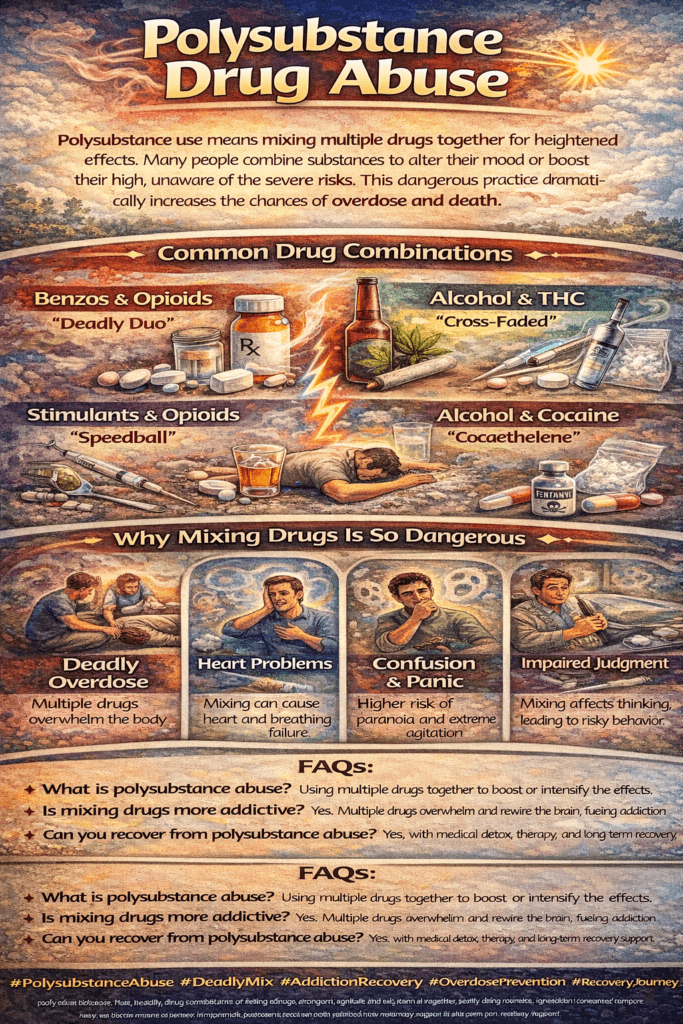
Polysubstance abuse, the usage of multiple drugs, presents complex challenges in addiction treatment. Among the dangerous combinations are opioids and benzodiazepines, which can lead to fatal respiratory depression. Polysubstance users span various demographics, highlighting the need for comprehensive solutions. Treatment options include tailored approaches addressing specific substances through medical detoxification, therapy, and medication-assisted treatment. Understanding polysubstance abuse is crucial for effective intervention and support.
Understanding Polysubstance Abuse: Risks and Treatment Challenges
Polysubstance abuse is a significant public health concern characterized by the concurrent use or misuse of multiple substances, including drugs and alcohol. This complex pattern of substance use poses unique challenges and risks for individuals and healthcare providers alike. In this blog, we will explore the nature of polysubstance abuse, its associated risks, and the complexities of treatment.
What Is Polysubstance Abuse?
Polysubstance abuse occurs when individuals consume various types of drugs—whether illicit drugs, prescription medications, or alcohol—either simultaneously or within a short timeframe. This behavior often arises from the desire to achieve specific effects, intensify the high, or mitigate withdrawal symptoms from one substance with another. For example, a person might combine opioids with alcohol to enhance euphoria or use stimulants to counteract the sedative effects of depressants.
Risks Associated with Polysubstance Abuse
The concurrent use of multiple substances significantly heightens the risk of various adverse health outcomes, including:
- Increased Risk of Overdose: Combining substances can amplify their effects, leading to dangerous respiratory depression, cardiovascular issues, and potentially fatal overdoses. For instance, mixing opioids with alcohol can dangerously depress the central nervous system, increasing the likelihood of overdose.
