Opioid overdose deaths among individuals aged 65 and older pose a significant public health challenge, demanding targeted interventions. Government efforts focus on safe prescribing practices, expanding treatment access, and raising awareness. Alongside these, self-management strategies, family support networks, and community resources are vital in prevention. This introduction outlines the multifaceted approach needed to address opioid overdose deaths among older adults, emphasizing collaborative efforts for their well-being.
Understanding the Rising Opioid Overdose Death Rates Among Older Adults: Factors and Solutions
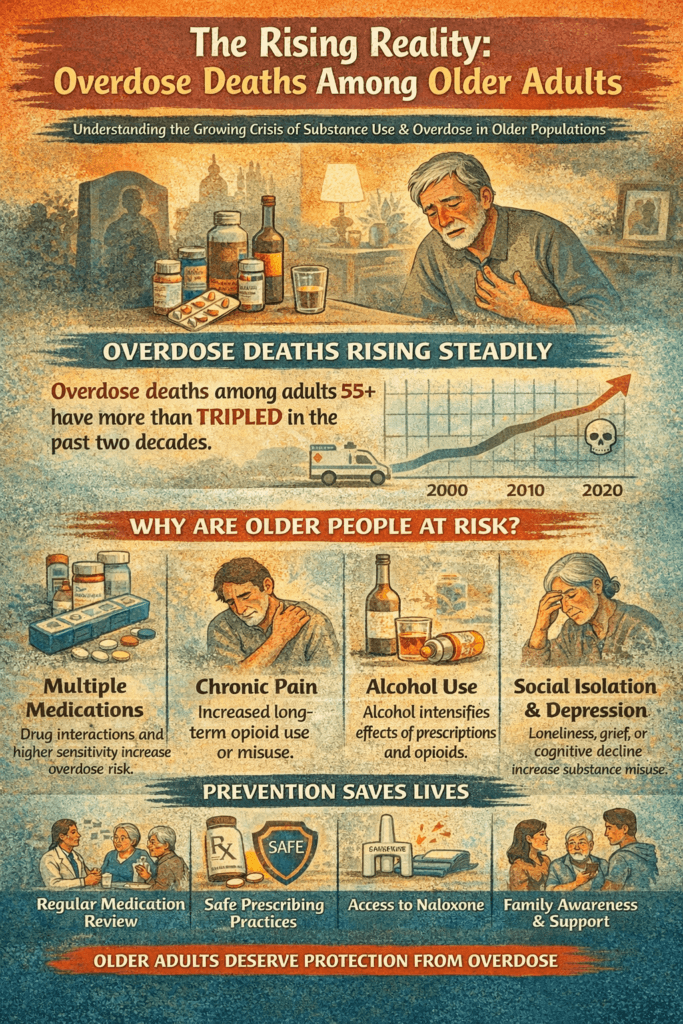
The alarming rise in opioid overdose death rates among individuals aged 65 and older has become a pressing public health concern. This demographic, often overlooked in discussions about substance use disorders, faces unique challenges that contribute to the increasing prevalence of opioid-related fatalities. Understanding the factors behind this trend is essential for developing effective interventions and support systems.
1. Prescription Opioid Misuse
Many older adults are prescribed opioids to manage chronic pain conditions such as arthritis or neuropathy. While these medications can provide relief, prolonged use can lead to misuse or dependence, especially as individuals may not be fully aware of the risks involved. Age-related changes in metabolism and physiology also make older adults more vulnerable to the adverse effects of opioids, heightening the risk of overdose.
2. Polypharmacy and Drug Interactions
Polypharmacy—taking multiple medications simultaneously—is common among older adults. This increases the risk of drug interactions that can be dangerous, particularly when opioids are combined with other depressants such as benzodiazepines or certain antidepressants. These combinations can amplify the soothing effects on the central nervous system, leading to respiratory depression and an increased risk of overdose.
3. Chronic Health Conditions
Chronic health issues are prevalent in older adults, necessitating the use of opioids for effective pain management. However, underlying conditions can complicate treatment, as they may exacerbate the risk of adverse outcomes, including opioid-related overdose. The complex health landscape of older adults requires careful management to mitigate these risks.
4. Stigma and Underreporting
The stigma surrounding substance use disorders is a significant barrier for older adults. Many may hesitate to seek help or disclose opioid misuse due to fear of judgment. This underreporting can delay necessary interventions and treatment, contributing to the escalating risk of overdose-related fatalities.
5. Limited Access to Treatment
Older adults often face numerous barriers when it comes to accessing addiction treatment services. These can include a lack of awareness about available resources, financial constraints, transportation difficulties, or cognitive and physical impairments. Such barriers can hinder timely intervention, exacerbating opioid-related harms.
6. Physician Prescribing Practices
Historically, healthcare providers have been more inclined to prescribe opioids liberally to older adults for pain management. This approach often occurs without a comprehensive evaluation of the potential risks and benefits. There is a pressing need to address inappropriate prescribing practices and enhance provider education to minimize the risk of opioid-related harms in this vulnerable population.
7. Social Isolation and Loneliness
Social isolation and loneliness are prevalent among older adults, which can increase the risk of substance use disorders, including opioid misuse. A lack of social support networks and meaningful engagement may lead some individuals to cope with their feelings through substance use, further compounding the issue.
Addressing the rising opioid overdose death rates among older adults necessitates a multifaceted approach. Key strategies should include:
- Targeted Prevention Efforts: Initiatives focused on educating older adults about the risks of opioid use and promoting safe medication practices can play a crucial role in prevention.
- Improved Access to Evidence-Based Treatment: Enhancing the availability of treatment and support services tailored to older adults is essential for timely intervention.
- Enhanced Provider Education: Training healthcare providers on the risks associated with opioid prescribing for older adults can lead to safer prescribing practices.
- Promotion of Alternatives for Pain Management: Encouraging non-opioid therapies and comprehensive medication management can mitigate the reliance on opioids for pain relief.
- Fostering Social Connections: Programs designed to combat social isolation among older adults can provide essential support and reduce the risk of substance misuse.
By adopting a comprehensive strategy, we can work towards mitigating the risk of opioid-related harms among older adults, ultimately promoting their health and well-being in a supportive environment.
Government Interventions to Combat Opioid Overdose Deaths Among Older Adults
As the opioid crisis continues to affect communities across the United States, one of the most vulnerable populations is individuals aged 65 and older. With rising rates of opioid overdose deaths in this demographic, government interventions have become crucial in addressing this urgent public health issue. These interventions involve a comprehensive approach that combines policies, programs, and initiatives designed to prevent opioid misuse, promote safe prescribing practices, improve access to treatment, and raise awareness of the risks associated with opioid use. Here’s an overview of some common government interventions aimed at preventing opioid overdose deaths among older adults.
1. Prescription Drug Monitoring Programs (PDMPs)
PDMPs are essential tools in tracking the prescribing and dispensing of controlled substances, including opioids. These electronic databases provide healthcare providers with access to patients’ prescription histories, helping to identify cases of overprescribing, misuse, or polypharmacy. By monitoring prescribing patterns, PDMPs can deter inappropriate prescribing and facilitate timely interventions.
2. Provider Education and Training
Government agencies offer training and educational resources to healthcare providers to promote safer prescribing practices. This education covers appropriate pain management strategies, the risks associated with opioid use in older adults, and the importance of screening for substance use disorders. Providers are also encouraged to assess pain in older adults effectively and consider non-opioid alternatives for pain management.
3. Clinical Guidelines and Recommendations
Organizations such as the Centers for Disease Control and Prevention (CDC) and the Substance Abuse and Mental Health Services Administration (SAMHSA) develop and disseminate clinical guidelines that inform healthcare providers about evidence-based practices for opioid prescribing. These guidelines are vital for ensuring that older adults receive appropriate care tailored to their specific needs, minimizing the risk of misuse and overdose.
4. Opioid Prescribing Limits and Regulations
Some states have introduced policies that limit the quantity and duration of opioid prescriptions, particularly for acute pain. These regulations are designed to reduce the likelihood of opioid misuse and dependence among older adults. Additionally, many states require prescribers to obtain informed consent and conduct regular reassessments when prescribing opioids for chronic pain, ensuring ongoing evaluation of the necessity and effectiveness of treatment.
5. Expansion of Access to Addiction Treatment
To address the specific needs of older adults struggling with opioid use, government agencies are allocating funding to expand access to addiction treatment and recovery support services. This includes medication-assisted treatment (MAT) options, such as buprenorphine or methadone, and initiatives that integrate addiction treatment into primary care settings. Increasing the availability of specialized services for older adults is essential for timely and effective intervention.
6. Naloxone Distribution Programs
Naloxone, a life-saving medication used to reverse opioid overdoses, is a critical component of overdose prevention efforts. Government agencies have implemented naloxone distribution programs that provide training and naloxone kits to healthcare providers, first responders, and community members, including caregivers of older adults. Ensuring that those who interact with older adults are equipped with naloxone can significantly reduce opioid-related fatalities.
7. Public Awareness Campaigns
Public awareness campaigns targeting older adults, their caregivers, and healthcare providers are vital for raising awareness about the risks of opioid use. These campaigns inform communities about the signs of opioid overdose, available resources for prevention and treatment, and the importance of safe medication practices. Increasing knowledge and understanding can empower individuals and families to take proactive steps in managing opioid-related risks.
8. Research and Surveillance
Finally, government agencies support research initiatives that aim to understand the epidemiology of opioid use and overdose among older adults. By identifying risk factors and evaluating the effectiveness of interventions, these research efforts provide valuable insights that can inform policy decisions and enhance prevention strategies. Surveillance systems that monitor trends in opioid-related morbidity and mortality are essential for adapting interventions to the evolving landscape of opioid use among older adults.
In summary, the multifaceted approach taken by government interventions is critical for addressing the rising rates of opioid overdose deaths among older adults. By implementing strategies that include prescription monitoring, provider education, clinical guidelines, and access to treatment, policymakers aim to create a safer environment for older adults while promoting effective pain management practices. Collaborative efforts between government agencies, healthcare providers, and communities are essential to mitigate the risks associated with opioid use and ensure the health and well-being of this vulnerable population. Through continued commitment to these interventions, we can work towards a future where opioid-related harms are significantly reduced among older adults.
Self-Management Strategies to Prevent Opioid Overdose Deaths Among Older Adults
As the opioid crisis continues to pose significant risks, particularly for older adults, individuals aged 65 and older need to engage in self-management strategies actively. These strategies empower them to take control of their health and safety, ultimately helping to prevent opioid overdose deaths. Here are some critical self-management strategies explicitly tailored for older adults.
1. Medication Management
Adherence to Prescribed Regimens:
Older adults must take medications exactly as prescribed by their healthcare providers. This includes adhering to the recommended dosage and schedule for opioids and other drugs. By following these guidelines, individuals can minimize the risk of overdose and ensure the effectiveness of their treatment.
Review Medications Regularly:
It is essential to periodically review all medications with healthcare providers. This review helps identify potential interactions or side effects and ensures that the treatment plan remains appropriate and effective. Keeping an updated list of all medications can facilitate these discussions.
2. Pain Management Alternatives
Explore Non-Opioid Pain Relief:
Older adults should discuss non-opioid alternatives for pain management with their healthcare providers. Options such as physical therapy, acupuncture, massage therapy, or over-the-counter pain relievers can effectively alleviate pain while minimizing reliance on opioids.
3. Safe Storage and Disposal
Secure Medications:
Storing opioids and other medications securely is vital to prevent accidental ingestion or misuse. Keeping medications out of reach of children and visitors—ideally in a locked cabinet or container—can significantly reduce the risk of accidents.
Dispose of Unused Medications:
Proper disposal of unused or expired medications is essential for preventing diversion and accidental ingestion. Older adults should utilize community drug take-back programs or follow FDA guidelines for safe disposal to ensure that medications do not pose a risk.
4. Risk Reduction Strategies
Limit Alcohol Consumption:
Older adults should avoid excessive alcohol consumption while taking opioids. Alcohol can enhance the depressant effects of opioids, increasing the risk of respiratory depression and overdose.
Avoid Combining Medications:
It is crucial to avoid combining opioids with other sedating medications, such as benzodiazepines or certain sleep aids, without consulting healthcare providers. This practice can further increase the risk of respiratory depression and overdose.
5. Recognition and Response to Overdose
Learn Signs of Overdose:
Education about the signs and symptoms of opioid overdose is vital. Older adults and their caregivers should recognize symptoms such as slowed or shallow breathing, confusion, and loss of consciousness, enabling them to act quickly in an emergency.
Have Naloxone Available:
Having naloxone on hand is a necessary precaution. This medication can reverse opioid overdoses and should be prescribed or recommended by healthcare providers. Caregivers should be trained to administer naloxone in an emergency.
6. Regular Monitoring and Communication
Monitor for Adverse Effects:
Older adults should actively monitor for potential adverse effects of opioid medications, such as dizziness, drowsiness, constipation, or changes in mood or cognition. Reporting any concerns to healthcare providers promptly can lead to timely interventions.
Open Communication with Providers:
Maintaining open communication with healthcare providers about pain management, medication use, and any changes in health status or medication effectiveness is crucial. This dialogue allows for adjustments to the treatment plan as needed, ensuring that individuals receive the best possible care.
7. Healthy Lifestyle Habits
Maintain Overall Health:
It is vital to prioritize overall health and well-being through regular physical activity, balanced nutrition, adequate hydration, and sufficient sleep. These lifestyle habits support the body’s ability to cope with pain and stress, promoting a healthier, more resilient individual.
Overall, by implementing these self-management strategies, older adults can minimize the risk of opioid overdose while promoting safer medication use. These strategies empower individuals to maintain their independence and quality of life, equipping them with the tools needed to navigate the complexities of pain management more safely. With awareness and proactive measures, older adults can significantly reduce risk and lead healthier, more fulfilling lives.
Family Support Strategies to Prevent Opioid Overdose Deaths Among Older Adults
Opioid overdose deaths among older adults are a growing concern, making family support essential in navigating the complexities of medication management and pain relief. Family members can play a crucial role in preventing these tragic outcomes by providing guidance, education, and emotional support. Here are several strategies tailored specifically for families to support older adults and reduce the risk of opioid overdose.
1. Medication Management Assistance
Assist with Medication Organization:
Family members can help older adults organize their medications, including opioids, to ensure clarity around dosages and schedules. Using pill organizers or medication management apps can simplify this process.
Remind and Encourage Adherence:
Regular reminders and encouragement to take medications as prescribed can improve adherence. Family members should also monitor for signs of medication misuse or adverse effects, allowing for early intervention when necessary.
2. Communication and Monitoring
Open Dialogue:
Maintaining open and honest communication about pain management, medication use, and any health concerns is vital. Family members should create a safe space for older adults to discuss their feelings and experiences related to their medications.
Monitor for Signs of Overdose:
Education is key. Family members should be aware of the signs and symptoms of opioid overdose, such as slowed or shallow breathing, confusion, and loss of consciousness. This vigilance can lead to timely responses in emergencies.
3. Safe Storage and Disposal of Medications
Secure Medications:
To prevent accidental ingestion or misuse, family members should ensure that opioids and other medications are stored securely and out of reach of children and visitors. A locked cabinet can provide an additional layer of safety.
Dispose of Unused Medications:
Family members can help older adults properly dispose of unused or expired medications. Utilizing community drug take-back programs or following FDA guidelines for safe disposal can help mitigate risks associated with unused opioids.
4. Risk Reduction Strategies
Encourage Limiting Alcohol:
Family members should encourage older adults to limit alcohol consumption while taking opioids, as the combination can increase the risk of respiratory depression and overdose. Open discussions about the potential dangers can help reinforce this guideline.
Monitor for Drug Interactions:
Being vigilant about potential drug interactions between opioids and other medications is essential. Family members should discuss any concerns with healthcare providers to ensure a comprehensive approach to medication management.
5. Emergency Response Preparedness
Provide Naloxone Training:
If recommended by healthcare providers, family members should receive training on how to administer naloxone, a life-saving medication that can reverse opioid overdoses. Being prepared can make a critical difference in emergencies.
Create Emergency Plans:
Developing and practicing emergency response plans with older adults is crucial. This plan should include instructions on recognizing and responding to opioid overdoses, ensuring everyone knows their role in case of an emergency.
6. Emotional Support and Encouragement
Offer Emotional Support:
Providing emotional support and reassurance is vital for older adults who may be experiencing pain, anxiety, or depression. Family members should encourage them to seek help from healthcare providers or counselors when needed.
Celebrate Progress:
Acknowledge and celebrate milestones and achievements in pain management and medication adherence. Reinforcing positive behaviors can enhance motivation and foster a sense of accomplishment.
7. Education and Advocacy
Educate Family Members:
Educating family members about the risks associated with opioid use in older adults can promote safer practices. Understanding the complexities of pain management can foster a supportive environment for the older adult.
Advocate for Access to Support Services:
Family members should advocate for older adults’ access to addiction treatment and support services, helping them navigate healthcare systems to receive appropriate care. This advocacy ensures that older adults receive the support they need.
In summary, by implementing these family support strategies, caregivers and loved ones can significantly contribute to promoting safer medication use and preventing opioid overdose deaths among older adults. The collaborative efforts of family members not only enhance the well-being of older adults but also foster a supportive environment where they can thrive. Together, we can make a meaningful difference in the lives of our loved ones as they navigate the challenges of opioid use and pain management.
Community Resource Strategies to Prevent Opioid Overdose Deaths Among Older Adults
As the opioid crisis continues to impact communities across the nation, older adults are particularly vulnerable to the risks associated with opioid use and overdose. To effectively combat this issue, communities must leverage local services, organizations, and resources to provide education, support, and intervention tailored to this population. Here are some key community resource strategies to prevent opioid overdose deaths among people aged 65 and older.
1. Senior Centers and Community Organizations
Education and Awareness Programs:
Partnering with senior centers and community organizations can create opportunities to host educational workshops and seminars. These sessions should focus on opioid safety, medication management, and recognizing signs of overdose among older adults. Tailored programs can empower older adults and their families with the knowledge needed to make informed decisions about pain management.
Support Groups:
Facilitating support groups or peer-led discussions specifically for older adults and their caregivers provides a safe space to share experiences and learn coping strategies. These groups can help individuals navigate the complexities of managing pain and medications while offering mutual support.
2. Healthcare Providers and Pharmacies
Educational Materials:
Distributing educational materials about opioid safety, medication management, and naloxone administration to healthcare providers and pharmacies can enhance awareness. This ensures that older adults receive consistent messaging from various healthcare touchpoints.
Pharmacist Consultations:
Offering pharmacist consultations or medication reviews for older adults can be instrumental in discussing medications, potential drug interactions, and safe storage and disposal practices. Pharmacists can play a crucial role in providing personalized advice to mitigate risks.
3. Local Health Departments and Agencies
Naloxone Distribution Programs:
Collaborating with local health departments to implement naloxone distribution programs can save lives. Providing training and naloxone kits to older adults and caregivers, along with education on how to recognize and respond to opioid overdose, is essential for community safety.
Community Outreach Events:
Organizing community outreach events or health fairs focused on opioid safety can help raise awareness. These events can offer free naloxone training, medication reviews, and referrals to addiction treatment and support services.
4. Community-Based Organizations and Coalitions
Coalition Building:
Establishing or supporting coalitions composed of healthcare providers, community leaders, law enforcement agencies, and other stakeholders allows for a comprehensive approach to opioid overdose prevention initiatives. Collaborative efforts can lead to the development of targeted programs that address the unique needs of older adults.
Peer Navigator Programs:
Training peer navigators or community health workers to provide outreach, education, and support can significantly benefit older adults. These individuals can assist with medication management, help access support services, and navigate the complexities of healthcare systems.
5. Public Awareness Campaigns
Media Outreach:
Launching public awareness campaigns through local media outlets—such as newspapers, radio stations, and social media—can increase visibility around opioid safety and overdose prevention. Engaging the public through various channels ensures the message reaches a broader audience.
Community Events and Activities:
Participating in community events, health fairs, and senior expos allows organizations to disseminate information and distribute educational materials directly to older adults and their families. This face-to-face engagement fosters trust and encourages conversations about opioid-related issues.
6. Emergency Services and First Responders
Collaboration with Emergency Services:
Partnering with emergency medical services (EMS) and first responders is vital for ensuring timely access to naloxone and emergency medical care. Collaborative training can help first responders understand the unique challenges older adults face in overdose situations.
Training for First Responders:
Providing specialized training for EMS personnel and first responders on identifying and responding to opioid overdoses in older adults can improve outcomes. This training should consider age-related factors and common comorbidities among older patients.
In summary, by implementing these community resource strategies, local stakeholders can work together to strengthen support networks, raise awareness, and provide accessible resources and services to prevent opioid overdose deaths among older adults. A collaborative approach that combines education, support, and intervention can make a meaningful difference in safeguarding the health and well-being of older adults in our communities. Together, we can build a safer future for our elders, ensuring they receive the care and support they need to thrive.
Frequently Asked Questions
Here are some common questions:
Are older adults really at risk for overdose?
Yes. Overdose deaths among older adults have increased significantly due to medication sensitivity, chronic health conditions, and multiple prescription drug use.
Why do aging bodies increase overdose risk?
As people age, the liver and kidneys process drugs more slowly, and the nervous system becomes more sensitive, meaning standard doses can become too strong.
Do prescription medications cause most overdoses in older adults?
Many overdoses involve prescribed opioids, benzodiazepines, or sleep medications, especially when combined or taken incorrectly.
Can alcohol increase overdose risk in seniors?
Yes. Alcohol interacts with many medications and can intensify sedation and breathing suppression, raising overdose risk even at low amounts.
Does chronic pain contribute to overdose risk?
Older adults are more likely to receive long-term opioid treatment for pain, which increases dependence and accidental overdose risk.
Are illicit drugs a factor for older adults, too?
Yes. Fentanyl contamination in illicit drug supplies has led to unexpected overdoses in older individuals who may not realize the drug strength.
Does social isolation increase overdose deaths?
Yes. Living alone means an overdose may go unnoticed, delaying life-saving emergency response.
Can cognitive decline affect medication safety?
Memory problems or confusion can lead to double-dosing or improper medication mixing.
Are overdose deaths in older adults preventable?
Yes. Medication reviews, safer prescribing, naloxone access, and family awareness significantly reduce risk.
What is the first step in protecting an older loved one?
Talking openly with healthcare providers about medication safety, substance use, and mental health is the most effective starting point.
Conclusion
Addressing opioid overdose deaths among individuals aged 65 and older requires a comprehensive approach that integrates government interventions, self-management strategies, family support, and community resources. While government efforts focus on policy implementation, treatment access, and awareness campaigns, individual self-management strategies empower older adults to take control of their health and medication use. Additionally, family support networks provide essential emotional and practical assistance, while community resources offer education, naloxone distribution, and peer support. By combining these approaches, we can effectively prevent opioid overdose deaths among older adults, safeguarding their health and well-being for years to come.
Video: Senior Overdoses Are Skyrocketing, and Nobody Noticed #epidemic #elderly #crisis