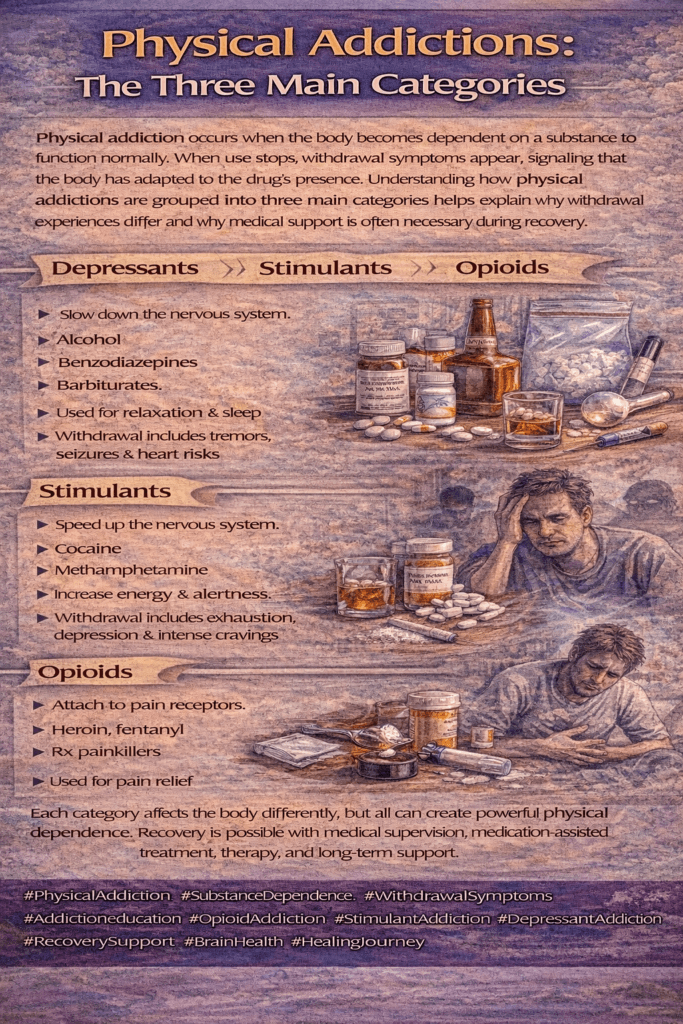
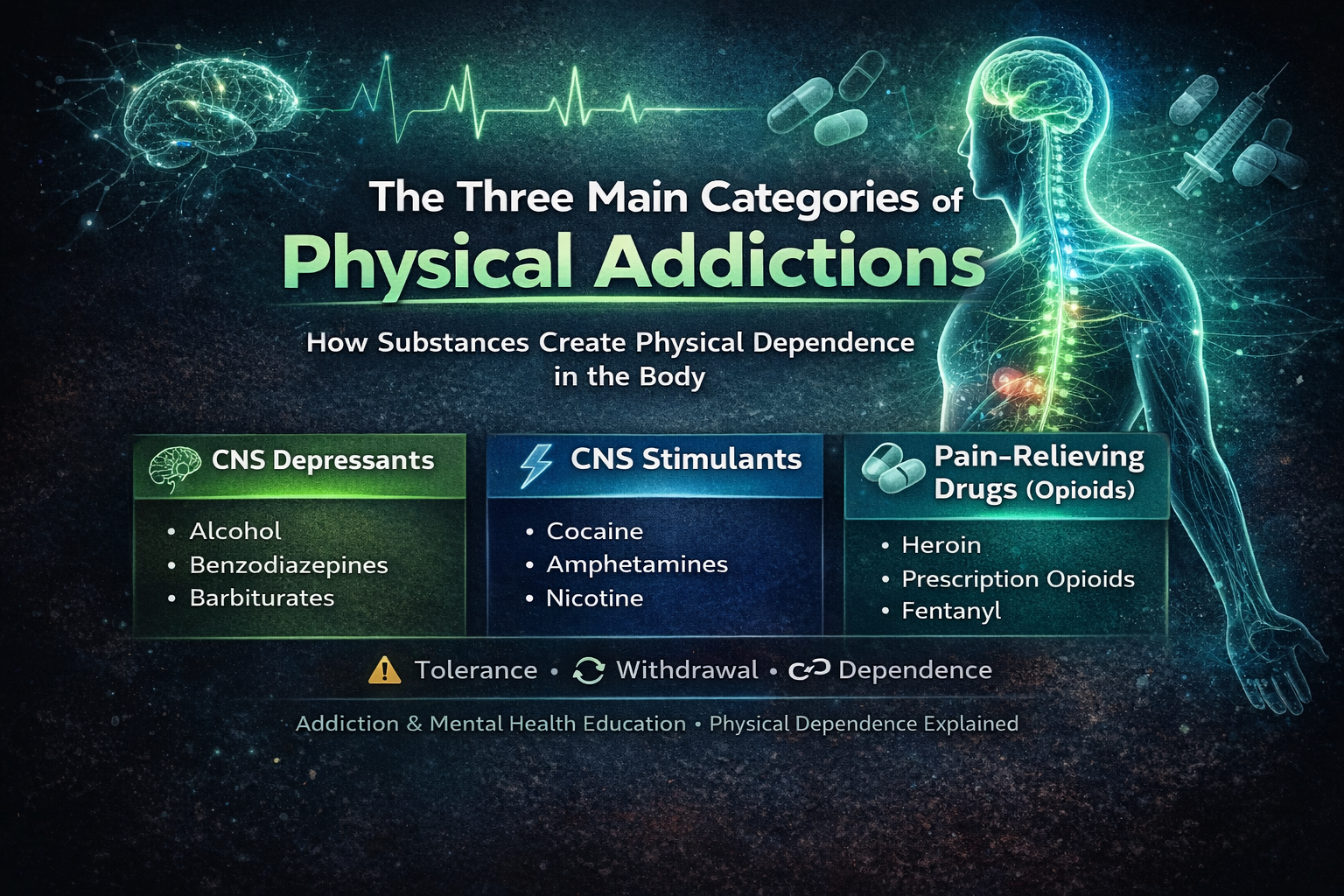
Physical addiction occurs when the body adapts to repeated substance use and becomes dependent on that substance to maintain normal functioning. This process is driven by changes in brain chemistry and physiological regulation, leading to tolerance, withdrawal symptoms, and cravings when use is reduced or stopped. Most physical addictions fall into three main categories—depressants, stimulants, and fast-acting substances such as nicotine—each affecting the body in distinct ways but sharing common biological mechanisms of dependence. Understanding these categories helps clarify why physical addiction is a medical condition rather than a failure of self-control.
The Three Main Categories of Physical Addictions
Physical addiction refers to a state in which the body adapts to the repeated presence of a substance and becomes dependent on it to function normally. When use is reduced or stopped, the body reacts with withdrawal symptoms, signaling that physiological dependence has developed. While many substances can be addictive, most physical addictions fall into three main categories, based on how they affect the brain and body.
The first category is depressants, which slow down the central nervous system. This group includes substances such as alcohol, opioids, and sedatives. Depressants reduce pain, anxiety, and stress by suppressing brain activity, but with repeated use, the body compensates by increasing excitatory responses. Over time, tolerance develops, requiring higher doses to achieve the same effect. Withdrawal from depressants can be physically severe and, in some cases, life-threatening, involving symptoms such as tremors, seizures, nausea, and cardiovascular instability.
The second category is stimulants, which increase activity in the central nervous system. Drugs in this category include cocaine, methamphetamine, and certain prescription stimulants when misused. Stimulants elevate dopamine and adrenaline levels, producing heightened energy, alertness, and euphoria. Physical addiction to stimulants often involves strong cravings, fatigue, sleep disturbances, and changes in appetite. While stimulant withdrawal may be less medically dangerous than depressant withdrawal, it can still cause significant physical and psychological distress that reinforces continued use.
The third category is nicotine and similar fast-acting substances, which rapidly alter brain chemistry and create strong physical dependence despite often subtle intoxication effects. Nicotine acts quickly on reward pathways, conditioning the body to frequent dosing throughout the day. Withdrawal symptoms—such as irritability, headaches, restlessness, and concentration problems—can begin within hours, making cessation challenging even though nicotine does not produce dramatic intoxication.
Understanding these three categories helps clarify why physical addiction is not about willpower, but about biological adaptation. Each category affects the body differently, yet all involve tolerance, dependence, and withdrawal. Recognizing how physical addiction develops is essential for effective treatment planning, medical support during withdrawal, and compassionate approaches to recovery.
Self-Management Strategies to Avoid the Three Main Categories of Physical Addictions
Physical addiction develops when the body adapts to repeated substance use and begins to rely on that substance to maintain balance. The three main categories of physical addiction—depressants, stimulants, and fast-acting substances such as nicotine—affect the body in different ways, but all involve tolerance, dependence, and withdrawal. Self-management strategies help individuals reduce risk, recognize early warning signs, and protect their physical and mental health.
One essential strategy is building awareness of how substances affect the body. Understanding that depressants slow the nervous system, stimulants overstimulate it, and nicotine rapidly conditions the brain to frequent dosing helps individuals recognize when use is becoming physiological rather than situational. Awareness makes it easier to notice increasing tolerance, cravings, or withdrawal symptoms.
Setting clear personal boundaries around substance use is another powerful self-management tool. This may include limiting frequency, avoiding mixing substances, refusing non-medical use of prescriptions, or choosing substance-free routines. Boundaries reduce impulsive behavior and prevent gradual escalation into physical dependence.
Effective stress management is critical across all categories of physical addiction. Chronic stress increases vulnerability to both depressants and stimulants, while nicotine is often used to regulate mood and focus. Healthy alternatives such as exercise, mindfulness, structured daily routines, adequate sleep, and relaxation techniques reduce reliance on substances to regulate physiological or emotional needs.
Monitoring early physical warning signs supports prevention. These signs may include the need for larger doses to experience effects, headaches, shakiness, fatigue, sleep disruption, or irritability when not using. Responding early—by reducing use and seeking guidance—can prevent deeper physical dependence.
Finally, seeking medical and professional support early is a key self-management strategy. Healthcare providers can help assess risk, manage withdrawal safely, and offer guidance tailored to each substance category. Early intervention is especially important for depressants, where unsupervised withdrawal can be dangerous.
Self-management is about proactive care rather than control. By increasing awareness, setting boundaries, managing stress, monitoring physical changes, and seeking help early, individuals can reduce the risk of physical addiction across all three major categories and support long-term health and recovery.
Family Support Strategies to Avoid the Three Main Categories of Physical Addictions
Physical addiction can develop when the body becomes dependent on substances that alter normal physiological functioning. The three main categories—depressants, stimulants, and fast-acting substances such as nicotine—affect the body differently, but all can lead to tolerance, withdrawal, and long-term health consequences. Families play a powerful protective role in helping prevent these patterns from taking hold.
A cornerstone of family prevention is open, consistent communication. Families that talk honestly about how substances affect the body—without fear, blame, or shame—create safe spaces for questions and early disclosure. Clear discussions about risks associated with alcohol, opioids, stimulants, and nicotine help family members make informed choices before dependence develops.
Modeling healthy coping behaviors is equally important. Family members, especially children and adolescents, learn how to manage stress, pain, and emotions by observation. When families demonstrate healthy strategies—such as exercise, emotional expression, problem-solving, and seeking help—substances are less likely to become tools for regulation or escape.
Establishing clear expectations and boundaries around substance use provides structure and protection. This may include rules about prescription medication use, limits on alcohol exposure, or shared values regarding nicotine and stimulant use. Boundaries work best when they are consistent, clearly explained, and paired with emotional support rather than punishment.
Emotional connection and support act as strong protective factors against physical addiction. Feeling valued, heard, and supported reduces the likelihood that substances will be used to cope with loneliness, stress, or pressure. Regular family time, active listening, and validation of feelings strengthen resilience across all ages.
Finally, families should prioritize early recognition and support-seeking. Physical addiction often develops gradually, with subtle signs such as increased tolerance, irritability, sleep changes, or reliance on substances for daily functioning. Addressing concerns early and involving healthcare providers when needed can prevent progression and reduce harm—especially with substances where withdrawal may be medically risky.
Family support strategies are not about control; they are about connection, guidance, and early action. By fostering communication, modeling healthy behaviors, setting clear boundaries, strengthening emotional bonds, and seeking help early, families can significantly reduce the risk of physical addiction across all three major categories and promote long-term health and stability.
Community Resource Strategies to Avoid the Three Main Categories of Physical Addictions
Physical addiction develops when repeated substance use causes the body to adapt and rely on that substance to function normally. The three main categories—depressants, stimulants, and fast-acting substances such as nicotine—can all lead to tolerance, withdrawal, and serious health risks. Community resources play a critical role in prevention by shaping environments, access to care, and early intervention systems that protect individuals and families.
A foundational strategy is community education and prevention outreach. Schools, workplaces, faith-based organizations, and public health departments can provide accurate, science-based information about how different substances affect the body and why physical dependence develops. Education that emphasizes health and safety—rather than fear or punishment—helps people recognize early warning signs and seek help sooner.
Accessible healthcare and screening services are essential. Community clinics, primary care practices, and public health programs can offer early screening, brief interventions, and referrals for substance-related concerns. Easy access to medical guidance is especially important for depressants, where unsupervised withdrawal can be dangerous, and for stimulants and nicotine, where early support can prevent escalation.
Communities also reduce risk by offering recovery-oriented and support services. Peer-support groups, counseling programs, smoking-cessation resources, and outpatient treatment options provide practical tools for reducing or avoiding substance use. When these services are affordable, local, and culturally responsive, people are more likely to engage before physical addiction becomes severe.
Environmental and policy strategies further strengthen prevention. Responsible prescribing practices, prescription drug monitoring programs, safe medication disposal sites, smoke-free public spaces, and workplace wellness initiatives all reduce exposure and normalize healthier choices. These strategies protect the broader population while supporting individuals at higher risk.
Finally, strong community connection and engagement act as powerful protective factors. Recreational programs, volunteer opportunities, recovery-friendly workplaces, and social-support networks reduce isolation and stress—two major drivers of physical addiction across all categories. Communities that foster belonging and purpose make it easier for individuals to cope without relying on substances.
Preventing physical addiction is a shared responsibility. By investing in education, accessible healthcare, supportive services, protective policies, and connected communities, society can reduce the risk of physical dependence across all three major categories and promote long-term health, stability, and recovery.
Frequently Asked Questions
Here are some common questions:
What is physical addiction?
Physical addiction occurs when the body adapts to repeated substance use and becomes dependent on that substance to function normally. When use stops or decreases, withdrawal symptoms appear, indicating physiological dependence.
What are the three main categories of physical addiction?
The three main categories are depressants, stimulants, and fast-acting substances such as nicotine. These categories are based on how substances affect the central nervous system and bodily functions.
What substances fall under depressants?
Depressants include alcohol, opioids (such as heroin and prescription pain medications), benzodiazepines, and some sedatives. These substances slow brain activity and bodily functions and often produce dangerous withdrawal symptoms.
Why are depressant withdrawals considered dangerous?
Withdrawal from depressants can be life-threatening because the nervous system rebounds into overactivity. Symptoms may include seizures, severe anxiety, heart complications, and delirium, often requiring medical supervision.
What substances are classified as stimulants?
Stimulants include cocaine, methamphetamine, and prescription stimulants when misused. These substances increase brain activity, heart rate, and alertness, leading to strong cravings and physical exhaustion during withdrawal.
Does stimulant addiction involve physical dependence?
Yes. While stimulant withdrawal may not always be medically dangerous, it involves physical symptoms such as fatigue, sleep disruption, appetite changes, and intense cravings that reinforce continued use.
Why is nicotine considered a major physical addiction?
Nicotine is fast-acting and rapidly conditions the brain to frequent dosing. Withdrawal symptoms—such as irritability, headaches, restlessness, and difficulty concentrating—can begin within hours of stopping use.
Can someone be physically addicted without being psychologically addicted?
Physical and psychological addiction often overlap, but they are not identical. Physical addiction involves bodily dependence and withdrawal, while psychological addiction focuses on cravings, habits, and emotional reliance.
How does tolerance relate to physical addiction?
Tolerance occurs when the body adapts to a substance, requiring higher doses to achieve the same effect. It is a key sign that physical dependence is developing across all three categories.
How can physical addiction be prevented or addressed early?
Early prevention includes education, setting limits, managing stress without substances, recognizing early physical warning signs, and seeking medical or professional support before dependence becomes severe.
Is physical addiction a sign of weak willpower?
No. Physical addiction is a biological process caused by changes in brain chemistry and body regulation. It is a medical condition that benefits from compassionate, evidence-based treatment.
Conclusion
Recognizing the three main categories of physical addictions provides a clearer framework for prevention, early intervention, and treatment. While depressants, stimulants, and nicotine-based substances impact the body differently, all can disrupt normal functioning and lead to serious health consequences if left unaddressed. Effective responses require awareness, supportive environments, and access to medical and behavioral care. By approaching physical addiction through education, compassion, and coordinated support, individuals, families, and communities can reduce risk and promote long-term health and recovery.
Video: Physical Addictions- The Three Main Categories