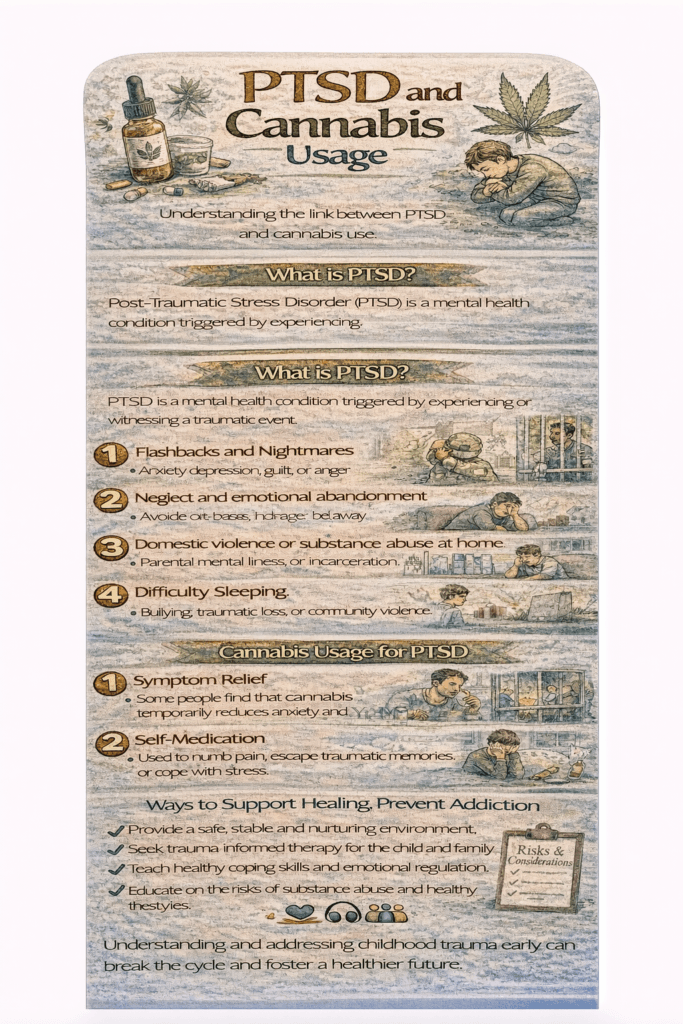
Post-Traumatic Stress Disorder (PTSD) poses challenges in treatment due to the variable effectiveness and potential side effects of current regimens, which typically involve psychotherapy and medication. In recent times, cannabis has emerged as an alternative for managing PTSD symptoms, though limited scientific evidence, regulatory concerns, and the presence of established treatments hinder its acceptance. The science of cannabis in PTSD treatment is actively researched, exploring the therapeutic potential of cannabinoids. Despite anecdotal reports, cautious adoption prevails, emphasizing the need for further research and a nuanced understanding of the complexities surrounding PTSD treatment.
Understanding PTSD: Causes, Symptoms, and Treatment Options
Post-Traumatic Stress Disorder (PTSD) is a serious mental health condition that arises after experiencing or witnessing a traumatic event. While trauma affects everyone differently, PTSD is characterized by a specific set of symptoms that persist and disrupt daily life.
Causes of PTSD
PTSD can develop after exposure to various types of trauma, including:
- Combat Exposure: Military personnel often face intense combat situations that can lead to PTSD.
- Physical Assault: Survivors of violent assaults may experience lasting psychological impacts.
- Accidents: Severe car crashes or other life-threatening accidents can trigger PTSD.
- Natural Disasters: Surviving events like earthquakes, floods, or hurricanes can leave lasting scars.
- Sexual Assault: Survivors of rape or sexual assault frequently face profound emotional and psychological challenges.
- Childhood Trauma: Individuals who experienced abuse, neglect, or other adverse childhood experiences are at increased risk for PTSD.