- Dependency and Addiction: Polysubstance abuse can lead to more complex patterns of dependency, making it challenging for individuals to quit using any one substance. The interplay of multiple substances can exacerbate withdrawal symptoms and cravings, complicating recovery efforts.
- Physical Health Complications: The health risks associated with polysubstance use are multifaceted. Chronic use of various substances can lead to cardiovascular problems, liver damage, respiratory issues, and other severe health conditions.
- Mental Health Issues: Polysubstance abuse is often linked with mental health disorders such as anxiety, depression, and psychosis. The combined effects of different substances can exacerbate these conditions and hinder effective treatment.
Treatment Challenges
Treating polysubstance abuse presents unique challenges for healthcare providers. Some of the critical complexities include:
- Comprehensive Assessment: Effective treatment begins with a thorough assessment of all substances used, their frequency, and the individual’s overall health status. This information is crucial for developing a tailored treatment plan.
- Integrated Treatment Approaches: Addressing polysubstance abuse often requires integrated treatment that simultaneously targets multiple substances. This may involve medication-assisted treatment for opioid use disorder alongside therapy for alcohol dependence, for example.
- Co-occurring Disorders: Many individuals with polysubstance abuse also struggle with co-occurring mental health disorders. Treating both substance use and mental health issues concurrently is essential for successful recovery.
- Individualized Support: Each person’s journey through polysubstance abuse is unique, requiring personalized support that considers their specific needs, preferences, and circumstances. This includes access to counseling, support groups, and community resources.
Strategies for Prevention and Intervention
Preventing and addressing polysubstance abuse involves a multifaceted approach:
- Education and Awareness: Public health campaigns can raise awareness about the dangers of polysubstance abuse, helping individuals understand the risks and encouraging safer practices.
- Access to Treatment Services: Expanding access to comprehensive treatment services is critical. This includes making evidence-based therapies available for individuals struggling with polysubstance abuse.
- Harm Reduction Strategies: Implementing harm reduction programs, such as syringe exchange programs and naloxone distribution, can help mitigate the negative consequences of drug use and save lives.
- Community Support: Fostering supportive environments through community outreach, peer support networks, and recovery resources can empower individuals to seek help and promote long-term recovery.
Polysubstance abuse is a complex and challenging public health issue that requires a comprehensive understanding and targeted interventions. By recognizing the risks associated with concurrent substance use and addressing the unique treatment challenges, healthcare providers and communities can work together to support individuals on their journey to recovery.
Through education, prevention, and compassionate care, we can help reduce the impact of polysubstance abuse and empower individuals to reclaim their lives from addiction. Ultimately, a holistic approach that prioritizes mental and physical health is essential for promoting long-lasting recovery and well-being.
The Dangers of Polysubstance Abuse: Identifying High-Risk Combinations
Identifying the “most dangerous” combinations of drugs in polysubstance abuse can be challenging due to the complexities involved. The risks associated with using multiple substances depend on various factors, including the specific combinations, individual tolerance levels, and overall health. However, certain combinations are widely recognized for their exceptionally high risks and potential for fatal outcomes. This blog will explore some of these dangerous drug pairings and emphasize the importance of seeking help for substance use disorders.
High-Risk Combinations in Polysubstance Abuse
- Opioids and Benzodiazepines:
- Risks: The combination of opioids (such as heroin or prescription painkillers) with benzodiazepines (like Xanax or Valium) is one of the most lethal pairings. Both substances are central nervous system (CNS) depressants, which means they can slow down brain activity and bodily functions. This synergy can lead to severe respiratory depression, increased risk of overdose, and even death.
- Impact: Individuals using both substances often experience compounded effects, including enhanced sedation, impaired motor skills, and heightened potential for accidents.
- Alcohol and Opioids:
- Risks: Mixing alcohol with opioids significantly raises the risk of respiratory depression and overdose. Both substances depress the CNS, which can lead to dangerously low breathing rates and unconsciousness.
- Impact: This combination can impair judgment and coordination, increasing the likelihood of risky behaviors and accidents. It also heightens the potential for fatal overdose, as users may not realize the full extent of the danger they’re in.
- Stimulants and Depressants:
- Risks: The combination of stimulants (such as cocaine or methamphetamine) with depressants (like alcohol or benzodiazepines) presents a unique danger. These substances exert conflicting effects on the body’s systems—stimulants increase heart rate and energy levels, while depressants slow them down.
- Impact: This can lead to cardiovascular complications, including heart attack or stroke, and increase the risk of overdose. Users may not perceive the danger, as the stimulant may mask the depressant’s effects, leading them to consume higher doses of depressants.
- Polydrug Use Involving Multiple Substances:
- Risks: Using various drugs simultaneously—such as opioids, benzodiazepines, stimulants, and alcohol—can result in unpredictable interactions and severe health risks. Each substance can alter how the body metabolizes the others, leading to heightened effects and increased risk of overdose.
- Impact: Medical emergencies can arise from polydrug use, as individuals may experience a range of symptoms that complicate treatment and increase the likelihood of life-threatening situations.
The Importance of Seeking Help
Overall, any combination of substances used in polysubstance abuse can be dangerous and potentially life-threatening. The unpredictability of drug interactions and the cumulative effects of multiple depressants or stimulants underscore the importance of recognizing the risks involved.
Seeking Support and Treatment
For individuals struggling with substance use disorders, seeking help is crucial. Effective interventions can lead to healthier coping strategies, addiction recovery, and improved overall well-being. Here are a few steps to consider:
- Reach Out for Support: Connecting with healthcare professionals, addiction specialists, or support groups can provide individuals with the guidance and resources they need to navigate their recovery journey.
- Educate Yourself: Understanding the risks associated with specific drug combinations can empower individuals to make informed choices about their substance use.
- Consider Treatment Options: Evidence-based treatment approaches, such as medication-assisted treatment, counseling, and peer support programs, can effectively address polysubstance use and facilitate recovery.
Polysubstance abuse presents significant risks, especially with certain combinations of drugs. The potential for overdose, dependence, and other adverse health effects emphasizes the need for awareness and proactive measures. By identifying high-risk combinations and seeking help, individuals can take essential steps toward recovery, ultimately leading to a healthier and more fulfilling life.
Understanding the Demographics of Polysubstance Users: A Multifaceted Approach
Polysubstance drug use is a complex issue that transcends demographic boundaries, encompassing various factors such as age, gender, race/ethnicity, socioeconomic status, and geographic location. Understanding the demographics of polysubstance users is crucial for developing targeted prevention and intervention strategies. This blog will explore the diverse characteristics of individuals who engage in polysubstance use and highlight the need for a comprehensive approach to address this growing concern.
Age: A Spectrum of Use
Polysubstance use is observed across a wide range of age groups, including adolescents, young adults, and older adults. While certain substances are more commonly associated with specific age demographics—such as marijuana and alcohol among younger individuals and prescription drugs among older adults—polysubstance use can occur at any stage of life.
- Adolescents and Young Adults: This group often experiments with substances, leading to combinations of alcohol, marijuana, and illicit drugs.
- Older Adults: As this demographic may rely on prescription medications for chronic conditions, there is a risk of combining these drugs with alcohol or other substances, leading to increased health risks.
Gender: Distinct Patterns of Use
Research suggests that polysubstance use patterns may differ between genders.
- Men: Typically, men are more likely to engage in polysubstance use that involves alcohol and illicit drugs. This may be attributed to social norms that encourage risk-taking behaviors among males.
- Women: Conversely, women may be more inclined to combine prescription medications with other substances, potentially due to factors such as healthcare access, societal pressures, or underlying mental health issues.
Despite these trends, it’s essential to recognize that polysubstance use is not confined to any specific gender; both men and women can exhibit diverse patterns of use.
