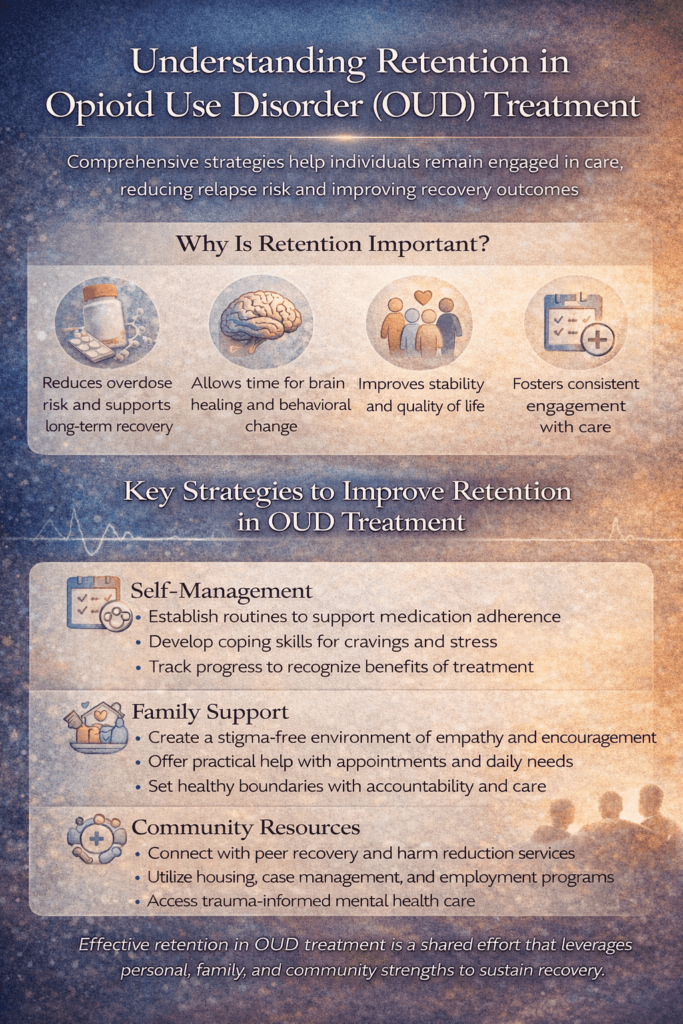
Retention in opioid use disorder (OUD) treatment is one of the most critical factors influencing survival, stability, and long-term recovery. Remaining engaged in care—particularly in medication for opioid use disorder (MOUD)—significantly reduces overdose risk and supports brain and behavioral recovery over time. However, retention is often threatened by cravings, stigma, logistical barriers, co-occurring mental health conditions, and social instability. Improving retention requires more than clinical intervention alone; it depends on a coordinated approach that empowers individuals through self-management skills, strengthens family support systems, and leverages community resources to reduce barriers and sustain engagement in care.
Retention in Opioid Use Disorder (OUD) Treatment: A Cornerstone of Recovery
Retention in opioid use disorder (OUD) treatment is one of the strongest predictors of reduced overdose risk, improved health outcomes, and long-term recovery. Retention refers to a patient’s ability to remain engaged in treatment over time, particularly in medication-based care such as methadone, buprenorphine, or extended-release naltrexone. While treatment initiation is critical, staying in care is what saves lives.
OUD is a chronic, relapsing condition that affects brain reward, stress, and decision-making systems. Early treatment dropout is common and often occurs during periods of instability, withdrawal discomfort, social stress, or stigma. When individuals disengage from care, the risk of relapse and overdose increases sharply, especially after periods of reduced tolerance. For this reason, retention is not merely an administrative metric—it is a clinical priority.
Medication for opioid use disorder (MOUD) plays a central role in improving retention. MOUD reduces cravings, stabilizes brain chemistry, and allows individuals to function without the constant cycle of withdrawal and intoxication. However, medication alone is not enough. Retention improves when care is accessible, flexible, and responsive to patients’ real-world needs.
Barriers to retention often include rigid program rules, transportation difficulties, work or childcare conflicts, insurance disruptions, stigma, untreated mental health conditions, and fear of judgment after relapse. When treatment models are punitive or inflexible, patients are more likely to disengage. In contrast, low-barrier, patient-centered approaches increase trust and continuity of care.
Supportive services significantly enhance retention. Counseling, peer recovery support, case management, housing assistance, and integrated mental health care help address the social and psychological factors that interfere with ongoing engagement. Trauma-informed care is especially important, as many individuals with OUD have histories of trauma that make traditional healthcare environments feel unsafe or alienating.
Retention also improves when treatment emphasizes dignity and collaboration. When patients are treated as partners in their care—rather than as noncompliant or high-risk—they are more likely to remain engaged even through setbacks. Relapse should be viewed as a clinical signal for adjustment, not a reason for discharge.
Ultimately, retention in OUD treatment saves lives. Sustained engagement allows time for brain recovery, behavioral change, and rebuilding of stability, relationships, and purpose. By prioritizing flexible, compassionate, and long-term care models, healthcare systems can transform OUD treatment from short-term interventions into sustained recovery support—where patients are not merely admitted but truly retained in care.
Self-Management Strategies to Improve Retention in Opioid Use Disorder (OUD) Treatment
Retention in opioid use disorder (OUD) treatment depends not only on program design and clinical care, but also on an individual’s ability to manage daily challenges that threaten engagement. Self-management strategies empower patients to remain active participants in their care, reduce the risk of dropout, and sustain recovery over time. When individuals develop skills that support consistency, emotional regulation, and motivation, staying in treatment becomes more achievable—even during difficult periods.
One key self-management strategy is routine building. OUD treatment often works best when medication dosing, appointments, sleep, and meals are consistent. Establishing daily routines helps stabilize the nervous system, reduce stress, and minimize missed doses or appointments. Simple tools such as reminders, alarms, calendars, and medication organizers support follow-through and continuity of care.
Craving and stress management are also essential. Cravings, emotional distress, or environmental triggers can undermine motivation to attend appointments or continue medication. Self-management techniques such as urge surfing, paced breathing, grounding exercises, and brief mindfulness practices help individuals tolerate discomfort without disengaging from care. Having a written plan for high-risk moments increases confidence and preparedness.
Self-advocacy strengthens retention by helping individuals communicate their needs within the treatment system. Patients who feel empowered to ask questions, report side effects, request dose adjustments, or discuss barriers such as transportation or work schedules are more likely to remain engaged. Understanding treatment options and participating in shared decision-making increases trust and commitment.
Tracking progress is another important strategy. Retention improves when individuals recognize benefits beyond abstinence, such as better sleep, reduced cravings, stronger relationships, or greater stability. Journaling or using recovery apps to document improvements reinforces motivation and reframes treatment as meaningful rather than burdensome.
Connection and accountability further support self-management. Peer support groups, recovery check-ins, or trusted support persons help normalize struggles and encourage persistence. Knowing that someone will notice disengagement or celebrate consistency reinforces commitment to care.
Finally, aligning treatment with personal values helps sustain engagement. When individuals connect OUD treatment to what matters most—health, family, freedom, stability, or self-respect—attendance and adherence become purposeful choices rather than obligations. Values-based motivation supports retention even during periods of low energy or doubt.
Self-management strategies do not replace clinical support, but they are critical complements to it. By building routines, coping skills, self-advocacy, and a sense of purpose, individuals strengthen their ability to remain engaged in OUD treatment. Improved retention not only supports recovery—it protects lives by keeping people connected to care when it matters most.
