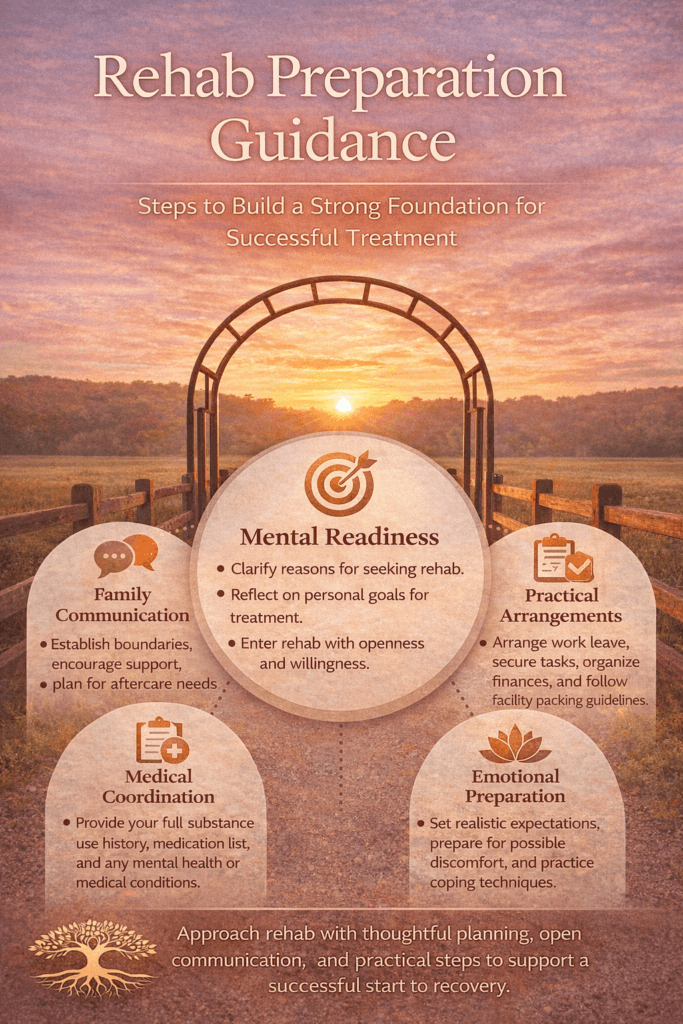
Preparing for rehab is a pivotal step that can strongly influence both immediate treatment success and long-term recovery stability. Entering a structured program involves more than arrival—it requires mental readiness, practical organization, and emotional preparation. Individuals who clarify their reasons for treatment, understand what rehab involves, and set personal goals often begin with greater motivation and openness to change. Thoughtful preparation also stabilizes outside responsibilities—such as finances, work leave, or family arrangements—so attention can remain focused on healing rather than unresolved stressors. It also helps set realistic expectations about challenges like withdrawal discomfort and emotional vulnerability, reducing fear and increasing engagement. When viewed not as a last-minute step but as the first intentional phase of recovery, preparation becomes a meaningful commitment that builds confidence and lays the groundwork for lasting change.
Preparation Guide for Rehab: How to Get Ready for Treatment and Recovery
Entering rehab is a courageous and life-changing decision. Preparation can significantly improve engagement, reduce anxiety, and increase the likelihood of long-term recovery. Whether treatment involves inpatient rehabilitation, outpatient programs, or medication-assisted therapy, thoughtful planning supports a smoother transition into care.
The first step in preparing for rehab is mental readiness. Individuals should reflect on their motivations for change and clarify personal goals. Writing down reasons for seeking treatment—improved health, restored relationships, professional stability, or legal resolution—helps reinforce commitment during challenging moments. Programs such as Alcoholics Anonymous often emphasize willingness as the foundation of recovery; entering treatment with openness rather than resistance strengthens outcomes.
Practical preparation is equally important. Arrange work leave through FMLA if applicable, notify essential contacts, secure childcare, and organize finances. For inpatient programs, pack according to facility guidelines: comfortable clothing, approved hygiene items, identification, insurance documentation, and prescribed medications in their original containers. Avoid bringing prohibited items, including substances, weapons, or unapproved electronics.
Medical coordination should occur before admission. Provide a complete substance use history, current medications, psychiatric diagnoses, and prior treatment experiences. If detoxification is anticipated, discuss withdrawal risks with healthcare providers to ensure appropriate medical monitoring.
Emotional preparation includes setting realistic expectations. Rehab is structured and may involve therapy, group counseling, education sessions, family meetings, and relapse prevention planning. Treatment can feel uncomfortable at times as underlying trauma, guilt, or grief surfaces. Understanding that discomfort is part of healing reduces premature dropout.
Family communication is another key element. Establish boundaries regarding visitation, communication schedules, and financial involvement. Encourage supportive relatives to seek their own education or peer support during your treatment.
