Psychedelic-assisted therapy is a developing treatment that uses substances like psilocybin, MDMA, and ketamine to address mental health issues such as addiction and PTSD. It offers benefits like emotional healing and self-awareness, but also presents challenges, including legal barriers, misuse risks, and ethical concerns about safety and consent. Successful therapy relies on self-management strategies, family support, and community resources to help individuals sustain recovery and ensure long-term success.
Exploring Psychedelic-Assisted Therapy for Addiction
Psychedelic-assisted therapy for addiction is an emerging approach that combines the use of psychedelic substances with psychotherapy to help individuals address and overcome substance use disorders. This innovative treatment leverages the therapeutic effects of substances such as psilocybin (the active compound in magic mushrooms), MDMA, or ayahuasca, alongside psychological support, to facilitate profound emotional and psychological healing.
How It Works
The therapy typically involves a trained therapist guiding the individual through the experience, helping them process thoughts, emotions, and insights that arise during the psychedelic session. These substances can induce altered states of consciousness that allow individuals to confront deeply rooted emotional issues, trauma, and patterns of behavior associated with addiction. The aim is to reduce cravings, enhance self-awareness, and promote long-term behavioral changes.
The Science Behind It
Psychedelics are believed to disrupt default neural pathways, leading to heightened neuroplasticity temporarily—the brain’s ability to rewire itself. This can help individuals break free from compulsive patterns and develop healthier coping mechanisms. Studies have shown that substances like psilocybin and MDMA can increase emotional openness, decrease fear responses, and foster a sense of connection and meaning, all of which are crucial elements in addiction recovery.
Current Research and Challenges
Psychedelic-assisted therapy is still in the experimental stages, with ongoing research focused on its safety, efficacy, and potential to provide new pathways for recovery. Early clinical trials suggest promising results in treating various addictions, including alcohol and drug dependency. However, regulatory hurdles, ethical considerations, and the need for controlled clinical settings remain significant challenges. More research and clinical trials are needed to establish its role in addiction treatment fully.
The Future of Psychedelic Therapy
As scientific interest and societal acceptance grow, psychedelic-assisted therapy may become a mainstream option for addiction treatment. Institutions like Johns Hopkins University and MAPS (Multidisciplinary Association for Psychedelic Studies) are leading efforts to explore its potential. If approved for medical use, these treatments could offer hope for those struggling with addiction where traditional methods have failed.
While psychedelic-assisted therapy is not yet widely available, its potential to revolutionize addiction treatment is undeniable. With careful research and responsible implementation, it may soon offer a transformative pathway to healing for many individuals.
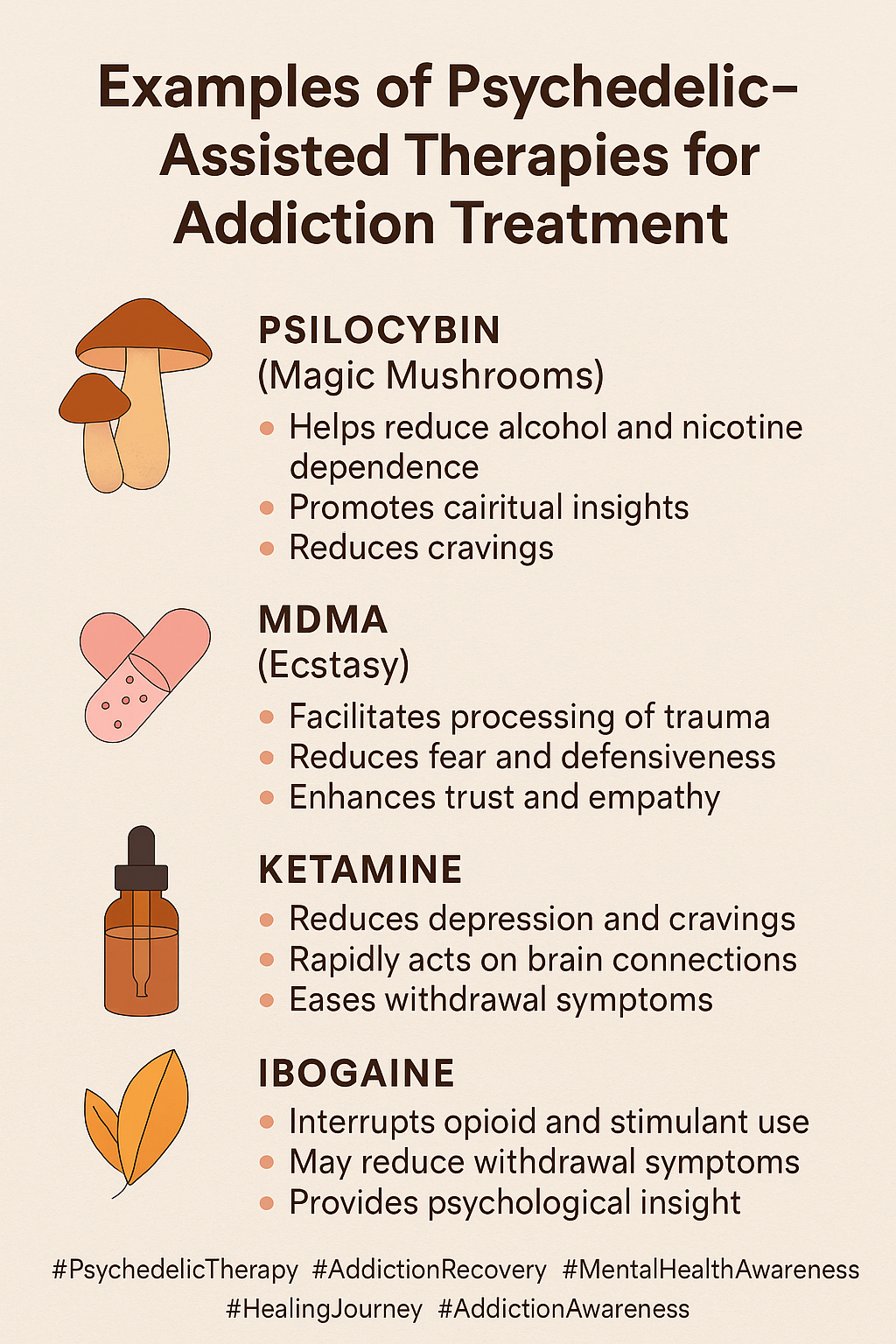
Examples of Psychedelic-Assisted Therapies for Addiction Treatment
Psychedelic-assisted therapies for addiction treatment involve the controlled administration of specific substances in therapeutic settings, paired with psychotherapy to address the root causes of addiction. Below are some well-known examples:
