocaine-related deaths are preventable. When individuals practice self-awareness, use available harm-reduction tools, seek support, and engage in treatment services, the risk of fatal outcomes decreases. Combining personal self-management with family, community, and medical support offers the strongest defense against this growing crisis.
Family Support Strategies to Reduce Cocaine-Related Deaths
Cocaine-related deaths have increased dramatically in recent years, driven largely by unpredictable drug supply contamination and polysubstance use, especially with fentanyl. This rise has affected families across all communities, often catching loved ones off guard. While public health and medical responses are critical, family support remains one of the most powerful protective factors in reducing the risk of fatal cocaine-related outcomes.
One essential family strategy is education. When family members understand current drug-market risks — including fentanyl contamination and overdose warning signs — they are better prepared to respond quickly in emergencies. Knowing symptoms such as slowed or stopped breathing, loss of consciousness, or blue lips can mean the difference between life and death. Families who learn how and when to call emergency services become active safety partners.
Open and non-judgmental communication is another key strategy. Individuals using cocaine are more likely to disclose struggles or risky behavior when they feel emotionally safe rather than shamed. Calm listening, empathy, and honest conversations about safety create opportunities for intervention before a crisis occurs.
Families can also encourage harm-reduction practices. Supporting access to naloxone, encouraging drug-checking services when available, and discouraging substance use alone increases survival chances if an overdose occurs. These conversations may feel uncomfortable, but they save lives.
Creating a stable home environment further reduces risk. Reducing exposure to high-risk social circles, encouraging healthy daily routines, and offering emotional support during stress or trauma lowers the likelihood of dangerous binge use.
Finally, families play a vital role in connecting loved ones to treatment. Supporting counseling, stimulant-use disorder programs, mental health care, and peer recovery groups helps individuals reduce dependence and build long-term stability. Families who participate in therapy or support groups themselves also strengthen their ability to help without enabling.
Cocaine-related deaths are preventable. When families stay informed, communicate openly, encourage safety measures, and support treatment engagement, they become a powerful shield against fatal outcomes. With education, compassion, and preparedness, families help turn crisis into connection and protection.
Community Resource Strategies to Reduce Cocaine-Related Deaths
Cocaine-related deaths have risen sharply in recent years, becoming an urgent public health concern. A major driver of this increase is the contamination of cocaine with potent synthetic opioids such as fentanyl, leading to unexpected and often fatal overdoses. Because these risks extend beyond individual behavior, community-level strategies are crucial for preventing deaths and strengthening public safety.
One of the most effective community strategies is expanding access to harm-reduction services. Drug-checking programs that test for fentanyl contamination help individuals understand the risks before use. Community distribution of naloxone — a medication that reverses opioid overdoses — ensures bystanders can act quickly during emergencies. Training residents, families, and public service workers to recognize overdose signs further increases survival rates.
Community health centers and outreach programs also play an essential role. Mobile clinics, street-outreach teams, and public health initiatives connect high-risk individuals to medical care, mental health services, and substance-use treatment. Early screening and referral to stimulant-use disorder programs help reduce dependence before a crisis occurs.
Public education campaigns strengthen prevention efforts. When communities openly share information about polysubstance risks, fentanyl contamination, and emergency response steps, stigma decreases and help-seeking increases. Awareness programs in schools, workplaces, and local organizations create a culture of preparedness rather than silence.
Practical support services are equally important. Housing assistance, employment programs, transportation services, and crisis hotlines reduce instability that often drives high-risk substance use. When individuals have access to basic needs and support systems, risky patterns of drug use decline.
Finally, collaboration between healthcare systems, law enforcement, social services, and recovery organizations creates coordinated safety networks. Communities that work together provide faster response, stronger prevention infrastructure, and more accessible treatment pathways.
Cocaine-related deaths are preventable when communities take action. By offering harm-reduction tools, education, outreach, treatment access, and social support, communities become a protective force that saves lives and builds healthier futures.
Frequently Asked Questions
Here are some common questions:
What does “cocaine-related death” mean?
A cocaine-related death refers to a fatal overdose or medical complication caused by cocaine use, either alone or in combination with other substances.
Why have cocaine-related deaths increased in recent years?
The primary reason is fentanyl contamination in the cocaine supply. Many individuals unknowingly consume cocaine mixed with powerful synthetic opioids, greatly increasing overdose risk.
Is cocaine itself dangerous enough to cause death?
Yes. Cocaine can cause a heart attack, stroke, seizures, and respiratory failure. Risk increases further when combined with other substances.
What role does fentanyl play in cocaine-related deaths?
Fentanyl is an extremely potent opioid. When mixed into cocaine, even tiny amounts can cause sudden and fatal breathing suppression.
Are most cocaine overdoses now linked to opioids?
Yes. Current data shows the majority of cocaine-related overdose deaths involve opioids, particularly fentanyl.
Can someone who does not use opioids still overdose on fentanyl-contaminated cocaine?
Yes. Individuals with no opioid tolerance are at especially high risk if exposed to fentanyl-laced cocaine.
What are the warning signs of a cocaine-related overdose?
Signs may include chest pain, irregular heartbeat, seizure, loss of consciousness, slow or stopped breathing, or blue lips and fingertips.
How can individuals reduce the risk of fatal overdose?
Using harm-reduction tools such as fentanyl test strips, carrying naloxone, avoiding use alone, and seeking treatment services can reduce risk.
How can families help prevent cocaine-related deaths?
Families can learn overdose warning signs, keep naloxone available, encourage open communication, and support access to treatment and counseling.
What community resources help reduce cocaine-related deaths?
Community programs provide naloxone distribution, drug-checking services, harm-reduction education, crisis hotlines, and addiction treatment access.
Is treatment available for cocaine use disorder?
Yes. Behavioral therapies, support groups, and mental health treatment programs help individuals reduce or stop cocaine use.
Are cocaine-related deaths preventable?
Yes. With education, harm-reduction strategies, family support, community resources, and treatment engagement, many cocaine-related deaths can be prevented.
Conclusion
Cocaine-related deaths are increasing, but they are not inevitable. When individuals practice self-awareness and harm-reduction behaviors, families communicate openly and provide informed support, and communities deliver accessible education, testing services, naloxone distribution, and treatment programs, lives can be saved. Addressing this crisis requires compassion, preparedness, and coordinated effort rather than blame or stigma. By combining self-management, family involvement, and community resource strategies, the risk of fatal cocaine-related overdose can be significantly reduced, offering hope, protection, and healthier futures for individuals and communities alike.
Video: