The introduction of overdose reversal medications, such as naloxone, marks a critical advancement in addressing the alarming rise of opioid overdoses. These medications are designed to rapidly reverse the life-threatening effects of opioid intoxication, providing a crucial lifeline during emergencies. The purpose is clear: to save lives and buy valuable time for individuals in the throes of overdose. However, despite their effectiveness, challenges exist in ensuring widespread accessibility and utilization. This essay explores the multifaceted landscape of overdose reversal medications, delving into their purposes and uses, the hurdles encountered in their distribution and adoption, and the pivotal roles of family support and community resources in maximizing their impact. As we navigate this complex terrain, it becomes evident that the success of overdose reversal efforts hinges not only on the availability of these medications but also on the collaborative and supportive networks that communities and families can cultivate to address the opioid crisis comprehensively.
The Life-Saving Impact of Overdose Reversal Medications in Combating the Opioid Crisis
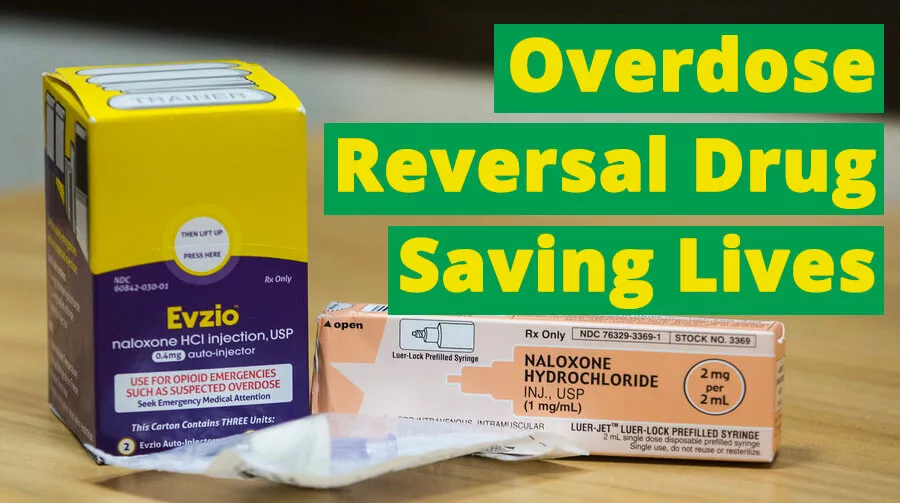
Overdose reversal medications are vital tools in the fight against the opioid crisis, designed to counteract the effects of opioid overdoses rapidly. These medications, like naloxone (commonly known by brand names such as Narcan and Evzio), work by binding to the same brain receptors as opioids, effectively reversing their toxic effects. Available as nasal sprays, intramuscular injections, and auto-injectors, naloxone can be administered by bystanders, first responders, and healthcare professionals to prevent fatal outcomes in overdose situations.
Here’s why overdose reversal medications like naloxone are essential:
- Rapid Response to Opioid Overdoses
Opioid overdoses often lead to respiratory depression, which can be fatal if not promptly addressed. Naloxone quickly restores normal breathing, offering an immediate, potentially life-saving emergency intervention. - Preventing Fatalities
Without swift action, opioid overdoses can be fatal. Naloxone, when administered in time, effectively reverses the overdose, offering the individual a second chance at life and averting tragedy. - Accessibility for Bystanders
Naloxone is designed to be easy to use and is available in various forms, including nasal sprays and auto-injectors. This accessibility enables friends, family, and community members—often without medical training—to act as first responders, making a critical difference in life-threatening situations. - Empowering Communities
Expanding access to naloxone empowers communities to take an active role in addressing overdoses. Public health initiatives and harm reduction programs prioritize making naloxone readily available, fostering a sense of communal support in the face of the opioid crisis. - Bridge to Professional Medical Care
While naloxone is not a substitute for comprehensive medical care, it buys essential time by temporarily reversing the overdose, allowing first responders to transport the individual to the hospital for follow-up treatment. - Reducing Stigma and Promoting Harm Reduction
The widespread availability of overdose reversal medications helps reduce the stigma surrounding substance use disorders. By emphasizing a harm reduction approach, communities can prioritize life-saving interventions and encourage people to seek help for their addiction without shame or judgment. - Protecting First Responders
Paramedics, law enforcement officers, and other first responders frequently encounter opioid overdoses. By carrying naloxone, they are equipped to respond quickly, ensuring their safety and enabling them to provide life-saving care. - Addressing the Opioid Crisis
Given the ongoing opioid crisis, distributing overdose reversal medications is an essential component of a comprehensive response. Naloxone alone is not the solution, but it’s a crucial tool in reducing opioid-related fatalities, helping individuals survive long enough to access treatment and recovery resources.
Overdose reversal medications like naloxone are indispensable tools in tackling the opioid crisis. By providing a rapid, effective response to opioid overdoses, these medications save lives, empower communities, and foster a compassionate, harm-reduction approach to addiction. Increasing naloxone accessibility is essential not only to reduce fatalities but also to offer individuals a path toward recovery and healing.
Overdose Education and Naloxone Distribution (OEND) Programs: A Community-Driven Approach to Combatting Opioid Overdoses
Overdose Education and Naloxone Distribution (OEND) programs are a robust response to the opioid crisis aimed at reducing overdose fatalities and empowering communities to respond effectively in emergencies. These programs provide critical education on recognizing opioid overdoses, offer training on naloxone administration, and prioritize community engagement to build a collective effort against opioid-related harm. Here’s how OEND programs contribute to decreasing opioid overdoses:
1. Empowering Bystanders
OEND programs equip community members—including friends, family, and bystanders—with the knowledge to recognize an overdose and administer naloxone. By making naloxone available and providing essential training, OEND programs empower everyday individuals to act swiftly, increasing the chances of survival for those experiencing an overdose.
2. Enabling Timely Intervention
Opioid overdoses can result in respiratory failure, and timely intervention is crucial. OEND programs provide education on spotting overdose symptoms and how to use naloxone correctly, reducing the time between recognizing an overdose and administering this life-saving medication.
3. Expanding Access to Naloxone
Traditionally available only to first responders or healthcare workers, naloxone is now distributed widely through OEND programs, making it accessible to individuals who may witness an overdose in the community. This broader access ensures that the necessary tools for overdose reversal are readily available when and where they are needed most.
4. Fostering Community Engagement
By involving local communities in overdose prevention, OEND programs foster a sense of shared responsibility and unity. Community members become actively engaged in preventing opioid overdoses, creating a network of support, and increasing awareness about the realities of addiction and the importance of harm reduction.
5. Reducing Stigma Around Substance Use
By framing naloxone as a vital tool for harm reduction, OEND programs play a role in destigmatizing opioid use disorders. This perspective encourages a compassionate, non-judgmental approach to substance use, focusing on the importance of saving lives and supporting individuals in their recovery journeys.
6. Making a Public Health Impact
With opioid overdoses reaching epidemic levels in many regions, OEND programs have a substantial public health impact by helping to decrease overdose fatalities. These programs are essential to overdose prevention efforts, contributing to safer communities and improving overall public health and well-being.
7. Integrating with Harm Reduction Strategies
OEND programs align with harm reduction principles, emphasizing practical, non-punitive strategies to mitigate the adverse consequences of drug use. By making naloxone accessible, these programs acknowledge the realities of opioid use and promote safety and health within the community.
8. Training First Responders and Professionals
Alongside community members, OEND programs also extend training to first responders—such as law enforcement officers and emergency medical personnel—ensuring they are well-prepared to recognize and respond to opioid overdoses effectively. This inclusive training provides a comprehensive approach to overdose prevention across all community levels.
In summary, OEND programs are an essential, community-driven approach to combatting opioid overdoses. Through education, expanded access to naloxone, and community engagement, these programs provide communities with the tools and knowledge to make a meaningful impact in the fight against opioid overdose fatalities. By reducing stigma, fostering a sense of collective responsibility, and aligning with harm reduction strategies, OEND programs are saving lives and helping communities come together to address the opioid crisis compassionately and proactively.
Challenges in Overdose Reversal: Addressing the Barriers to Effective Naloxone Use and Distribution
Overdose reversal medications, like naloxone, have become invaluable tools in the fight against opioid overdose fatalities. However, despite their life-saving potential, these medications face several significant challenges. From distribution barriers to societal stigma, here’s a look at the obstacles to effective naloxone use and how they can be addressed.
1. Access and Distribution
Ensuring that naloxone is available to those most at risk is a significant challenge, particularly in rural or underserved communities. Distributing naloxone in remote areas requires coordinated outreach efforts, partnerships with local organizations, and resource allocation to improve access for all.
2. Stigma and Awareness
The stigma around addiction and overdose can prevent people from seeking naloxone or administering it. Some individuals may believe naloxone encourages drug use, or they may hold misconceptions about its safety. Education campaigns are crucial to dispelling myths, emphasizing naloxone’s role as a life-saving tool, and fostering a compassionate response to addiction.
3. Training and Education
Effective naloxone use requires proper training. Lack of awareness programs and accessible training can make bystanders hesitant or uncertain about administering naloxone. Implementing widespread training initiatives can empower individuals to act quickly and confidently during an overdose emergency.
4. Legislation and Regulation
Regulatory barriers can impact access to naloxone. Some areas require prescriptions, or there may be legal restrictions on their availability. More lives could be saved by addressing these legal hurdles and supporting policies that allow greater access. Clear and consistent regulations help normalize the availability and use of naloxone as part of harm reduction efforts.
5. Cost and Affordability
The cost of naloxone can be prohibitive, especially for individuals without insurance. To increase accessibility, public health programs and insurance coverage should prioritize making naloxone affordable. Subsidizing its cost for high-risk communities can make a substantial difference in accessibility.
6. Quality of Training Materials
Inconsistencies in training materials and program quality can lead to improper naloxone administration. Ensuring training resources are standardized, up-to-date, and accessible will improve bystanders’ readiness to use naloxone effectively.
7. Complexity of Administration
While naloxone is designed for user-friendly administration, the stress of an emergency can impact bystanders’ ability to administer it effectively. Simplified instruction and greater public exposure to naloxone training can help alleviate this challenge, making it easier to respond accurately under pressure.
8. Response Time
Naloxone’s effectiveness depends on timely administration, and delays in recognizing an overdose can reduce its efficacy. Promoting community awareness of overdose signs and symptoms can help bystanders react more quickly, ensuring naloxone is administered promptly when needed.
9. Fear of Legal Consequences
Some individuals may hesitate to administer naloxone due to fear of legal repercussions, even with Good Samaritan laws in place. Increasing public knowledge about these legal protections can alleviate fears and encourage people to step in without hesitation.
10. Follow-Up Care
Naloxone reverses an overdose temporarily, but it is not a substitute for medical treatment. Individuals who receive naloxone often need further care and support for long-term recovery. Strengthening post-overdose resources and ensuring a smooth transition to follow-up care can improve outcomes and support lasting recovery.
In summary, while overdose reversal medications like naloxone have proven essential in saving lives, overcoming these challenges is critical to maximizing their impact. Addressing barriers to distribution, fostering community education, promoting legal protections, and ensuring seamless follow-up care are necessary to make naloxone as effective as possible. With a comprehensive approach, communities can help ensure that naloxone is accessible, properly used, and fully integrated into public health strategies to reduce opioid overdose fatalities.
The Role of Family Support in Enhancing the Effectiveness of Opioid Reversal Medications Like Naloxone
Family support is a vital component in maximizing the life-saving impact of opioid reversal medications, such as naloxone, and in helping individuals with opioid use disorders pursue recovery. A family’s role goes beyond just administering naloxone during an overdose emergency—it involves creating an environment of understanding, safety, and support. Here are key family strategies that can make a difference:
1. Education and Training
Educating family members about recognizing overdose symptoms and properly administering naloxone can empower them to act quickly and confidently in emergencies. Comprehensive training sessions, often available through local health organizations or online, can equip family members with critical knowledge and the skills needed to intervene effectively.
2. Naloxone Distribution and Accessibility
Families need to have naloxone on hand and readily accessible. Keeping multiple doses available is prudent, especially for severe overdoses or in cases where emergency services may be delayed. Families should agree on where naloxone is stored and ensure everyone can access it immediately.
3. Open Communication
Fostering open, non-judgmental communication creates an environment where individuals feel safe to express their struggles and needs. This openness can break down the stigma associated with opioid use disorders and make individuals more likely to seek help and use naloxone in emergencies.
4. Creating a Supportive Environment
Individuals struggling with addiction often face stigma, which can worsen feelings of isolation. By providing a supportive, understanding, and non-judgmental home environment, families can encourage loved ones to pursue treatment and recovery options without fear of shame or rejection.
5. Encouraging Treatment and Recovery
While naloxone is crucial in emergencies, it is not a long-term solution. Family members can support individuals accessing comprehensive treatment, including counseling, medication-assisted treatment (MAT), and support groups. By promoting a multifaceted approach, families can help their loved ones establish a foundation for recovery.
6. Safety Planning for Emergencies
Preparing a safety plan with clear steps for managing an overdose can reduce panic and confusion. This plan can include overdose signs, emergency contacts, and information on nearby treatment facilities. When family members know what to do in a crisis, they can act faster and more effectively.
7. Monitoring and Supervision
Families can take measures to help reduce overdose risks, such as safely storing medications, monitoring treatment adherence, and minimizing access to opioids. This level of support should respect boundaries but can be particularly useful when an individual is in early recovery.
8. Accessing Support Services for the Family
Addiction affects the whole family. Counseling, support groups, or family therapy can help address the emotional and relational impact of addiction, allowing families to approach the situation with empathy and resilience.
9. Empowering Family Members as Recovery Allies
Empowering family members with knowledge about addiction, communication skills, and how to offer emotional support is essential for effective involvement in the recovery journey. This understanding can also make families more compassionate and patient during challenging times.
10. Ensuring Follow-Up Care
After an overdose reversal, it’s essential to connect the individual with follow-up care and appropriate treatment. Family members can play an active role by assisting with appointment scheduling, transportation, and other logistics to ensure that recovery support is consistent and accessible.
11. Addressing Underlying Issues
Often, substance use is linked to underlying challenges, such as mental health issues, past trauma, or environmental stressors. Working with professionals to address these root causes can create a more supportive foundation for recovery, making naloxone interventions and other treatments more effective over the long term.
In summary, family support is an ongoing, adaptable process, but when family members take active, informed roles, they can significantly contribute to the effectiveness of opioid reversal medications like naloxone. Beyond emergency response, a supportive family can help create the conditions for sustained recovery, encouraging individuals to seek help, pursue treatment, and work toward a healthier, addiction-free future.
Harnessing Community Resources to Enhance Overdose Reversal Initiatives: Strategies for Naloxone Distribution Programs
Overdose reversal medications like naloxone are potent tools in addressing the opioid crisis, but their effectiveness relies on community support and accessibility. By implementing community-based strategies, we can expand access to naloxone and empower community members to respond to opioid overdoses effectively. Here are critical strategies for utilizing community resources to support naloxone distribution and overdose prevention:
1. Establish Naloxone Distribution Programs
Local naloxone distribution programs make this life-saving medication accessible to individuals at risk of overdose and their families. These programs can operate through health departments, pharmacies, clinics, and nonprofits, ensuring naloxone is readily available throughout the community.
2. Offer Training and Education
Providing training sessions on overdose recognition and naloxone administration is essential. These can include workshops, local events, and collaborative programs with community organizations, helping residents learn what to do in emergencies and build confidence in using naloxone.
3. Community Outreach and Awareness Campaigns
Raising awareness about naloxone’s availability and benefits is crucial for community-wide impact. Utilize social media, local news, posters, and in-person events to inform residents about where they can access naloxone, how it works, and the steps to take during an overdose.
4. Collaborate with Healthcare Providers
Partnerships with healthcare providers, clinics, and pharmacies can ensure that at-risk individuals have access to naloxone when they need it. Providers can discuss the importance of naloxone with patients who may be at risk or know someone at risk, strengthening distribution and access points within the community.
5. Create Peer Support Networks
Peer support networks enable those with personal experience in addiction and recovery to play a vital role. By offering support and information about naloxone, peer advocates reduce stigma and encourage individuals struggling with addiction to seek help and keep naloxone on hand.
6. Deploy Mobile Outreach Units
Mobile outreach units, equipped with naloxone and staffed by trained professionals, can reach areas with high opioid use. These units can distribute naloxone, provide on-site training, and connect individuals to local services, enhancing support where needed most.
7. Integrate with Community Health Clinics
Community health centers are valuable naloxone distribution points, as many individuals seeking healthcare services are likely at risk of or affected by opioid use. Offering naloxone here ensures easy access and an opportunity for education during regular health visits.
8. Combine with Harm Reduction Services
Integrating naloxone distribution into existing harm reduction services, such as needle exchanges and safe consumption sites, reaches those actively using opioids and in need of immediate overdose prevention support. This approach aligns with harm reduction principles by addressing immediate health risks.
9. Organize Community Training Events
Hosting training events led by healthcare professionals, addiction specialists, or first responders can engage community members directly. These events educate the public, distribute naloxone, and offer a space for questions, ensuring clarity and understanding about overdose response.
10. Promote Crisis Helplines and Hotlines
Making crisis helplines accessible in the community can provide immediate support during overdose events. Through these resources, people can get guidance on administering naloxone, access emergency assistance, and learn about local treatment and support services.
11. Form Community Partnerships
Building partnerships with schools, businesses, faith-based institutions, and local organizations strengthens naloxone distribution efforts. Together, these entities can broaden naloxone access and promote community well-being, fostering a shared responsibility for overdose prevention.
12. Monitor and Evaluate Programs
Implementing mechanisms to track and assess the impact of naloxone distribution programs is essential for continual improvement. Monitoring data on naloxone use, overdose reversals, and follow-up care provides valuable insights into program effectiveness and areas for enhancement.
In summary, community-based strategies can transform the accessibility and effectiveness of naloxone. By establishing distribution points, providing education, and forming partnerships, communities can create a robust safety net for individuals at risk of overdose. These collective efforts are essential in addressing the opioid crisis, fostering resilience, and promoting health and well-being throughout the community.
Conclusion
Overdose reversal medications stand as powerful tools in the battle against opioid-related fatalities, offering a lifeline that can bridge the gap between life and death during critical moments of overdose. Their purpose is unmistakable — to save lives and provide a second chance for individuals trapped by the grips of opioid misuse. However, challenges persist in ensuring the widespread distribution, accessibility, and acceptance of these vital medications. Yet, within these challenges lie opportunities for change, and the support systems of family and community resources emerge as crucial pillars in this endeavor. Family support, coupled with community initiatives, can bolster the impact of overdose reversal medications, fostering a collective commitment to combating the opioid crisis. As we navigate the complexities of this public health challenge, it becomes clear that a united front, fortified by education, awareness, and compassion, is essential for maximizing the effectiveness of overdose reversal strategies and, ultimately, saving lives.