Finally, approach rehab as the beginning—not the end—of recovery. Discharge planning, outpatient follow-up, peer support, and lifestyle restructuring are essential for long-term success. Treatment provides stabilization, skill-building, and foundation work. Sustainable recovery develops through continued engagement.
Preparation transforms rehab from a crisis response into a strategic turning point. With thoughtful planning, honest communication, and a willingness to participate fully, individuals can enter treatment equipped for meaningful change and long-term healing.
Self-Management Strategies for Rehab Preparation: A Practical Guidance Plan
Preparing for rehab is not just about packing a bag or arranging time off work—it is an opportunity to begin recovery before treatment officially starts. Self-management strategies help individuals enter rehab with clarity, structure, and readiness for change. The more intentional the preparation, the stronger the foundation for long-term success.
The first strategy is intentional goal setting. Before admission, write down clear and realistic objectives: detox safely, understand relapse triggers, stabilize mental health, rebuild family trust, or develop coping skills. Aligning treatment with personal goals increases engagement and reduces resistance. Programs such as Alcoholics Anonymous emphasize willingness as a cornerstone of change; defining your “why” strengthens that willingness.
Emotional regulation is another key self-management tool. Anxiety about detox, group therapy, or vulnerability is normal. Practice grounding techniques such as deep breathing, journaling, light exercise, or guided mindfulness to stabilize mood before entering treatment. Developing these skills early allows smoother adaptation to the structured rehab environment.
Practical organization also reflects self-management. Create a checklist: confirm insurance coverage, arrange leave from work, organize medications, secure childcare, and pay critical bills in advance. Completing logistical tasks reduces external stressors that could distract from treatment focus.
Cognitive preparation is equally important. Replace catastrophic thoughts (“This will ruin everything”) with realistic reframing (“This is a step toward rebuilding stability”). Understanding that discomfort during therapy is part of healing can prevent early withdrawal from treatment.
Boundary setting is another crucial strategy. Identify individuals who may trigger cravings or minimize the need for treatment. Limit contact before admission and commit to prioritizing recovery over social pressure. Protecting your treatment decision reinforces autonomy.
Lastly, begin adopting small recovery behaviors before rehab starts. Reduce substance use if medically safe, attend a peer support meeting, establish a consistent sleep routine, and practice honest communication. These early actions signal commitment and create psychological momentum.
Rehab is not a passive experience—it requires participation. By practicing self-management strategies in advance, individuals enter treatment prepared not just to attend, but to engage. Preparation transforms rehab from a crisis intervention into a purposeful beginning of recovery.
Family Support Strategies for Rehab Preparation: A Guide to Strengthening Recovery Before Treatment Begins
When a loved one decides to enter rehab, the period before admission is critical. Family involvement during this stage can either reduce anxiety and strengthen commitment or unintentionally increase stress. Effective family support strategies focus on structure, education, emotional stability, and healthy boundaries.
The first strategy is education. Families should learn about substance use disorder as a chronic medical condition rather than a moral failing. Understanding withdrawal, relapse risk, co-occurring mental health conditions, and treatment structure reduces stigma and fear. Attending open meetings or family-oriented groups connected to organizations like Al-Anon Family Groups or open sessions of Alcoholics Anonymous can provide insight into recovery dynamics and boundary setting.
Second, families can help reduce logistical stress. Assisting with insurance verification, arranging transportation, managing temporary childcare, securing work documentation, or organizing medications allows the individual to focus on emotional readiness. However, support should not cross into over-control. Empowering people to take responsibility for their own preparation fosters accountability.
Communication is another cornerstone. Encourage open, calm conversations about treatment expectations. Avoid ultimatums or shaming language. Instead of saying, “You better not fail again,” consider, “We’re proud you’re taking this step, and we’ll support your effort.” Affirmation increases motivation and reduces defensive resistance.
Boundary setting is equally important. Families should clarify financial, housing, and behavioral expectations both during and after treatment. Clear agreements prevent enabling and protect long-term stability. Support does not mean removing all consequences—it means responding with compassion while maintaining structure.
Emotional regulation within the family system also matters. Loved ones often experience fear, guilt, anger, or exhaustion. Seeking counseling or peer support helps families manage their own stress so they can respond thoughtfully rather than reactively.
Finally, begin planning for post-rehab continuity. Discuss outpatient follow-up, sober living options, transportation to meetings, and family therapy participation. Recovery does not end at discharge; preparation should reflect long-term thinking.
When families provide informed, structured, and compassionate support, they transform rehab preparation into a collaborative effort. A stable family environment before admission increases the likelihood of engagement, retention, and sustainable recovery outcomes.