Race/Ethnicity: Cultural Influences
Polysubstance use occurs among individuals of various racial and ethnic backgrounds. However, disparities may exist regarding substance use prevalence and access to treatment resources.
- Cultural Factors: Social norms and attitudes toward substance use can significantly influence how different racial and ethnic groups engage in polysubstance use.
- Access to Treatment: Systemic barriers may affect certain groups’ access to healthcare and substance use treatment, leading to differences in outcomes and recovery experiences.
Socioeconomic Status: Risk Factors
Polysubstance use spans various socioeconomic strata, but individuals from lower socioeconomic backgrounds may face additional risk factors.
- Economic Instability: Limited access to healthcare, financial stress, and environmental factors contribute to substance use among these populations.
- Healthcare Access: Disparities in healthcare access can lead to a lack of preventive and treatment resources, exacerbating the issue of polysubstance use in lower socioeconomic groups.
Urban vs. Rural Settings: Variations in Use
Polysubstance use is prevalent in urban and rural environments, but the specific substances and use patterns can vary significantly.
- Urban Areas: Illicit drugs may be more common in urban settings, where availability and social factors influence usage patterns.
- Rural Areas: In contrast, opioid use and methamphetamine use are often more prevalent in rural communities, where isolation and limited access to healthcare can intensify substance use issues.
A Comprehensive Approach
Polysubstance use is a multifaceted phenomenon influenced by a myriad of demographic factors. Understanding these demographics is essential for developing effective prevention and intervention strategies tailored to specific populations. Addressing polysubstance use requires a comprehensive approach that considers the intersecting social, economic, and environmental factors contributing to substance use behaviors. By recognizing the diverse demographics of polysubstance users, stakeholders can better allocate resources, enhance treatment accessibility, and ultimately foster healthier communities.
A Comprehensive Guide to Treating Polysubstance Use Disorder
Treating polysubstance use disorder (PSUD) is a complex process that requires a holistic approach, taking into account the unique needs and challenges of individuals struggling with multiple substance dependencies. Successful treatment involves a combination of medical interventions, behavioral therapies, and support services tailored to the individual. Here are some key treatment components for polysubstance users:
1. Detoxification: Safe Management of Withdrawal
Detoxification, or detox, is often the first step in treating PSUD. It involves medically supervised withdrawal management to help individuals safely discontinue substance use while minimizing withdrawal symptoms.
- Medically Supervised Detox: Provides round-the-clock medical support and monitoring to manage withdrawal symptoms and potential complications.
- Symptom Management: Physicians may prescribe medications to alleviate symptoms, making the detox process safer and more comfortable.
2. Medication-Assisted Treatment (MAT): Managing Cravings and Withdrawal
Medication-assisted treatment (MAT) involves using FDA-approved medications to reduce cravings and withdrawal symptoms, which can be especially beneficial for individuals with opioid or alcohol dependence.
- Common Medications Used:
- Methadone: An opioid agonist that reduces cravings and withdrawal symptoms.
- Buprenorphine: A partial opioid agonist that helps manage withdrawal while reducing the risk of misuse.
- Naltrexone: An opioid antagonist that blocks the euphoric effects of opioids and alcohol, reducing the urge to use.
- Benefits of MAT: MAT can improve treatment retention, reduce substance use, and lower the risk of overdose.
3. Behavioral Therapies: Addressing Underlying Issues
Behavioral therapies play a critical role in treating PSUD by addressing the psychological and behavioral aspects of addiction. They help individuals develop coping skills, identify triggers, and change unhealthy thought patterns.
- Cognitive-behavioral therapy (CBT): Teaches individuals how to manage cravings and avoid relapse by changing negative thinking patterns.
- Motivational Interviewing: Enhances the individual’s motivation to change by exploring ambivalence toward recovery.
- Contingency Management: Uses positive reinforcement to encourage sobriety and offers incentives for meeting treatment goals.
- Relapse Prevention Techniques: Focuses on identifying and avoiding high-risk situations that could trigger substance use.
4. Support Groups: Building a Network of Peer Support
Participation in support groups provides an essential social support network that promotes recovery through shared experiences, encouragement, and accountability.
- 12-Step Programs: Groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) offer peer-led support and a structured recovery framework.
- Non-12-Step Alternatives: Groups such as SMART Recovery focus on self-empowerment and cognitive-behavioral techniques rather than spiritual principles.
5. Integrated Treatment Programs: Addressing Co-Occurring Disorders
Many individuals with PSUD also suffer from co-occurring mental health disorders, such as anxiety, depression, or PTSD. Integrated treatment programs address both substance use and mental health issues concurrently, providing comprehensive care.
- Medical, Psychiatric, and Behavioral Services: These programs offer a combination of medical management, therapy, and social support to address the full spectrum of the individual’s needs.
6. Holistic Therapies: Complementing Traditional Treatment
Holistic approaches can enhance traditional treatment modalities by addressing overall well-being and providing additional coping strategies.
- Mindfulness Practices: Meditation and yoga promote relaxation and stress reduction.
- Acupuncture: May help alleviate withdrawal symptoms and reduce cravings.
- Art Therapy: Allows individuals to express emotions and experiences creatively, facilitating emotional healing.
7. Aftercare Planning: Maintaining Long-Term Recovery
A comprehensive aftercare plan is vital for sustaining recovery after initial treatment. This plan may involve ongoing therapy, medication management, support groups, and access to community resources.
- Ongoing Therapy: Continued individual or group therapy can help individuals navigate the challenges of maintaining sobriety.
- Medication Management: Monitoring and adjusting MAT as needed to support recovery.
- Community Resources: Linking individuals to sober living arrangements, vocational training, or educational opportunities.
8. Family Involvement: Strengthening Support Systems
Family involvement can significantly enhance the recovery process. Engaging family members in treatment helps build a supportive home environment and improves communication.
- Family Therapy: Addresses family dynamics, improves communication, and helps repair strained relationships.
- Education Programs: Teach family members about addiction, recovery, and ways to support their loved one’s sobriety.
Conclusion: A Multidisciplinary Approach to Treating PSUD
Polysubstance use disorder is a multifaceted condition that requires a personalized and multidisciplinary approach to treatment. The most effective interventions address the biological, psychological, and social factors influencing substance use. Successful treatment often involves collaboration between healthcare providers, therapists, support groups, and other stakeholders to provide comprehensive care and support for individuals struggling with PSUD.
By understanding the complexities of polysubstance use and implementing an integrated approach, individuals can achieve lasting recovery and improve their quality of life.
Frequently Asked Questions
Here are some common questions:
Q: What is polysubstance drug abuse?
A: Using more than one drug at the same time or within the same period.
Q: Why do people mix substances?
A: To intensify effects, reduce withdrawal, or cope with emotional or mental health issues.
Q: Why is polysubstance use so dangerous?
A: Drugs interact unpredictably, increasing the risk of overdose and organ failure.
Q: Can someone overdose without realizing it?
A: Yes. One drug may mask the effects of another, delaying awareness of danger.
Q: Is treatment different for polysubstance addiction?
A: Yes. Treatment must address all substances and underlying mental health needs.
Q: Can recovery from polysubstance abuse be successful?
A: Absolutely. Comprehensive medical care, therapy, and long-term support are effective.
Conclusion
Polysubstance abuse represents a multifaceted issue within addiction treatment, with certain combinations posing significant risks, such as opioids and benzodiazepines. This pattern of substance use is not limited to any particular demographic, highlighting the need for comprehensive and adaptable interventions. Treatment options, including medical detoxification, therapy, and medication-assisted treatment, must be tailored to address the specific substances involved. By understanding the complexities of polysubstance abuse and implementing targeted interventions, we can better support individuals struggling with this challenging form of addiction and work towards improved outcomes and recovery.
Video: When Two Drugs Mix Your Body Shuts Down #polysubstance #realstory #shorts