Psilocybin-Assisted Therapy
- Substance: Psilocybin, the active compound in “magic mushrooms.”
- Therapeutic Approach: Psilocybin is administered in a controlled setting alongside psychotherapy. Research suggests it helps individuals confront the emotional and psychological roots of addiction, reduce cravings, and shift harmful thought patterns.
- Applications: It has shown promise in treating alcohol addiction, smoking cessation, and other substance use disorders.
MDMA-Assisted Therapy
- Substance: MDMA (commonly known as ecstasy or molly), used in much smaller, controlled doses than in recreational settings.
- Therapeutic Approach: This therapy enhances emotional openness and empathy, helping individuals address trauma and emotional pain linked to addiction. MDMA is often used in combination with talk therapy to process difficult emotions and experiences.
- Applications: Primarily studied for PTSD treatment, but also explored for substance use disorders, particularly in cases where trauma has played a role in addiction.
Ayahuasca-Assisted Therapy
- Substance: Ayahuasca, a brew made from two plants native to the Amazon, containing the powerful hallucinogen DMT.
- Therapeutic Approach: Traditionally used in spiritual ceremonies, ayahuasca is now being explored in clinical settings to help individuals face deep-seated emotions and trauma. The intense psychological experience can shift perspectives and behaviors, leading to transformative healing.
- Applications: While more research is needed, some individuals with addiction have reported significant emotional breakthroughs, especially in cases of substance abuse linked to trauma or depression.
Ketamine-Assisted Therapy
- Substance: Ketamine, a dissociative anesthetic, is used in sub-anesthetic doses in a therapeutic setting.
- Therapeutic Approach: Ketamine is thought to induce dissociative states that allow patients to gain new insights into their addiction and mental health issues. It may also have neuroplastic effects that help “reset” the brain’s addiction pathways.
- Applications: Commonly used to treat depression, ketamine has also been studied for its potential in addressing alcohol and opioid addiction.
These therapies are currently part of clinical research and require professional oversight. The goal of psychedelic-assisted therapy is not recreational use but to harness the therapeutic potential of these substances to break the cycle of addiction and address its underlying psychological and emotional causes. With continued research, psychedelic-assisted therapies may become integral components of addiction treatment in the future.
Disadvantages of Psychedelic-Assisted Therapies in Addiction Treatment
While psychedelic-assisted therapy holds promise for treating addiction and other mental health disorders, it also has several disadvantages and potential risks. These include:
Psychological Risks
- Intense Emotional Reactions: Psychedelic experiences can bring up deeply suppressed emotions and memories, potentially leading to overwhelming psychological distress during or after the session. This is particularly concerning for individuals with a history of trauma, anxiety, or depression.
- Bad Trips: Some individuals may experience negative or frightening “trips” that lead to fear, paranoia, or confusion. These experiences can be unsettling and may lead to lasting anxiety or mistrust of the therapeutic process.
Unpredictability of Effects
- Individual Variability: The effects of psychedelics can vary significantly between individuals, making it difficult to predict how a person will respond. What works for one individual may not work for another.
- Altered Perception: The altered states of consciousness induced by psychedelics may not always lead to positive outcomes. Some individuals may experience disorientation, hallucinations, or confusion that complicate the therapeutic process.
Limited Research
- Lack of Long-Term Data: While early research into psychedelic-assisted therapy is promising, there is still a lack of long-term studies that explore the efficacy and safety of these therapies over extended periods.
- Regulatory and Legal Barriers: Psychedelic substances remain classified as controlled substances in many parts of the world, limiting access to therapy and research opportunities. This regulatory hurdle restricts the broader implementation of these treatments.
Potential for Abuse
- Misuse of Substances: Despite controlled settings, there is a risk that individuals might attempt to self-administer psychedelics outside of a therapeutic context, leading to misuse or unsafe recreational use.
- Escalation of Dependency: While psychedelics themselves are not physically addictive, their therapeutic use may encourage some individuals to seek them outside of treatment, particularly if they lack proper support systems.
Access and Cost
- Limited Availability: Psychedelic-assisted therapy is not widely available and is often restricted to clinical trials or specialized treatment centers, making it inaccessible for many who might benefit from it.
- High Cost: The therapy is often expensive, requiring multiple sessions with trained therapists and the administration of psychedelics in a controlled setting. This cost can be prohibitive for individuals without adequate financial resources or health insurance coverage.
Stigma and Social Resistance
- Cultural and Societal Stigma: Many people still associate psychedelics with recreational drug use or illicit activity, leading to the stigmatization of those seeking this form of therapy.
- Lack of Public Awareness: Many healthcare providers and the general public may be unfamiliar with psychedelic-assisted therapy, causing hesitancy or opposition to its use, even in clinical settings.
Potential for Unresolved Addiction Issues
- Not a Cure-All: While psychedelics can be a powerful tool for addressing underlying issues related to addiction, they are not a standalone cure. Without integration into a broader treatment plan that includes therapy and support, individuals may not fully resolve the root causes of their addiction.
Despite these disadvantages, many of these issues can be mitigated through professional oversight, adherence to ethical guidelines, and further research into the long-term effects and benefits of psychedelic-assisted therapy. However, these challenges highlight the need for careful consideration before widespread adoption.
Ethical Dilemmas of Psychedelic-Assisted Therapies in Addiction Treatment
Psychedelic-assisted therapy, while showing promise for treating addiction and other mental health conditions, presents several ethical dilemmas. These concerns primarily revolve around safety, informed consent, accessibility, and the potential for misuse. Here are some key ethical dilemmas:
Informed Consent
- Complexity of the Experience: Psychedelic therapy involves altered states of consciousness, which can be difficult for some individuals to understand or anticipate fully. Ensuring that patients provide truly informed consent is a significant challenge. Patients must fully comprehend the potential effects, both positive and negative, as well as the risks involved in their participation.
- Vulnerability of Participants: Some patients seeking psychedelic therapy may be in vulnerable mental states, such as dealing with addiction, trauma, or severe mental health issues. This raises questions about whether individuals can truly make informed decisions when they may be seeking desperate solutions to deep emotional pain.
Psychological Safety
- Risk of Psychological Harm: Psychedelics can bring up intense emotions or distressing memories, and the resulting “bad trips” may exacerbate existing mental health conditions, potentially causing long-term psychological harm. Adequate mental health support during and after therapy is crucial.
- Vulnerable Populations: Individuals with severe mental health issues like schizophrenia, psychosis, or personality disorders may be at heightened risk of adverse reactions. Ethically, there is a concern about offering psychedelic-assisted therapy to these individuals.
Therapist Responsibility and Boundaries
- Therapist’s Role in Integration: The therapist plays a critical role in guiding the patient and helping them integrate insights gained. Ethical dilemmas arise regarding the therapist’s responsibilities to maintain boundaries and ensure the patient’s well-being.
- Therapist Competency and Training: The field is still emerging, and not all therapists may be adequately trained in administering psychedelics safely. This lack of standardization raises concerns about ethical practices and patient safety.
Accessibility and Equity
- Cost and Inequality: Psychedelic-assisted therapy is often expensive and not widely available, raising ethical concerns about accessibility, particularly for low-income individuals or marginalized communities.
- Barriers to Access: Regulatory restrictions and stigma surrounding psychedelics limit their availability, reinforcing social disparities in healthcare access.
Addiction and Abuse Potential
- Misuse of Psychedelics: While generally not considered addictive, there is concern about individuals seeking to use them outside the therapeutic context, leading to misuse or unsafe recreational use.
- Perceived Normalization: As psychedelics gain popularity, there is a risk of the public perceiving them as harmless, potentially leading to unregulated use and ethical concerns about their responsible implementation.
Cultural Sensitivity and Appropriation
- Cultural Appropriation: Psychedelic therapy draws from indigenous practices that have used psychoactive substances for spiritual and healing purposes for centuries. The commercialization of these therapies raises concerns about cultural appropriation.
- Cultural Sensitivity in Therapy: Therapists need to be culturally competent and mindful of their patients’ diverse backgrounds, ensuring that therapy aligns with individuals’ cultural beliefs and values.
Long-Term Effects and Uncertainty
- Limited Research on Long-Term Effects: While early research is promising, there is still limited data on long-term consequences. Ensuring that individuals are fully aware of these uncertainties is a crucial ethical consideration.
While psychedelic-assisted therapy has the potential to revolutionize addiction and mental health treatment, it must be approached with caution. Addressing these ethical dilemmas requires careful regulation, proper therapist training, informed consent, and a commitment to equity and cultural sensitivity. Only with ethical practices in place can the therapeutic benefits of psychedelics be fully realized while minimizing potential harm.
Self-Management Strategies in Psychedelic-Assisted Therapy for Addiction Treatment
Psychedelic-assisted therapy is emerging as a promising approach to addiction treatment, offering profound insights and emotional breakthroughs. However, to maximize its therapeutic potential and ensure safety, individuals must adopt self-management strategies before, during, and after their psychedelic sessions. These strategies help facilitate integration, reduce risks, and support long-term healing.
1. Preparation Before Sessions
- Set Clear Intentions: Before the session, individuals should establish clear goals for what they hope to explore or achieve. This provides direction and focus, making the experience more meaningful.
- Mental and Emotional Readiness: Engaging in mindfulness, journaling, or self-reflection can help individuals prepare for potentially challenging emotions. Understanding personal triggers and emotional states can create a sense of preparedness for the session.
- Physical Preparation: Physical well-being plays a crucial role in a successful experience. Individuals should prioritize sleep, hydration, and avoiding substances like alcohol or other drugs that may interfere with the session.
- Build Trust with the Therapist: A strong therapeutic alliance fosters a safe and supportive environment. Establishing trust with the therapist ensures individuals feel secure during their journey.
2. During the Session
- Surrender to the Experience: Psychedelic therapy requires an open mind. Resisting the emotions or visions that arise can create distress, whereas surrendering allows for deeper exploration and healing.
- Focus on Breathing and Mindfulness: During intense moments, practicing deep breathing and mindfulness can help individuals stay grounded and navigate anxiety or discomfort.
- Stay Connected to the Therapist: Therapists play a crucial role in providing reassurance and grounding support. Individuals should openly communicate with the therapist when needed.
3. Integration After the Session
- Reflect on the Experience: Journaling, meditation, or discussing insights with a therapist can help individuals process and make sense of their experiences.
- Actionable Steps: Translating insights into real-life changes is essential for lasting therapeutic success. Setting specific goals and implementing lessons learned fosters personal growth.
- Self-Care Practices: Post-session self-care—such as relaxation techniques, exercise, or connecting with loved ones—supports emotional well-being and recovery.
- Ongoing Therapy and Support: Continued therapy and community support groups provide accountability and reinforce positive changes over time.
4. Cultivate a Growth Mindset
- Embrace Change: Psychedelic experiences may bring forth challenging emotions. Recognizing that healing is a process can help individuals approach their journey with acceptance and adaptability.
- Patience and Self-Compassion: Self-discovery takes time. Practicing patience and self-compassion helps individuals navigate setbacks without discouragement.
5. Track Progress
- Monitor Emotional and Mental Health: Tracking emotions, behaviors, and thought patterns over time helps reinforce progress and identify areas needing further attention.
- Use of Journals or Tracking Apps: Recording experiences and insights in a journal or app allows individuals to monitor integration and track changes in mindset and behavior.
6. Develop a Strong Support Network
- Engage with a Supportive Community: A network of supportive peers, friends, or family reinforces lessons learned and provides encouragement.
- Therapist Check-ins: Regular follow-ups with a therapist ensure continued guidance and help address challenges that arise after the session.
By employing these self-management strategies, individuals can enhance the benefits of psychedelic-assisted therapy, reduce risks, and maintain long-term healing in their addiction recovery journey. Through preparation, integration, and support, psychedelic therapy can be a powerful tool for transformation and personal growth.
Family Support Strategies in Psychedelic-Assisted Therapy for Addiction Treatment
Family support plays a crucial role in psychedelic-assisted therapy, particularly for individuals dealing with addiction, trauma, or mental health issues. By offering emotional, psychological, and logistical support before, during, and after therapy, family members can significantly contribute to the success of the healing process. Below are key family support strategies to optimize the benefits of psychedelic-assisted therapy.
1. Education and Understanding
- Learn About the Process: Family members should educate themselves on psychedelic-assisted therapy, its potential benefits, risks, and the therapeutic framework. Understanding how psychedelics work therapeutically allows families to offer informed support.
- Normalize the Experience: Families can help reduce stigma by acknowledging psychedelic therapy as a legitimate and research-backed approach to addiction treatment. A supportive, non-judgmental atmosphere enhances the individual’s comfort and trust in the process.
2. Preparation and Encouragement
- Offer Emotional Support Before the Session: Providing reassurance and encouragement can help individuals feel safe and supported before their session. A calm and positive mindset is essential for maximizing the therapeutic experience.
- Create a Safe Environment: A peaceful, distraction-free setting before and after the session contributes to a more effective healing process. Family members can ensure the person feels physically and emotionally secure.
3. During the Session
- Respect Boundaries and Privacy: Since trained professionals typically guide therapy sessions, family members should respect the individual’s need for privacy and autonomy during the process.
- Refrain from Judgment: Even if family members are not directly involved in the session, maintaining an open-minded, non-judgmental attitude afterward fosters open, honest discussions about the experience.
4. Post-Session Support
- Be Available for Integration: Families can support the integration process by being present for conversations, actively listening, and offering a compassionate space for the individual to process insights gained during the session.
- Support Emotional Regulation: Post-therapy vulnerability is common. Families can help individuals navigate emotional responses by offering comfort and stability during this period of adjustment.
- Encourage Reflection: Asking open-ended questions and engaging in discussions about the experience can help the individual make sense of their emotions and insights, reinforcing the long-term benefits of therapy.
5. Encourage Healthy Lifestyle Choices
- Promote Self-Care and Wellness: Supporting good habits such as proper sleep, nutrition, and exercise reinforces the positive effects of therapy and aids in overall well-being.
- Support in Avoiding Triggers: Family members should help identify and minimize exposure to triggers that could lead to substance use or unhealthy behaviors, reinforcing the individual’s commitment to recovery.
6. Facilitate Ongoing Therapy
- Encourage Continued Professional Support: Supporting ongoing therapy and integration sessions is essential in maintaining progress and addressing lingering challenges that may arise after psychedelic experiences.
- Participate in Family Counseling: Family therapy sessions can help resolve relational issues contributing to addiction, promoting healing for both the individual and their family members.
7. Patience and Compassion
- Be Patient with the Process: Healing through psychedelic-assisted therapy is often non-linear. Families must exercise patience and provide unconditional support as individuals navigate their recovery journey.
- Provide Encouragement in Challenging Moments: Emotional distress may arise post-therapy. Offering empathy and encouragement without pressuring the individual to move through their emotions too quickly fosters a supportive healing environment.
8. Create a Supportive Home Environment
- Foster a Positive and Safe Environment: A calm, stress-free, and nurturing home environment enhances the therapeutic benefits of the experience and supports sustained recovery.
- Celebrate Progress: Recognizing and celebrating milestones, no matter how small, boosts motivation and reinforces the individual’s commitment to healing.
By providing education, emotional support, patience, and encouragement, family members can play a significant role in the success of psychedelic-assisted therapy. Their involvement ensures that the individual feels supported, safe, and empowered to integrate the lessons learned into their daily life, leading to lasting recovery and personal growth.
Community Resource Strategies for Psychedelic-Assisted Therapy in Addiction Treatment
Psychedelic-assisted therapy has emerged as a promising approach for treating addiction, offering individuals profound insights and emotional healing. However, ensuring the success and accessibility of this therapy requires strong community support systems. Community resource strategies play an essential role in reducing stigma, facilitating safe access, and fostering long-term recovery. Here are key strategies communities can implement to support psychedelic-assisted therapy for addiction treatment.
1. Public Education and Awareness Campaigns
- Raising Awareness: Communities can organize educational programs to inform the public about the benefits, risks, and scientific backing of psychedelic-assisted therapy. This reduces stigma and promotes informed, open-minded discussions about its potential as a treatment for addiction, mental health disorders, and trauma.
- Dispelling Myths: It’s crucial to challenge misconceptions surrounding psychedelics. Public education can help reframe these substances as evidence-based therapeutic tools rather than illicit drugs, fostering broader acceptance and understanding.
2. Access to Trained Professionals
- Facilitating Access to Qualified Therapists: Communities can work with mental health organizations, universities, and regulatory bodies to ensure that therapists and clinicians are appropriately trained and licensed in psychedelic-assisted therapy. This ensures that individuals receive high-quality, ethical care.
- Expanding Training Programs: Community-based organizations can collaborate with educational institutions to provide specialized training programs, equipping mental health professionals with the skills needed for safe and effective psychedelic-assisted therapy.