Community Resource Strategies for Rehab Preparation: Building a Strong Support Network Before Treatment Begins
Preparing for rehab is not solely an individual or family effort—it is also a community-supported transition. Effective community resource strategies reduce barriers, increase engagement, and create a smoother pathway into treatment. When individuals are connected to the right systems before admission, they enter rehab with stability rather than crisis-driven chaos.
One of the most important community strategies is early referral and screening. Primary care clinics, behavioral health providers, urgent care centers, and emergency departments play a vital role in identifying substance use disorders and connecting patients to appropriate levels of care. Coordinated referral systems reduce delays that can weaken motivation. In your clinical setting, as a PA, structured screening tools and rapid linkage pathways can significantly improve treatment entry timelines.
Peer recovery organizations also serve as foundational bridges. Programs such as Alcoholics Anonymous and Narcotics Anonymous offer immediate community connection even before formal rehab admission. Attending meetings prior to entering treatment familiarizes individuals with recovery language, sponsorship models, and accountability structures.
Community health departments and nonprofit organizations often assist with logistical barriers, including transportation vouchers, housing referrals, childcare coordination, and insurance navigation. These practical supports reduce external stressors that might otherwise derail treatment plans. Recovery community centers often provide peer coaching, intake navigation, and structured orientation services.
Legal and workplace systems can also be leveraged strategically. Courts may support treatment referrals in diversion programs, and employers may provide medical leave options such as FMLA. Coordinated communication between healthcare providers and employers ensures privacy while facilitating stability.
Faith-based organizations and volunteer networks can further expand support, offering mentorship, sober social activities, and spiritual guidance. These networks help individuals feel a sense of belonging before rehab begins, reinforcing their commitment to change.
Finally, integrated care coordination is essential. Collaboration among medical providers, therapists, case managers, and social workers ensures that medication management, mental health treatment, and detox planning are aligned. This reduces fragmentation and improves continuity of care.
Community resource strategies transform rehab preparation from an isolated decision into a supported transition. When communities build accessible, coordinated, and stigma-free systems, individuals enter treatment equipped with structure, encouragement, and sustainable support networks.
Frequently Asked Questions
Here are some common questions:
1. How do I know if I’m ready for rehab?
You don’t have to feel completely ready to begin treatment. Willingness—not certainty—is the key starting point. If substance use is affecting your health, relationships, work, or safety, seeking help is a strong indicator that rehab may be appropriate.
2. What should I do first when planning for rehab?
Start with an assessment from a healthcare provider or treatment center. They can determine the appropriate level of care (detox, inpatient, outpatient, or intensive outpatient) based on medical, psychological, and substance use history.
3. What should I pack for inpatient rehab?
Bring comfortable clothing, identification, insurance information, approved toiletries, prescribed medications in original bottles, and a list of emergency contacts. Facilities usually provide a packing list and specify prohibited items.
4. Should I stop using substances before admission?
Not always. Some substances require medical supervision during withdrawal. Always consult a clinician before attempting to stop use independently, especially with alcohol, benzodiazepines, or opioids.
5. How can I prepare mentally for rehab?
Clarify your reasons for seeking treatment, set realistic expectations, and understand that discomfort is part of the healing process. Journaling goals and fears can help organize thoughts before admission.
6. What practical arrangements should I make beforehand?
Arrange time off work, secure childcare or pet care, pay essential bills, notify necessary contacts, and plan transportation. Reducing outside stressors helps you focus fully on treatment.
7. Should my family be involved in preparation?
Yes, when safe and appropriate. Supportive family members can assist with logistics, emotional encouragement, and aftercare planning. Family education programs can also help them understand addiction and recovery.
8. What if I feel anxious or scared about rehab?
This is completely normal. Fear of the unknown, withdrawal symptoms, or vulnerability in therapy are common concerns. Talking with a counselor or someone who has attended treatment can ease anxiety.
9. Do I need a plan for after rehab before I go?
It helps. Thinking ahead about outpatient therapy, sober housing, peer support meetings, and lifestyle changes prepares you for continuity of care once treatment ends.
Programs such as Alcoholics Anonymous or Narcotics Anonymous are often recommended as part of aftercare support.
10. What is the most important mindset to have before entering rehab?
Openness. Treatment works best when individuals are willing to participate honestly, try new coping strategies, and accept guidance. Progress—not perfection—is the goal.
Conclusion
Rehab preparation transforms treatment from a crisis response into a purposeful transition toward recovery. When individuals approach admission with realistic expectations, organized responsibilities, and a willingness to engage, they increase their chances of benefiting from therapy, skill-building, and support systems. Preparation also helps families and care providers coordinate effectively, creating stability before treatment even begins. Ultimately, the steps taken before entering rehab reflect a commitment to change. Thoughtful preparation does not guarantee an easy journey, but it strengthens resilience, reduces barriers, and positions individuals to begin recovery with clarity, readiness, and hope.
Video: