Using oxytocin as an adjunctive treatment for pain management in addiction recovery offers potential benefits, including pain relief, reduced cravings, and enhanced emotional well-being. However, challenges such as response variability, side effects, and ethical dilemmas related to informed consent and dependency must be addressed. Community resource strategies, including education campaigns, access to alternative therapies, and support networks, are vital for maximizing oxytocin’s effectiveness. By navigating these considerations, healthcare providers can integrate oxytocin into comprehensive treatment plans, promoting better outcomes for individuals facing both addiction and chronic pain.
Exploring the Role of Oxytocin in Addiction Recovery and Pain Management
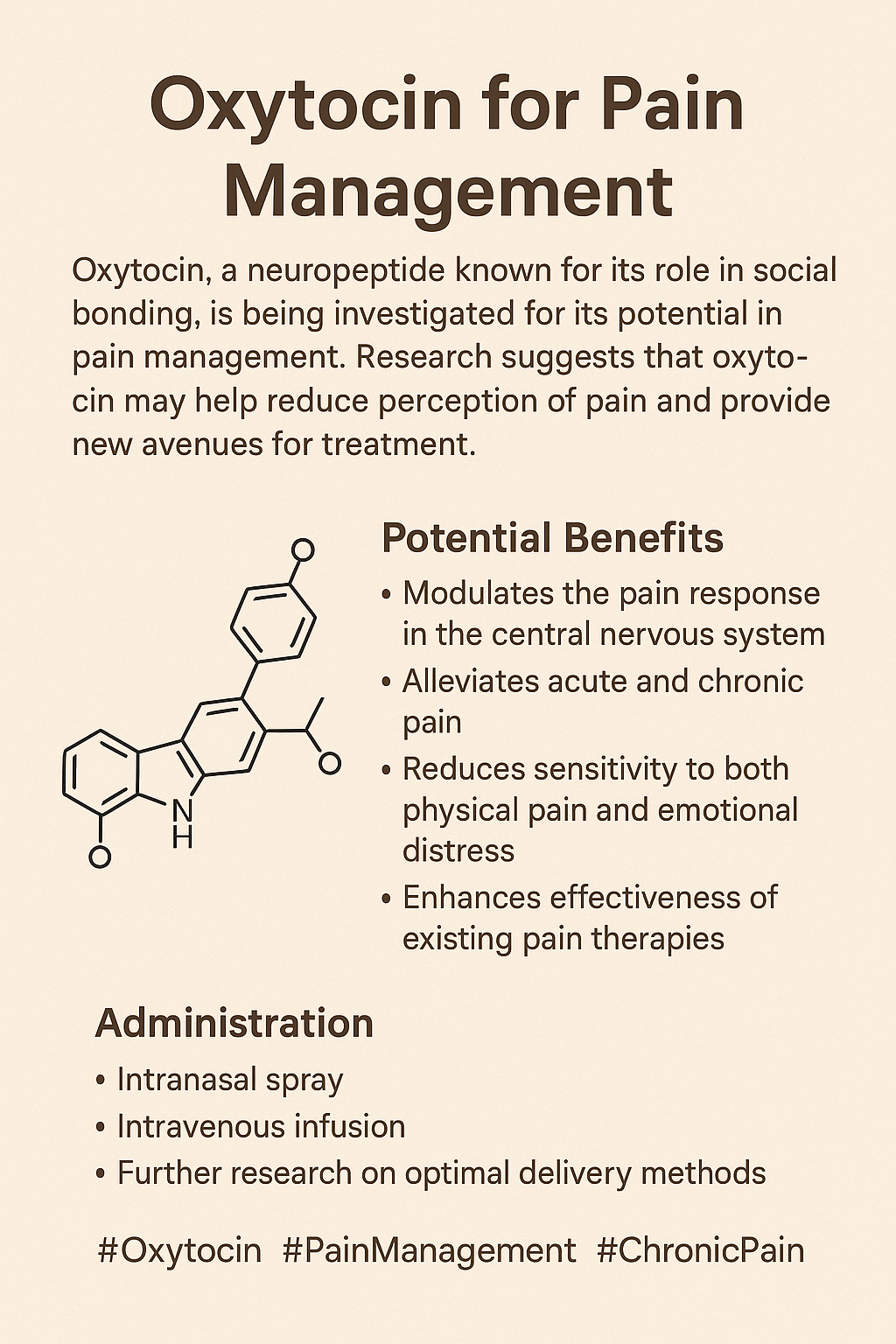
Oxytocin, commonly known as the “love hormone,” has attracted growing interest as a potential adjunctive therapy in addiction treatment, especially for managing pain. Known for its role in social bonding and emotional regulation, oxytocin’s multifaceted effects could offer a unique approach to addiction recovery by addressing pain, cravings, and social connection. Here are some of the critical functions of oxytocin in the context of addiction and pain management:
1. Pain Modulation
- Analgesic Effects: Oxytocin has been shown to possess analgesic, or pain-relieving, properties that can help reduce pain perception. This can be particularly beneficial for individuals in addiction recovery who may experience chronic pain or withdrawal-induced discomfort, making it easier to navigate recovery without resorting to addictive substances.
2. Reducing Cravings and Withdrawal Symptoms
- Craving Reduction: Some studies suggest that oxytocin may help reduce cravings for substances such as opioids or alcohol, potentially easing the withdrawal process and improving treatment outcomes.
- Anxiety and Stress Reduction: Oxytocin’s calming effects may help manage anxiety and stress, common triggers for substance use. By promoting a sense of calm and safety, oxytocin could make it easier for individuals to resist cravings.
3. Enhancing Social Connections
- Social Support: Oxytocin plays a crucial role in social bonding, which can be especially valuable in addiction recovery. A strong support network is vital for sustained recovery, and oxytocin’s effects on social bonding may help individuals feel more connected to their recovery community.
4. Improving Emotional Regulation
- Emotional Stability: Oxytocin influences emotional responses and helps with emotional regulation, potentially assisting individuals in managing the emotional challenges of addiction and recovery. Enhanced emotional stability can reduce the risk of relapse and improve overall well-being.
5. Potential for Reduced Opioid Use
- Opioid-Sparing Effect: Given its pain-relieving properties, oxytocin might reduce the need for opioid medications in pain management, which could lower the risk of opioid dependence or misuse in individuals with chronic pain.
6. Neurochemical Interactions
- Dopaminergic Pathways: Oxytocin interacts with the brain’s dopamine pathways, which play a central role in addiction. By modulating dopamine release, oxytocin may alter reward sensitivity and help break the addiction cycle by reducing the reliance on addictive substances for reward and pleasure.
7. Research and Future Directions
- While the potential benefits of oxytocin as an adjunctive therapy in pain management and addiction treatment are promising, further research is needed to understand its complete mechanisms, optimal dosing, and long-term effects. Clinical trials will be essential to determine the effectiveness and safety of oxytocin in these contexts.
Oxytocin holds promise as an adjunctive treatment in addiction recovery, offering both pain relief and support for the emotional and social aspects of recovery. By addressing pain, reducing cravings, and enhancing social bonding, oxytocin could serve as a holistic tool in addiction treatment, potentially transforming the recovery journey for many individuals.
Potential Disadvantages of Oxytocin in Addiction Treatment and Pain Management
Oxytocin, often called the “love hormone,” has shown potential as an adjunctive therapy in pain management and addiction recovery. However, several significant limitations and potential disadvantages exist when exploring its therapeutic use. Here’s a look at some of the challenges associated with oxytocin in this context:
1. Limited Research
- Insufficient Evidence: While early studies suggest promising effects, the current evidence on oxytocin’s effectiveness and safety in addiction treatment is limited. The lack of large-scale clinical trials makes establishing oxytocin as a widely accepted treatment difficult.
2. Variability in Response
- Individual Differences: Responses to oxytocin can vary due to genetic, physiological, and psychological factors. This variability can make it challenging to use oxytocin as a standardized treatment, as effects might differ significantly from one person to another.
3. Potential Side Effects
- Adverse Reactions: Oxytocin may cause side effects such as nausea, headache, and, in some cases, allergic reactions. For some individuals, it could also lead to increased anxiety or mood shifts, which could be counterproductive in addiction recovery.
4. Short Duration of Action
- Transient Effects: The analgesic effects of oxytocin are often short-lived and might require repeated dosing. This need for frequent administration could complicate treatment plans, especially for individuals dealing with chronic pain.
5. Impact on Hormonal Balance
- Hormonal Effects: Oxytocin interacts with other hormones and neuropeptides, potentially causing hormonal imbalances. This could have unintended health consequences, requiring careful monitoring.
6. Dependency Concerns
- Psychological Dependence: Although oxytocin itself is not addictive, there is a potential for psychological reliance. Individuals may become dependent on its calming effects, leading to an over-reliance on oxytocin for emotional regulation, which could complicate long-term recovery.
7. Cost and Accessibility
- Economic Barriers: The cost of oxytocin treatment, combined with limited insurance coverage, may create access issues for patients, particularly for those already experiencing financial hardship due to addiction or chronic pain.
8. Stigma and Misunderstanding
- Public Perception: There may be a stigma or lack of understanding around using hormones in addiction treatment. Patients may feel uncomfortable with this approach or worry about public perceptions, which can affect their willingness to pursue such therapy.
9. Regulatory Issues
- Approval and Regulation: Since oxytocin is not explicitly approved for pain management or addiction treatment, its use could lead to legal and regulatory complications in clinical settings, adding ethical and logistical hurdles.
10. Complexity of Pain Management
- Multi-Factorial Nature of Pain: Pain management, especially in individuals with addiction, is complex, involving physical, psychological, and social factors. Oxytocin alone may not address these multiple facets, and relying solely on it may oversimplify the treatment of chronic pain and addiction.
While oxytocin presents exciting possibilities as an adjunctive therapy in pain and addiction recovery, the disadvantages and limitations—such as limited research, potential side effects, and complex treatment requirements—must be carefully weighed. A thorough assessment and a holistic treatment approach are essential before integrating oxytocin into clinical practice.
Ethical Considerations in Using Oxytocin for Pain Management in Addiction Recovery
Oxytocin, known for its role in social bonding, has gained interest as a potential adjunctive treatment in pain management for those in addiction recovery. However, while this treatment holds promise, it also raises several ethical dilemmas that healthcare providers must navigate. Here are some of the primary ethical concerns surrounding oxytocin use in this context:
1. Informed Consent
- Understanding Risks and Benefits: Given the limited research on oxytocin’s efficacy for pain management in addiction recovery, patients must understand the potential risks and benefits. Providers must ensure patients are aware of the experimental nature of this approach, which can be challenging given limited data.
2. Patient Autonomy vs. Provider Recommendations
- Respecting Choices: Patients may have varying opinions about using hormonal treatments. Providers must balance respect for the patient’s autonomy with their professional recommendations on the suitability of oxytocin in their treatment plan, striving for shared decision-making.
3. Withdrawal Management
- Ethical Responsibility: Using oxytocin to help manage withdrawal symptoms during a vulnerable period in recovery must be ethically justified. Providers must consider whether the benefits outweigh the potential risks and if introducing a new substance could complicate recovery.
4. Equity of Access
- Resource Allocation: The cost and accessibility of oxytocin treatments may limit access for some patients, particularly those with fewer financial resources. Ethical questions arise about whether all patients have equal opportunities to benefit from this treatment regardless of socioeconomic status.
5. Dependency and Misuse
- Potential for Psychological Dependency: Although oxytocin does not carry the traditional risks of addiction, there is potential for psychological dependence on its calming effects. Providers should weigh the ethical implications of introducing a treatment that could become a crutch rather than a stepping-stone toward independence.
6. Impact on Treatment Goals
- Long-Term Outcomes: Introducing oxytocin should align with the broader goal of sustained recovery. Providers must consider whether its use genuinely contributes to long-term recovery or merely alleviates symptoms without addressing underlying addiction issues.
7. Variability in Response
- Individual Differences: People respond differently to oxytocin, complicating treatment. Providers face ethical dilemmas when personalizing treatments for individuals, especially if some patients experience adverse effects or derive no benefit, potentially impacting the patient-provider trust.
8. Research and Evidence Base
- Utilizing Emerging Treatments: Oxytocin’s use in pain management lacks robust clinical evidence, raising ethical concerns about whether it is appropriate to use treatments still considered emerging, even if they hold potential.
9. Regulatory and Approval Issues
- Compliance with Guidelines: Oxytocin is not formally approved for pain management or addiction treatment, which complicates its use in clinical practice. Providers must consider whether using an off-label treatment is ethically appropriate without specific regulatory approval.
10. Balancing Pain and Recovery Needs
- Compassionate Care: Providers face the ethical challenge of managing pain adequately without reinforcing addictive tendencies. Striking this balance is critical to ensuring that pain management approaches support sustainable recovery.
The ethical dilemmas surrounding oxytocin use in addiction treatment centers involve informed consent, patient autonomy, equity of access, and the need for evidence-based care. Providers need to engage in transparent communication, carefully assess each patient’s unique needs, and consider both the short—and long-term implications to uphold ethical standards in clinical practice.
Building Community Resource Strategies for Oxytocin as a Pain Management Aid in Addiction Recovery
As oxytocin gains attention as a potential adjunctive treatment for pain management in addiction recovery, establishing community resource strategies is essential for supporting patients, healthcare providers, and families. Here are some critical community-based strategies to provide comprehensive support, education, and access for individuals considering oxytocin as part of their treatment.
1. Education and Awareness Campaigns
- Community Workshops: Organize workshops to educate healthcare providers and patients about oxytocin’s potential benefits and risks in pain management and addiction treatment. These sessions can foster an informed understanding and help address common questions.
- Informational Materials: Distribute pamphlets, brochures, and online resources explaining oxytocin’s role, effects, and alternatives to ensure that patients and families have access to transparent, accurate information.
2. Access to Healthcare Providers
- Training Programs for Providers: Develop training modules for healthcare professionals to cover oxytocin’s appropriate use, including dosing protocols, monitoring requirements, and patient suitability considerations.
- Interdisciplinary Teams: Foster collaboration between doctors, pharmacists, and psychologists to create individualized, comprehensive care plans, ensuring a holistic approach to oxytocin-supported recovery.
3. Support Groups and Peer Counseling
- Peer Support Networks: Establish local or online support groups where individuals can share their experiences, challenges, and successes with others in similar situations, offering mutual support through the treatment journey.
- Peer Navigators: Train individuals in recovery to act as peer navigators, providing emotional support and practical advice to those considering or actively using oxytocin in their recovery plans.
4. Access to Alternative Therapies
- Complementary Treatment Options: Provide resources on additional pain management strategies, such as physical therapy, acupuncture, and mindfulness, that can complement oxytocin’s effects for a more balanced approach.
- Integrative Health Programs: Establish programs combining oxytocin with non-pharmacological therapies, addressing both pain management and addiction support in an integrative model.
5. Monitoring and Follow-Up Services
- Routine Follow-Up Appointments: Encourage consistent follow-ups to assess patients’ responses to oxytocin, manage side effects, and adjust treatment as needed.
- Data Collection and Evaluation: Implement a system to track patient outcomes. This will help inform future practices and contribute to a stronger evidence base for oxytocin’s role in addiction recovery.
6. Crisis Intervention Resources
- Emergency Support Services: Establish crisis intervention services to provide immediate assistance for patients experiencing severe pain or withdrawal symptoms and ensure timely support when needed.
- 24/7 Helplines: Provide round-the-clock helplines for patients to access guidance related to oxytocin treatment and connect them with qualified professionals for immediate support.
7. Research and Development Initiatives
- Collaborations with Research Institutions: Partner with academic institutions to advance research on oxytocin’s effectiveness in pain and addiction, contributing to the growing body of evidence.
- Clinical Trials: Facilitate patient participation in clinical trials, offering additional resources and insights while expanding understanding of oxytocin’s potential benefits and limitations.
8. Policy Advocacy
- Advocacy for Funding: Work with local governments to secure funding for community-based programs supporting oxytocin use, ensuring equitable access for patients regardless of financial circumstances.
- Support for Regulations: Advocate for policies promoting the safe and ethical use of oxytocin in clinical settings, including monitoring and follow-up care guidelines.
9. Online Resources and Telehealth
- Telehealth Services: Provide telehealth options for consultations and follow-ups, making it easier for patients to access support and guidance without frequent in-person visits.
- Educational Websites: Develop online platforms with information, videos, and discussion forums for patients and families to learn about oxytocin and share insights or experiences.
10. Community Partnerships
- Collaboration with Nonprofits: Partner with nonprofit organizations focused on addiction recovery and pain management to provide a network of resources, support groups, and educational materials.
- Engagement with Local Health Departments: Integrate oxytocin education and resources into community health initiatives, working alongside local health departments to broaden access to support.
By implementing these strategies, communities can build a supportive environment for patients using oxytocin in pain management and addiction recovery. These resources enhance awareness, improve access to complementary therapies, and ensure patients receive the comprehensive care they need to pursue sustainable recovery.
Conclusion
Using oxytocin for pain management as an adjunctive treatment in addiction recovery presents both significant benefits and notable challenges. Its potential to alleviate pain, reduce cravings, and improve emotional well-being makes it a promising option. However, concerns about individual variability, side effects, and ethical dilemmas surrounding informed consent and dependency highlight the complexities of its use. To effectively integrate oxytocin into treatment plans, community resource strategies—such as education, access to alternative therapies, and support networks—are essential. By addressing these factors, healthcare providers can enhance the overall effectiveness of addiction treatment, ultimately leading to better outcomes for individuals grappling with chronic pain and substance use disorders.
Video: 5 Things You Need to Know About Oxytocin’s Role in PAIN MANAGEMENT