3. Support Groups and Peer Networks
- Psychedelic Integration Support Groups: Communities can establish peer support groups where individuals can share their experiences and challenges following psychedelic therapy. These groups provide emotional support, coping strategies, and encouragement throughout the recovery process.
- Ongoing Emotional Support: Connecting individuals who have undergone similar healing journeys fosters a sense of belonging and helps prevent isolation during the integration process.
4. Integration Programs
- Psychedelic Integration Services: Local recovery centers and mental health organizations can offer integration programs to help individuals process their psychedelic experiences. These services may include counseling, group therapy, and guided reflection workshops.
- Workshops and Seminars: Hosting workshops that focus on integrating psychedelic experiences into everyday life, personal growth, and long-term recovery can enhance the therapy’s effectiveness.
5. Legislative and Policy Advocacy
- Promoting Legal Access: Communities can advocate for policy changes that support legal access to psychedelic-assisted therapy. This includes pushing for government-approved clinical trials, insurance coverage, and regulatory frameworks.
- Decriminalization Efforts: Supporting efforts to decriminalize therapeutic psychedelics can reduce stigma and create more opportunities for research and treatment accessibility.
6. Culturally Sensitive Resources
- Tailoring Therapy to Specific Communities: Culturally responsive programs ensure that psychedelic-assisted therapy is accessible and relevant to diverse populations. This includes providing services in multiple languages and training therapists to understand different cultural perspectives on healing.
- Engaging with Indigenous Healing Traditions: Many indigenous cultures have long histories of using plant medicine for healing. Collaborating with indigenous healers can enrich psychedelic therapy frameworks with traditional wisdom.
7. Holistic Health Support
- Complementary Health Services: Communities can integrate psychedelic-assisted therapy with holistic wellness practices such as meditation, yoga, nutrition counseling, and art therapy to support overall well-being.
- Access to Mental Health Services: Ensuring that individuals have access to ongoing mental health support, including traditional therapy and counseling, complements psychedelic-assisted treatment.
8. Collaboration with Recovery Communities
- Integrating with Addiction Recovery Programs: Psychedelic-assisted therapy can complement traditional recovery programs like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) by addressing underlying trauma and mental health issues.
- Specialized Treatment Centers: Establishing dedicated treatment centers that incorporate psychedelic therapy into comprehensive addiction recovery plans can enhance long-term success rates.
9. Funding and Accessibility Initiatives
- Increasing Research Funding: Advocacy for increased funding in psychedelic therapy research can help validate its effectiveness and expand accessibility.
- Financial Assistance Programs: Local organizations can offer financial aid, sliding-scale fees, and scholarships for those who cannot afford treatment, making therapy more inclusive.
10. Aftercare Support
- Post-Therapy Follow-Up: Providing structured aftercare support through regular check-ins, continued therapy sessions, and peer support can help individuals maintain their progress in recovery.
- Continuous Support Services: Communities should ensure long-term mental health support, access to social services, and engagement in recovery programs to sustain the benefits of therapy.
By implementing these community resource strategies, we can create an environment where psychedelic-assisted therapy is accessible, effective, and integrated into broader health and recovery systems. A supportive community network not only reduces stigma but also empowers individuals to achieve lasting healing and personal growth.
Frequently Asked Questions
Here are some common questions:
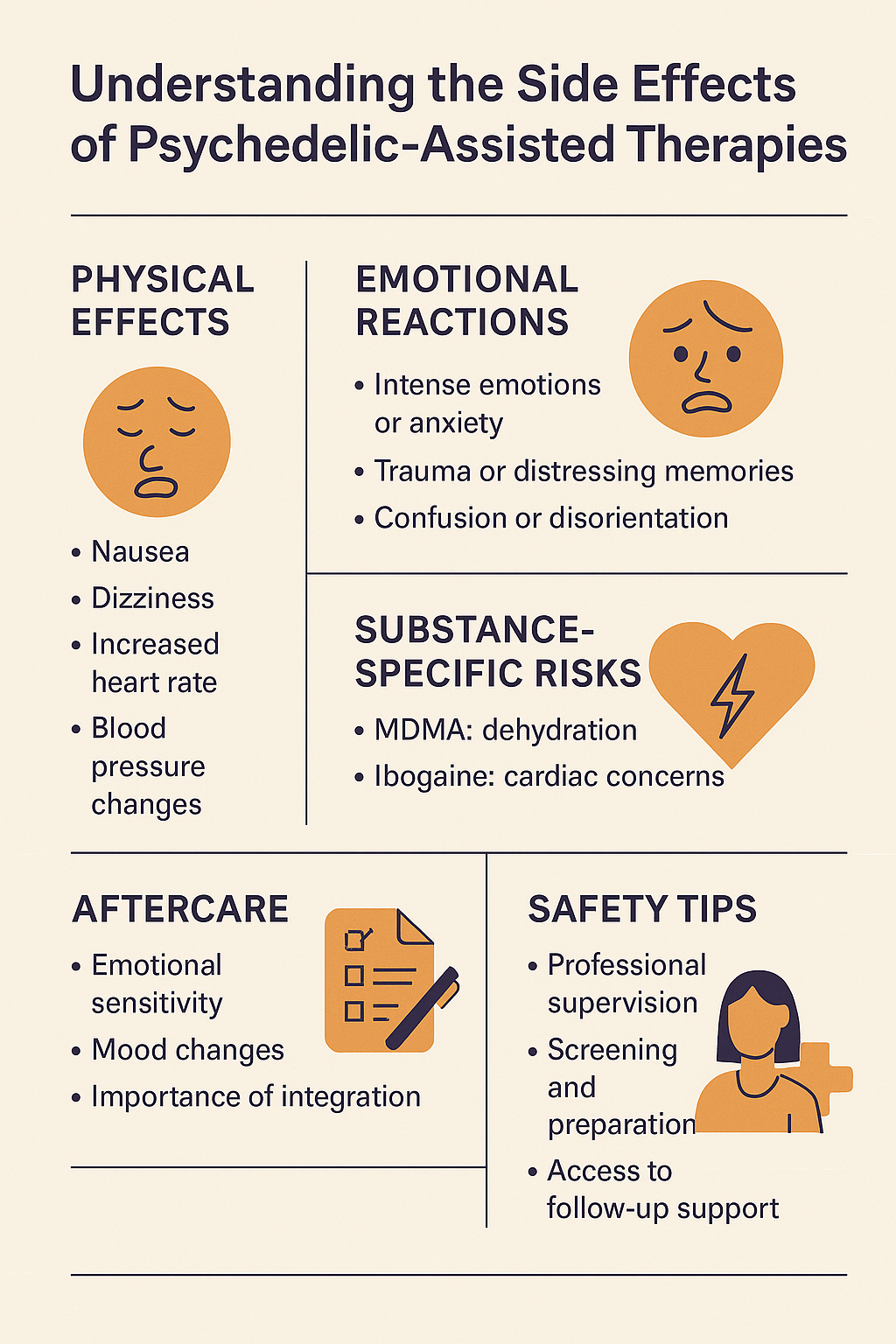
Question: What are the side effects of Psychedelic-Assisted Therapies?
Answer: Psychedelic-assisted therapies (PAT) can be highly effective for treating addiction, PTSD, depression, and other mental health conditions, but they also come with potential side effects. These effects vary based on the substance used, individual physiology, mental state, and therapeutic setting. Below are some common side effects:
1. Psychological Side Effects
- Intense Emotional Responses: Psychedelics can bring up deep-seated emotions, which may be overwhelming or distressing.
- Hallucinations & Perceptual Distortions: Visual, auditory, and sensory distortions can occur, sometimes leading to confusion or distress.
- Paranoia & Anxiety: Some individuals may experience heightened anxiety, paranoia, or even panic attacks during the session.
- Flashbacks (HPPD – Hallucinogen Persisting Perception Disorder): Some individuals experience lingering visual distortions or flashbacks after their experience.
- Psychotic Episodes: Those with a history of schizophrenia or bipolar disorder may be at higher risk of experiencing a psychotic break.
2. Physical Side Effects
- Nausea & Vomiting: Common with substances like ayahuasca or psilocybin mushrooms.
- Increased Heart Rate & Blood Pressure: Some psychedelics (like MDMA and LSD) can cause cardiovascular strain.
- Headaches & Dizziness: Can occur post-session, particularly with psilocybin.
- Temperature Dysregulation: Sweating, chills, or fever-like symptoms can be common.
3. Long-Term Risks
- Emotional Vulnerability Post-Therapy: Individuals may feel emotionally raw or vulnerable after their experience.
- Dependence Risk (Minimal but Possible): While most psychedelics are not physically addictive, improper use or repeated recreational use can lead to psychological dependence.
- Integration Challenges: Some individuals struggle to make sense of their psychedelic experience, leading to confusion, existential distress, or difficulty reintegrating into daily life.
How to Minimize Risks
Post-Therapy Integration Support: Proper integration therapy can help process and make sense of the experience.
Screening for Mental Health Conditions: Patients with a history of schizophrenia or psychosis should avoid psychedelics.
Therapeutic Setting & Guidance: A controlled environment with trained professionals reduces risks.
Question: What are the side effects of Psilocybin?
Answer: Psilocybin, the active compound in psychedelic mushrooms, has both short-term and potential long-term side effects. While it is generally considered physiologically safe, its psychological effects can vary widely depending on dosage, individual sensitivity, and setting.
Short-Term Side Effects
- Psychological Effects:
- Altered Perception: Visual and auditory hallucinations, time distortion, and synesthesia (mixing of senses, such as “seeing” sounds).
- Euphoria & Increased Emotional Sensitivity: Many users experience deep emotions, joy, or spiritual insights.
- Anxiety, Paranoia, or Fear: Higher doses can lead to overwhelming experiences, sometimes referred to as a “bad trip.”
- Confusion or Disorientation: Difficulty understanding reality, which may cause distress.
- Impaired Judgment: Risky behavior or accidents due to altered perception.
- Physical Effects:
- Nausea & Vomiting: Common, especially at higher doses.
- Dizziness & Lightheadedness: May cause temporary imbalance.
- Increased Heart Rate & Blood Pressure: Can be problematic for those with heart conditions.
- Muscle Weakness or Tremors: Some users report feeling physically shaky or weak.
- Pupil Dilation & Sensitivity to Light: Vision may be affected, making bright lights uncomfortable.
Long-Term Risks
- Hallucinogen Persisting Perception Disorder (HPPD):
- Some individuals experience flashbacks or lingering visual disturbances (e.g., seeing trails or halos around objects) after using psilocybin.
- Psychological Vulnerability:
- In rare cases, psilocybin may trigger or exacerbate latent mental health conditions like schizophrenia or bipolar disorder.
- Depersonalization or Existential Anxiety:
- Some individuals struggle to integrate their psychedelic experience, leading to a sense of detachment or existential confusion.
- Emotional Sensitivity Post-Trip:
- Increased vulnerability, requiring support and integration to process the experience.
How to Minimize Risks
Integration Support: Post-trip therapy or support groups can help process the experience.
Set & Setting: Being in a safe, controlled environment with a trusted guide or therapist can reduce risks.
Proper Dosing: Start with lower doses under supervision.
Screening for Mental Health Risks: Those with schizophrenia, psychotic disorders, or severe anxiety may be at higher risk of adverse effects.
Question: What are the side effects of Ketamine?
Answer: Ketamine, a dissociative anesthetic used in psychedelic-assisted therapy for depression, PTSD, and addiction, has several potential short-term and long-term side effects.
Short-Term Side Effects
- Psychological Effects:
- Dissociation (“Out-of-Body” Experience): A feeling of detachment from reality, oneself, or surroundings.
- Hallucinations & Perceptual Distortions: Visual, auditory, or sensory changes, including time distortion.
- Euphoria & Mood Elevation: Many people experience deep relaxation or a sense of well-being.
- Anxiety, Confusion, or Paranoia: Higher doses or individual sensitivity can trigger distress.
- Cognitive Impairment: Temporary difficulty with memory, thinking, and concentration.
- Physical Effects:
- Increased Heart Rate & Blood Pressure: Can be risky for individuals with heart conditions.
- Dizziness & Loss of Coordination: May cause difficulty walking or moving.
- Nausea & Vomiting: Common during or after infusion.
- Nystagmus (Rapid Eye Movements): Involuntary eye movements, which can be disorienting.
- Slurred Speech: Similar to alcohol intoxication at higher doses.
Long-Term Side Effects
- Bladder & Urinary Issues (Ketamine Cystitis):
- Chronic use can lead to painful urination, bladder inflammation, and in severe cases, permanent damage.
- Cognitive & Memory Impairment:
- Frequent or high-dose use may affect memory, attention, and executive function.
- Psychological Risks:
- Can exacerbate symptoms in people with underlying psychotic disorders (e.g., schizophrenia).
- Some users report persistent dissociation or difficulty reintegrating into daily life.
- Addiction & Dependence:
- Although less common in clinical settings, ketamine has addictive potential when misused recreationally.
How to Minimize Risks in Therapy
Integration Support: Helps process and make sense of the experience.
Medical Supervision: Proper screening and monitoring during treatment.
Controlled Dosing: Administered in a clinical setting to reduce risks of adverse effects.
Hydration & Bladder Care: Prevents urinary complications.
Conclusion
Psychedelic-assisted therapy presents a promising approach to treating addiction and other mental health conditions by fostering deep emotional healing and self-awareness. However, it faces challenges including legal barriers, the risk of misuse, and ethical concerns about patient safety and consent. To maximize its effectiveness, self-management strategies, family support, and community resources play a vital role in helping individuals navigate their recovery journey. While further research and ethical considerations are necessary, psychedelic-assisted therapy has the potential to transform addiction treatment when approached responsibly and with appropriate support systems.
Videos: Psychedelics Might Change Rehab Forever!
How Psychedelic Therapy Fights Cravings!
The Shocking TRUTH About Psychedelic Therapy Side Effects