Family Support Strategies to Improve Retention in Opioid Use Disorder (OUD) Treatment
Retention in opioid use disorder (OUD) treatment is one of the strongest predictors of survival and long-term recovery. While clinical care and medication are essential, family support often determines whether individuals remain engaged in treatment during periods of stress, doubt, or instability. Families who understand OUD as a chronic medical condition—and who respond with structure, empathy, and consistency—can significantly improve treatment retention.
One of the most effective family strategies is fostering a nonjudgmental environment. Shame, blame, and criticism increase dropout risk by reinforcing stigma and avoidance of care. Families who communicate concern rather than disappointment help individuals feel safe staying engaged, even after setbacks. Language that emphasizes health, effort, and progress encourages continued participation rather than withdrawal.
Practical support also improves retention. Assistance with transportation, appointment reminders, childcare, or schedule coordination reduces common barriers to attending treatment. These supports do not remove responsibility from the individual but help stabilize daily logistics that often interfere with consistent care.
Education is another critical family strategy. Understanding how medications for opioid use disorder (MOUD) work—and why long-term treatment is often necessary—helps families move away from pressure to “taper quickly” or stop medication prematurely. When families view MOUD as a legitimate, life-saving treatment, they are more likely to encourage continued engagement.
Healthy boundaries are equally important. Supportive families set clear expectations around safety, communication, and responsibilities without threatening treatment access or withdrawing emotional support. Consistent boundaries reduce chaos while preserving dignity and accountability, making treatment feel sustainable rather than conditional.
Emotional encouragement strengthens motivation to remain in care. Acknowledging effort, celebrating consistency, and recognizing non-obvious progress—such as improved mood, stability, or honesty—reinforces the value of staying in treatment. Feeling valued for engagement rather than perfection promotes long-term retention.
Finally, families must attend to their own well-being. Burnout, fear, and unresolved trauma can unintentionally undermine support efforts. Family therapy, education groups, and peer support for loved ones help families remain grounded and effective partners in the recovery process.
When families combine empathy, education, boundaries, and practical support, they become powerful allies in retaining OUD treatment. Their involvement helps transform treatment from an individual struggle into a shared commitment—one that keeps people connected to care and alive long enough for recovery to take hold.
Community Resource Strategies to Improve Retention in Opioid Use Disorder (OUD) Treatment
Retention in opioid use disorder (OUD) treatment is strongly influenced by what happens outside the clinic walls. Community resources provide continuity, accessibility, and practical support that help individuals remain engaged in care over time. When treatment is reinforced by community-based services, patients are less likely to disengage during periods of instability, stress, or transition.
Peer recovery support is one of the most effective community strategies for improving retention. Peer specialists—individuals with lived experience of recovery—offer trust, relatability, and real-world guidance that complements clinical care. Regular peer contact reduces isolation, normalizes challenges with medication adherence or appointments, and encourages re-engagement after missed visits rather than dropout.
Recovery community centers also play a critical role. These centers offer low-barrier, nonjudgmental spaces where individuals can access support groups, education, employment readiness, wellness activities, and social connection without the pressure of clinical performance. By creating a sense of belonging and routine, recovery centers help individuals stay connected to recovery even when motivation fluctuates.
Harm reduction services further improve retention by prioritizing safety and dignity. Syringe service programs, naloxone distribution, overdose education, and infectious disease screening reduce health risks and keep individuals engaged with supportive systems. These services often serve as entry points—or re-entry points—into OUD treatment for individuals who might otherwise disengage due to fear or stigma.
Case management and social service linkages are equally important. Community-based programs that assist with housing, transportation, insurance navigation, employment, and legal issues help reduce the external stressors that commonly disrupt treatment attendance. Addressing social determinants of health increases stability and facilitates ongoing engagement in OUD treatment.
Integrated community mental health services also enhance retention. Many individuals with OUD have co-occurring depression, anxiety, PTSD, or other conditions that interfere with consistent care. Accessible, trauma-informed mental health support improves emotional regulation and reduces treatment dropout.
Finally, stigma reduction and community education initiatives create environments that support retention. Communities that recognize OUD as a chronic medical condition—rather than a moral failure—make it easier for individuals to stay in treatment without fear of judgment, discrimination, or exclusion.
Community resource strategies do not replace clinical OUD treatment; they strengthen it. By offering sustained connection, practical assistance, and compassionate engagement, communities help individuals stay engaged with care long enough for treatment to work. Improved retention is not just a clinical outcome—it is a community responsibility that saves lives.
Frequently Asked Questions
Here are some common questions:
What does retention in OUD treatment mean?
Retention refers to a person’s ability to remain consistently engaged in opioid use disorder treatment over time, particularly in medication for opioid use disorder (MOUD) such as methadone, buprenorphine, or extended-release naltrexone. It includes attending appointments, taking medication as prescribed, and maintaining contact with the care team.
Why is retention so important in OUD treatment?
Retention is one of the strongest predictors of survival and recovery. Staying in treatment significantly reduces overdose risk, supports brain stabilization, improves physical and mental health, and increases the likelihood of long-term recovery.
What happens when someone leaves OUD treatment too early?
Early dropout increases the risk of relapse and overdose, especially because opioid tolerance decreases quickly after stopping treatment. Even brief gaps in care can be dangerous; therefore, continuous engagement is critical.
What are common barriers to staying in OUD treatment?
Barriers include cravings, stigma, rigid program rules, transportation challenges, work or childcare conflicts, insurance disruptions, untreated mental health conditions, fear of judgment after relapse, and lack of social support.
Does relapse mean treatment has failed?
No. Relapse is a common feature of chronic conditions and should be viewed as a signal to adjust care, not as a reason to discontinue treatment. Programs that allow re-engagement after relapse improve retention and outcomes.
How does medication improve retention?
MOUD reduces cravings and withdrawal symptoms, stabilizes brain chemistry, and allows individuals to function without the constant cycle of intoxication and withdrawal. This stabilization facilitates attendance at appointments and engagement in care.
What can individuals do to improve their own retention?
Self-management strategies include building daily routines, using reminders for medication and appointments, learning coping skills for cravings and stress, tracking progress, and communicating openly with providers about challenges or side effects.
How can families help improve retention?
Families can support retention by reducing stigma, encouraging ongoing treatment, helping with logistics such as transportation or childcare, setting healthy boundaries, and focusing on effort and engagement rather than perfection.
What role do community resources play in retention?
Community resources provide support beyond the clinic. Peer recovery support, recovery community centers, harm reduction services, housing assistance, case management, and mental health services help address barriers that commonly lead to treatment dropout.
Are long-term treatment and retention really necessary?
Yes. OUD is a chronic condition, and many individuals benefit from long-term or even lifelong treatment. Longer retention is consistently associated with better outcomes, reduced risk of overdose, and improved quality of life.
How can treatment programs improve retention rates?
Programs can improve retention by offering low-barrier access, flexible scheduling, nonpunitive policies, trauma-informed care, integrated mental health services, peer support, and a culture that treats patients with dignity and respect.
What is the main takeaway about retention in OUD treatment?
Retention saves lives. Keeping people engaged in care—through supportive self-management, family involvement, and community resources—helps treatment work and lays the foundation for lasting recovery.
Conclusion
Improving retention in OUD treatment is most effective when self-management, family support, and community resource strategies work together to reinforce continuity of care. Self-management skills help individuals build routines, manage cravings, and remain motivated during difficult periods. Family support provides emotional stability, practical assistance, and encouragement that reduce the risk of dropout, while healthy boundaries preserve accountability and dignity. Community resources extend support beyond the clinic by addressing social determinants of health, offering peer connection, and creating recovery-friendly environments. When these strategies are integrated, retention becomes a shared responsibility rather than an individual burden—keeping people connected to treatment long enough for recovery to take root and lives to be saved.
Video: OUD treatment retention literally saves lives #AddictionRecovery #OverdosePrevention #MOUD