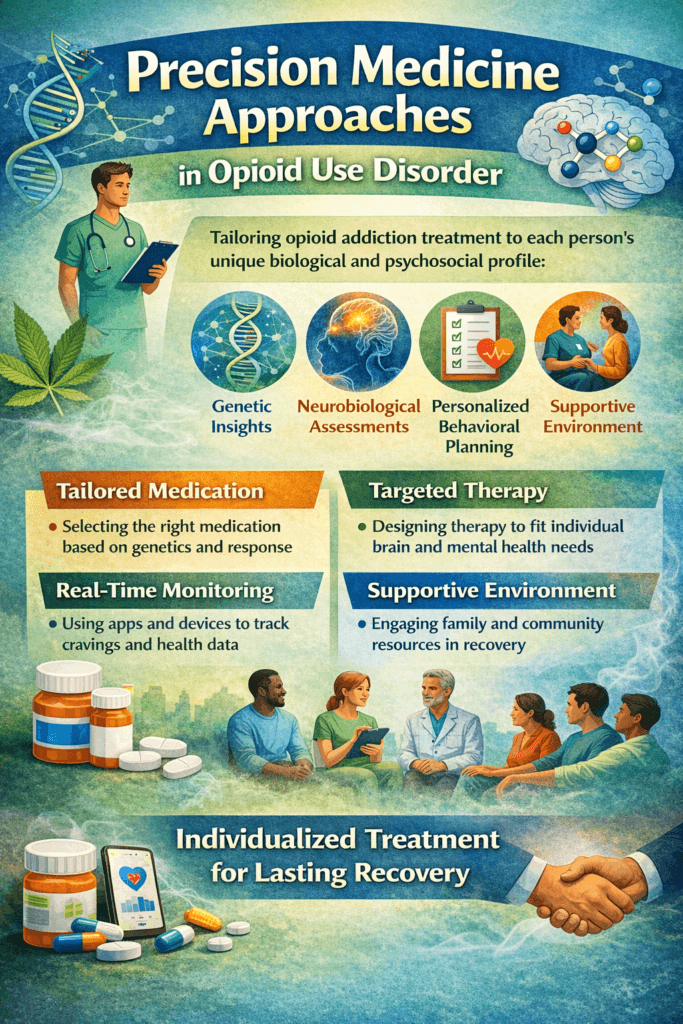
Opioid use disorder (OUD) remains a major public health challenge, with individuals responding differently to the same treatments. Traditional addiction care has often relied on standardized approaches, yet factors such as genetics, brain chemistry, mental health conditions, and life circumstances influence treatment success. Precision medicine offers a new solution by tailoring opioid addiction treatment to each person’s unique biological and psychosocial profile. By leveraging genetic insights, neurobiological assessments, and personalized behavioral planning, precision medicine aims to match individuals with the most effective medications, therapeutic approaches, and support services from the outset.
Precision Medicine Approaches in Opioid Use Disorder: Personalizing Recovery Treatment
Opioid use disorder (OUD) remains one of the most urgent public health crises worldwide. Traditional treatment approaches often rely on standardized medication and therapy plans, yet individuals respond differently to the same interventions. This variability has driven the rise of precision medicine—an approach that tailors treatment to a person’s unique biological, psychological, and environmental factors. In opioid addiction care, precision medicine offers a pathway toward more effective, individualized recovery strategies.
Precision medicine in OUD begins with understanding genetic and biological differences. Variations in genes that affect opioid receptor function or medication metabolism can influence how individuals respond to treatments such as methadone, buprenorphine, or naltrexone. Genetic testing and biomarker analysis may help clinicians determine optimal medication type and dosage, reducing trial-and-error prescribing and improving treatment retention.
Brain imaging and neurocognitive assessments also support personalized care. These tools help identify differences in reward-system sensitivity, impulse control, and stress response, thereby guiding decisions regarding therapy intensity, relapse-prevention strategies, and supportive services. Individuals with co-occurring mental health conditions may benefit from integrated treatment plans designed specifically for dual diagnoses.
Environmental and lifestyle factors are equally important. Precision medicine considers housing stability, family support, trauma history, employment needs, and access to healthcare. By addressing these elements, providers can develop recovery plans that align with real-life circumstances rather than one-size-fits-all programs.
Digital health technologies further enhance personalized care. Mobile apps, wearable monitoring devices, and telehealth platforms allow providers to track cravings, stress levels, medication adherence, and relapse risk in real time. This continuous feedback enables early intervention before setbacks occur.
While precision medicine in OUD is still evolving, it represents a major shift toward patient-centered addiction care. By matching the right treatment to the right person at the right time, recovery becomes more achievable, sustainable, and empowering. As research advances, precision-based approaches will continue to transform how opioid addiction is treated — offering renewed hope for lasting recovery.
Self-Management Strategies in Precision Medicine for Opioid Use Disorder
Opioid use disorder (OUD) is a complex condition that affects the brain, behavior, and overall health. Precision medicine has introduced a new direction in addiction treatment by personalizing care based on an individual’s genetics, brain function, mental health needs, and life circumstances. However, even the most advanced medical plans require active participation from the individual. Self-management strategies help people take ownership of their recovery while benefiting from personalized treatment approaches.
One key self-management strategy is medication adherence. Precision-based treatment may involve medications such as buprenorphine, methadone, or naltrexone, selected specifically for an individual’s biological response. Taking medications exactly as prescribed, using reminders, and attending follow-up appointments ensure the treatment plan remains effective and responsive to changing needs.
Self-monitoring is another important tool. Individuals can track cravings, mood changes, stress levels, sleep patterns, and triggers through journals or mobile recovery apps. This real-time feedback helps healthcare providers adjust treatment plans promptly, thereby preventing relapse.
Lifestyle management supports brain and body healing. Regular sleep routines, balanced nutrition, hydration, and physical activity improve emotional regulation and the effectiveness of medication. Precision medicine recognizes that biological recovery is influenced by daily habits, making healthy routines a powerful part of treatment.
Developing coping skills for stress and emotional regulation is also essential. Personalized therapy plans, such as cognitive-behavioral therapy, mindfulness training, or trauma-informed counseling, help individuals build tools that address their specific psychological needs.
Finally, maintaining engagement with support networks strengthens recovery. Peer groups, telehealth check-ins, and recovery coaching provide accountability and encouragement. Precision medicine is most effective when individuals actively communicate with their providers and participate in shaping their treatment plan.
Self-management transforms precision medicine from a clinical concept into a daily recovery practice. When individuals take consistent, informed action alongside personalized medical care, long-term recovery from opioid use disorder becomes more realistic, stable, and empowering.
Family Support Strategies in Precision Medicine for Opioid Use Disorder
Opioid use disorder (OUD) affects not only the individual but the entire family system. Precision medicine has transformed addiction treatment by tailoring care to a person’s genetic profile, brain function, co-occurring mental health needs, and environmental circumstances. While these personalized medical approaches improve treatment effectiveness, family support remains a critical factor in sustaining long-term recovery.
One essential family strategy is understanding the treatment plan. Precision-based care may involve specific medications, therapeutic approaches, or monitoring tools tailored to an individual’s unique needs. When family members learn how these personalized treatments work, they can provide informed encouragement and reduce fear or misunderstanding about medication-assisted recovery.
Families also play an important role in supporting medication adherence and appointment attendance. Simple actions such as helping maintain routines, offering transportation, or providing reminders reinforce consistency without becoming controlling. Encouragement and positive reinforcement strengthen motivation during periods of adjustment.
Emotional support is equally vital. Precision medicine recognizes that stress sensitivity and emotional regulation differ from person to person. Families that practice active listening, calm communication, and non-judgmental responses help reduce shame and defensiveness, which lowers relapse risk.
Creating a stable home environment further supports personalized recovery plans. Removing substance-related triggers, supporting healthy daily routines, and participating in shared wellness activities promote brain healing and behavioral change. Family involvement in therapy or education sessions also improves understanding of relapse warning signs and crisis response strategies.
Finally, families benefit from respecting boundaries and encouraging independence. Precision medicine is designed to empower individuals to take ownership of their treatment. Supportive families balance guidance with autonomy, fostering confidence and self-efficacy.
When precision medicine and family support work together, recovery becomes a shared process rather than an isolated struggle. Through education, encouragement, and compassionate involvement, families become powerful partners in sustained healing from opioid use disorder.
Community Resource Strategies in Precision Medicine for Opioid Use Disorder
Opioid use disorder (OUD) continues to impact individuals, families, and communities across the nation. Precision medicine has introduced a new era in addiction treatment by personalizing care based on genetic factors, brain function, mental health needs, and environmental conditions. While individualized treatment plans improve clinical outcomes, community resources are crucial for ensuring people can access and sustain these advanced approaches.
One of the most important community strategies is expanding access to precision-based healthcare services. Community health centers, addiction clinics, and integrated behavioral health programs provide screening, genetic testing, medication management, and personalized therapy services. Training healthcare providers in precision addiction medicine ensures that individuals receive accurate assessments and tailored treatment plans.
Peer recovery networks also strengthen personalized care. Community-based support groups, recovery coaching programs, and digital peer platforms offer encouragement, accountability, and shared experience. Connecting with others who understand medication-assisted and precision-based treatment reduces stigma and promotes long-term engagement.
Education and outreach programs further enhance success. Community workshops, public health campaigns, and school-based prevention efforts increase awareness of opioid risks and inform the public about personalized treatment options. Knowledge empowers individuals to seek help early and participate actively in their care decisions.
Practical support services are equally vital. Transportation programs, housing assistance, job training, and legal aid remove barriers that often interfere with treatment participation. Precision medicine is most effective when daily living needs are stable and secure.
Finally, collaboration between medical, mental health, and social service organizations creates integrated care networks. When communities offer coordinated services through a single system, individuals can access personalized medication management, therapy, and social support seamlessly.
Community involvement transforms precision medicine from a specialized clinical model into an accessible recovery pathway. With strong community infrastructure, education, and compassionate care systems, personalized treatment for opioid use disorder becomes achievable, equitable, and sustainable.
Frequently Asked Questions
Here are some common questions:
What is precision medicine in opioid use disorder?
Precision medicine in opioid use disorder is a treatment approach that personalizes care based on an individual’s genetics, brain function, mental health status, and environmental factors. Instead of using a one-size-fits-all method, treatment plans are tailored to match each person’s unique needs.
How is precision medicine different from traditional addiction treatment?
Traditional treatment applies similar medications and therapies to most patients. Precision medicine uses biological testing, clinical assessments, and lifestyle information to determine which medications, therapy approaches, and support services will work best for a specific individual.
What role do genetics play in opioid addiction treatment?
Genetic differences can influence how a person responds to opioids and how their body processes medications like methadone or buprenorphine. Genetic insights may help providers select the right medication and dosage to improve treatment outcomes.
Can precision medicine help prevent relapse?
Yes. By monitoring cravings, stress responses, and behavioral patterns in real time, treatment plans can be adjusted early to prevent relapse. Personalized therapy and medication adjustments improve long-term recovery stability.
Does precision medicine replace medication-assisted treatment?
No. Precision medicine enhances medication-assisted treatment by helping clinicians select the most effective medication for each patient. It works alongside established medications, not instead of them.
Is brain imaging used in precision addiction care?
In some research and specialized clinics, brain imaging and neurocognitive testing are used to assess the function of the reward system, impulse control, and stress sensitivity. These tools guide personalized therapy planning.
What role does mental health play in precision medicine for OUD?
Co-occurring conditions like depression, anxiety, or trauma influence addiction recovery. Precision medicine ensures therapy plans address both opioid addiction and mental health needs together.
Are digital tools part of precision treatment?
Yes. Mobile apps, wearable devices, and telehealth check-ins track cravings, sleep, stress, and medication adherence, allowing providers to adjust care quickly when risk increases.
Is precision medicine widely available?
Precision-based addiction care is growing but not yet available everywhere. Many elements, such as personalized medication planning and integrated care, are already used in modern treatment programs.
Does precision medicine guarantee recovery?
No treatment guarantees recovery, but precision medicine improves the likelihood of success by matching the right interventions to the right person at the right time.
Can families be involved in precision treatment?
Yes. Family education, support planning, and participation in therapy strengthen personalized recovery plans and improve treatment engagement.
Where can someone access precision-based care for opioid use disorder?
Primary care providers, addiction specialists, integrated behavioral health clinics, and research-informed treatment centers are increasingly offering precision-informed services. A healthcare provider can guide appropriate referrals.
Conclusion
Precision medicine is reshaping how opioid use disorder is treated by replacing one-size-fits-all care with individualized recovery strategies. When personalized medication selection, targeted therapy, and real-time health monitoring are combined with self-management, family involvement, and community support, treatment becomes more effective and sustainable. As research and technology continue to advance, precision-based addiction care offers renewed hope for reducing relapse, improving quality of life, and building long-term recovery. With access to personalized treatment and supportive environments, individuals facing opioid use disorder can achieve stronger, more lasting healing.
Video: Precision Medicine for Opioid Use Disorder: Personalized Pathways to Recovery