Symptoms of PTSD
PTSD symptoms generally fall into four main categories:
- Intrusive Thoughts
- Recurring, distressing memories or flashbacks of the traumatic event.
- Nightmares related to the trauma.
- Intense emotional or physical distress when reminded of the event.
- Avoidance
- Efforts to avoid people, places, or situations associated with the trauma.
- Avoiding conversations or thoughts about the traumatic event.
- Negative Changes in Thinking and Mood
- Persistent negative thoughts about oneself or the world.
- Distorted beliefs about responsibility for the trauma.
- Feelings of detachment or isolation.
- Difficulty experiencing joy or positive emotions.
- Loss of interest in activities once enjoyed.
- Changes in Arousal and Reactivity
- Being easily startled or hypervigilant.
- Difficulty sleeping or concentrating.
- Irritability, anger outbursts, or heightened reactivity to stimuli.
When PTSD is Diagnosed
For a diagnosis of PTSD:
- Symptoms must persist for at least one month.
- They must cause significant impairment in daily functioning or relationships.
It’s important to note that not everyone exposed to trauma develops PTSD, and the severity of symptoms can vary widely among individuals.
Treatment Options for PTSD
Effective treatments for PTSD often combine psychotherapy and, in some cases, medication:
- Psychotherapy
- Cognitive Behavioral Therapy (CBT): Focuses on identifying and changing negative thought patterns related to the trauma.
- Exposure Therapy: Gradually helps individuals face and process traumatic memories in a safe environment.
- Eye Movement Desensitization and Reprocessing (EMDR): Combines talk therapy with guided eye movements to help process traumatic memories.
- Group Therapy: Provides support and understanding by connecting with others who share similar experiences.
- Medications
- Selective Serotonin Reuptake Inhibitors (SSRIs) like sertraline (Zoloft) or paroxetine (Paxil) are often prescribed to manage symptoms such as anxiety or depression.
- Prazosin may be used to reduce nightmares and improve sleep.
PTSD is a complex condition that requires a nuanced and compassionate approach to treatment. Early intervention, access to professional care, and support from loved ones are crucial in helping individuals manage symptoms and work toward recovery. Understanding the causes and manifestations of PTSD is the first step in breaking the stigma and fostering a supportive environment for healing.
Effective Treatments for Post-Traumatic Stress Disorder (PTSD)
Post-Traumatic Stress Disorder (PTSD) is a complex mental health condition that requires tailored treatment approaches to address its varied symptoms. Effective management often involves a combination of medications and psychotherapy. Below is an overview of common treatments for PTSD:
Medications
- Selective Serotonin Reuptake Inhibitors (SSRIs)
- Medications like sertraline (Zoloft) and paroxetine (Paxil) are FDA-approved for PTSD treatment.
- They help alleviate symptoms such as depression, anxiety, and intrusive thoughts by regulating serotonin levels.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
- Venlafaxine (Effexor XR) may also be prescribed to manage PTSD symptoms, especially when anxiety and depression coexist.
- Prazosin
- This medication is often used to reduce trauma-related nightmares and improve sleep quality in individuals with PTSD.
- Benzodiazepines
- These anti-anxiety drugs are used cautiously, as they carry risks of dependence and can sometimes exacerbate PTSD symptoms.
Psychotherapy
- Cognitive Behavioral Therapy (CBT)
- A gold-standard approach, CBT focuses on identifying and reframing negative thought patterns and behaviors associated with trauma.
- Exposure Therapy
- In a safe, controlled setting, individuals are gradually exposed to memories, emotions, or situations associated with the traumatic event, helping them process and diminish their emotional impact.
- Eye Movement Desensitization and Reprocessing (EMDR)
- EMDR combines guided eye movements or other forms of bilateral stimulation with trauma processing, reducing the intensity of traumatic memories.
- Cognitive Processing Therapy (CPT)
- CPT helps individuals analyze and reshape their thoughts and beliefs impacted by trauma, fostering healthier perspectives and coping strategies.
- Group Therapy
- Sharing experiences in a supportive group setting can provide understanding, community, and mutual encouragement for recovery.
Individualized Treatment Plans
Treatment for PTSD is highly individualized. Mental health professionals develop personalized plans based on the individual’s symptoms, trauma history, and preferences. As research continues to evolve, new therapeutic approaches and medications may enhance the effectiveness of PTSD treatment.
Managing PTSD often requires a comprehensive approach that combines medication and psychotherapy. With the guidance of skilled mental health professionals, individuals can find relief from symptoms and work toward recovery. By staying informed about available treatments and emerging advancements, individuals and their support systems can ensure access to the best possible care.
Understanding the Challenges of Treating Post-Traumatic Stress Disorder (PTSD)
Treating Post-Traumatic Stress Disorder (PTSD) presents unique challenges due to the complexity of the condition and the diverse needs of individuals affected by it. Despite the availability of evidence-based treatments, achieving optimal outcomes remains difficult for various reasons:
1. Individual Variability
PTSD manifests differently in each individual. Symptoms such as flashbacks, hypervigilance, emotional numbness, and avoidance vary in intensity and impact. This variability complicates the development of a one-size-fits-all treatment.
2. Co-Occurring Conditions
PTSD often overlaps with other mental health conditions like depression, anxiety disorders, or substance use disorders. Managing these comorbidities requires an integrated, often more intricate approach, which adds to treatment complexity.
3. Treatment Resistance
Not everyone responds to standard therapies or medications. Treatment-resistant PTSD cases may necessitate trial-and-error adjustments, alternative therapies, or a combination of modalities, prolonging the journey to relief.
4. Trauma Complexity
The nature and severity of trauma play a significant role in treatment difficulty. Complex traumas, such as prolonged abuse or multiple traumatic events, may require specialized and nuanced therapeutic strategies.
5. Stigma and Barriers to Treatment
The stigma associated with mental health conditions often discourages individuals from seeking help. Additionally, logistical barriers such as cost, accessibility, and lack of culturally sensitive care can further hinder treatment initiation and adherence.
6. Neurobiological Factors
PTSD is linked to changes in brain chemistry, genetics, and neural pathways, yet these mechanisms remain poorly understood. The intricate neurobiological underpinnings of PTSD contribute to the difficulty in creating universally effective treatments.
7. Chronic Nature of PTSD
For many, PTSD becomes a chronic condition, with symptoms persisting or recurring over the years. This chronicity demands long-term management and ongoing therapeutic engagement, which can be challenging to maintain.
8. Limited Treatment Options
While therapies like Cognitive Behavioral Therapy (CBT) and medications like SSRIs are effective for many, they do not work universally. The need for innovative treatment modalities is a significant area of focus in PTSD research.
9. Impact of Avoidance
Avoidance of trauma-related thoughts, emotions, or situations is a hallmark symptom of PTSD. This can hinder participation in therapies, such as exposure therapy, which require confronting distressing memories.
10. Patient Engagement
Maintaining consistent engagement in therapy or adherence to prescribed medications can be challenging. Factors such as lack of motivation, side effects, or emotional overwhelm may lead individuals to disengage from treatment prematurely.
Hope for the Future
Despite these challenges, advancements in PTSD research and treatment provide hope. Innovations such as trauma-focused therapies, emerging medications, and integrative approaches are improving outcomes. Addressing stigma, enhancing accessibility, and fostering a supportive environment are essential for promoting recovery.
PTSD is a multifaceted condition that demands a holistic, individualized approach to treatment. By addressing the unique challenges faced by individuals and fostering a culture of understanding and support, we can pave the way for more effective interventions and improved quality of life for those affected by PTSD.
Exploring the Use of Cannabis for PTSD: Potential Benefits and Considerations
Some individuals with Post-Traumatic Stress Disorder (PTSD) turn to cannabis as a complementary approach to managing their symptoms. While research is still emerging, anecdotal evidence and preliminary studies suggest that cannabis may offer relief for specific PTSD symptoms. Here are some reasons why individuals with PTSD might consider using cannabis, and essential considerations:
Potential Benefits of Cannabis for PTSD
1. Anxiety Reduction
Cannabis strains rich in cannabidiol (CBD) and low in tetrahydrocannabinol (THC) are reported to have anxiolytic (anxiety-reducing) effects. For many with PTSD, managing chronic anxiety is a priority, and cannabis may provide some relief.
2. Sleep Improvement
Sleep disturbances, including insomnia and nightmares, are common in PTSD. Certain cannabis strains with sedative properties may help individuals achieve better sleep quality and reduce nightmare frequency.
3. Mood Stabilization
Cannabis may help regulate mood swings and intense emotional responses, providing individuals with a sense of emotional balance.
4. Pain Relief
Chronic pain often coexists with PTSD. The analgesic (pain-relieving) properties of cannabis can contribute to a person’s overall well-being and improve their ability to function.
5. Relaxation and Stress Reduction
PTSD is associated with a state of constant hyperarousal. Cannabis can induce a sense of relaxation, potentially helping individuals manage stress and calm their heightened nervous system.
6. Enhanced Therapy Sessions
Some individuals report that using cannabis alongside traditional therapies, such as Cognitive Behavioral Therapy (CBT) or Eye Movement Desensitization and Reprocessing (EMDR), facilitates deeper emotional processing and openness during sessions.
7. Alternative to Pharmaceuticals
For those wary of the side effects of pharmaceutical medications or seeking a more natural approach, cannabis may be seen as a viable alternative for symptom management.
Important Considerations
- Lack of Conclusive Evidence
While early research and anecdotal accounts are promising, cannabis is not universally proven as an effective treatment for PTSD. Ongoing studies are needed to understand its long-term safety and efficacy. - Variability in Effects
The effects of cannabis can vary widely depending on the strain, dosage, and individual response. Strains high in THC, for example, may exacerbate anxiety or paranoia in some individuals. - Legal Status
The legal status of cannabis varies across countries and regions. Individuals need to be aware of and adhere to local laws regarding cannabis use. - Potential Risks
Cannabis use carries risks, including dependency, cognitive impairment, and exacerbation of mental health symptoms in susceptible individuals. These risks should be weighed against potential benefits. - Professional Guidance
Individuals considering cannabis for PTSD should consult healthcare professionals to discuss potential interactions with existing medications, appropriate dosing, and overall treatment goals.
Cannabis may offer potential therapeutic benefits for some individuals with PTSD, particularly in managing anxiety, improving sleep, and reducing hyperarousal. However, it is not a one-size-fits-all solution, and careful consideration of its risks, benefits, and legal implications is essential. Collaboration with healthcare providers ensures that individuals take an informed and evidence-based approach to integrating cannabis into their PTSD management plan. As research continues to evolve, the role of cannabis in PTSD treatment may become clearer, offering hope for those seeking alternative or complementary therapies.
The Scientific Rationale for Using Cannabis in PTSD Management
The use of cannabis to manage Post-Traumatic Stress Disorder (PTSD) has garnered increasing attention in recent years. The scientific basis for this potential therapy lies in the interaction between cannabinoids—the active compounds in cannabis—and the body’s endocannabinoid system (ECS). The ECS is involved in regulating key physiological processes, such as mood, stress response, and memory, which are often disrupted in PTSD.
The Role of the Endocannabinoid System (ECS)
1. Cannabinoid Receptors
The ECS consists of cannabinoid receptors, primarily CB1 and CB2:
- CB1 receptors are abundant in the brain and central nervous system. They are involved in processes such as mood regulation, memory, and fear extinction.
- CB2 receptors are predominantly found in peripheral tissues and the immune system, influencing inflammation and immune response.
2. Neurotransmitter Regulation
Cannabinoids, including endocannabinoids naturally produced by the body and phytocannabinoids from cannabis, interact with CB1 and CB2 receptors. Activation of CB1 receptors in the brain can influence the release of neurotransmitters like serotonin, which is crucial for mood stabilization and reducing anxiety.
3. Stress Response Modulation
The ECS helps regulate the body’s response to stress. Cannabis may modulate stress hormones such as cortisol, potentially reducing hyperarousal and promoting a sense of calm in individuals with PTSD.
4. Fear Extinction
Fear extinction, the process of unlearning conditioned fear responses, is particularly relevant to PTSD treatment. Preliminary studies suggest cannabinoids may influence memory consolidation and retrieval, potentially altering how traumatic memories are processed and reducing the emotional intensity associated with them.
Challenges and Considerations
While the interaction between cannabis and the ECS provides a scientific foundation for its use in PTSD management, several challenges remain:
- Limited Clinical Evidence: Current research is in the early stages, with much of the evidence based on preclinical or anecdotal findings.
- Individual Variability: The effects of cannabis can vary significantly based on factors such as the strain, dosage, and individual biology.
- Potential Risks: Cannabis use is associated with risks, including dependency, cognitive impairment, and exacerbation of mental health issues in some individuals.
- Legal and Regulatory Concerns: The legality of cannabis varies widely across regions, complicating its accessibility and consistent regulation.
The potential for cannabis to influence the ECS and address PTSD symptoms such as anxiety, hyperarousal, and traumatic memory recall provides a compelling scientific rationale for its use. However, the complexities of PTSD, combined with the variability of cannabis effects, highlight the need for more rigorous research to establish safe and effective treatment protocols.
Individuals considering cannabis for PTSD management should consult with healthcare professionals to discuss the risks and benefits, ensure compliance with local laws, and explore complementary therapies. With continued research, cannabis could become a valuable component of a comprehensive, individualized approach to PTSD treatment.
The Complexities of Accepting Cannabis as a Treatment for PTSD
The use of cannabis as a treatment for Post-Traumatic Stress Disorder (PTSD) remains a contentious and evolving topic. While some advocate for its potential therapeutic benefits, others express caution due to a range of scientific, legal, and clinical concerns. Several critical factors shape the acceptance of cannabis for PTSD treatment:
1. Limited Scientific Evidence
Though anecdotal reports and preliminary research suggest that cannabis may alleviate symptoms such as anxiety, sleep disturbances, and hyperarousal, robust scientific evidence is lacking. The absence of large-scale, placebo-controlled clinical trials makes it difficult to draw definitive conclusions about its efficacy and safety for PTSD.
2. Divergent Research Findings
Studies on cannabis and PTSD have produced mixed results. While some research points to potential symptom relief, other studies highlight risks such as increased dependence, exacerbation of mental health symptoms, and challenges in long-term use. This variability complicates its endorsement as a reliable treatment option.
3. Complex Chemical Composition
Cannabis contains numerous active compounds, primarily tetrahydrocannabinol (THC) and cannabidiol (CBD). THC is psychoactive and can affect cognition and memory, while CBD is non-psychoactive and may have anxiolytic and anti-inflammatory properties. The diverse compositions of cannabis strains and their varying THC-to-CBD ratios make standardizing treatment challenging.
4. Regulatory and Legal Hurdles
The legal status of cannabis is inconsistent worldwide and in different regions within countries. In many places, it is classified as a Schedule I controlled substance, impeding research opportunities and limiting its accessibility. These regulatory barriers make it challenging to integrate cannabis into mainstream PTSD treatment frameworks.
5. Concerns About Side Effects
Cannabis use can lead to side effects such as:
- Cognitive impairment and memory issues.
- Dependency or abuse, particularly with THC-rich strains.
- Potential worsening of mental health conditions in some users.
Healthcare professionals may be hesitant to recommend a substance with such risks, especially to individuals already struggling with trauma-related vulnerabilities.
6. Lack of Product Standardization
Unlike pharmaceutical drugs, which undergo rigorous testing and standardization, cannabis products vary widely in potency and formulation. This inconsistency raises concerns about dosing accuracy and the potential for unintended effects.
7. Established Alternative Treatments
Evidence-based therapies, such as cognitive-behavioral therapy (CBT), eye movement desensitization and reprocessing (EMDR), and selective serotonin reuptake inhibitors (SSRIs), are proven and widely accepted treatments for PTSD. Many healthcare professionals prefer these options due to their established safety and efficacy profiles.
Evolving Perspectives and Future Directions
Despite these challenges, perspectives on cannabis are shifting. With ongoing research into its therapeutic potential and changes in regulatory frameworks, there is hope for more clarity regarding its role in PTSD treatment. As scientific understanding deepens, cannabis may become a complementary option alongside established therapies.
Limited evidence, regulatory restrictions, and clinical concerns hinder the acceptance of cannabis for PTSD treatment. However, as attitudes evolve and research progresses, its potential therapeutic role may gain greater acceptance. Individuals considering cannabis for PTSD should seek guidance from healthcare professionals to navigate the risks, benefits, and legal considerations based on their unique needs and circumstances.
Frequently Asked Questions
Here are some common questions:
What is PTSD?
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after experiencing or witnessing trauma. Symptoms include flashbacks, nightmares, anxiety, hypervigilance, and emotional numbness.
Why do some people with PTSD use cannabis?
Many individuals use cannabis to cope with anxiety, insomnia, intrusive memories, or emotional distress when access to therapy or medication feels limited.
Does cannabis help PTSD symptoms?
Some people report short-term relief of anxiety or sleep problems. However, scientific evidence remains mixed, and benefits vary by individual and dosage.
Can cannabis worsen PTSD symptoms?
Yes. Heavy or long-term use may increase anxiety, paranoia, emotional detachment, or memory problems, potentially worsening PTSD over time.
Is cannabis an approved medical treatment for PTSD?
In the U.S., cannabis is not federally approved as a standard PTSD treatment, though some states allow medical cannabis for PTSD under local laws.
Can cannabis lead to dependence in people with PTSD?
Yes. Individuals using cannabis to self-medicate trauma symptoms are at higher risk of developing cannabis use disorder.
How does cannabis affect trauma processing?
Frequent use may blunt emotional responses, which can interfere with trauma-focused therapy and emotional healing.
Are there evidence-based treatments for PTSD besides cannabis?
Yes. Trauma-focused cognitive behavioral therapy, EMDR therapy, exposure therapy, and certain medications are proven effective.
Can cannabis be used alongside PTSD therapy?
This depends on the individual and treatment provider. Some clinicians advise limiting use to avoid interfering with emotional processing.
What are the signs that cannabis use is becoming harmful?
Needing increasing amounts, difficulty stopping, loss of motivation, memory issues, or using cannabis to avoid emotions are warning signs.
What alternatives help manage PTSD symptoms naturally?
Mindfulness, breathing techniques, physical activity, grounding exercises, peer support, and consistent therapy reduce symptoms over time.
Is recovery from PTSD possible without substance use?
Yes. With proper trauma-informed care and support, many individuals achieve significant symptom relief and improved quality of life.
Conclusion
Addressing Post-Traumatic Stress Disorder (PTSD) remains a complex endeavor, marked by the challenges inherent in existing treatment regimens. While psychotherapy and medication form the conventional approach, their variable efficacy and side effects underscore the need for alternative solutions. Cannabis has emerged as a potential option, supported by anecdotal evidence and ongoing scientific exploration. However, the acceptance of cannabis for PTSD treatment faces hurdles, including regulatory concerns and the need for more robust research. Balancing innovation with evidence-based practices is crucial as we navigate the intricate landscape of PTSD treatment, striving for solutions that offer effective relief while ensuring the highest standards of safety and efficacy.
Video: