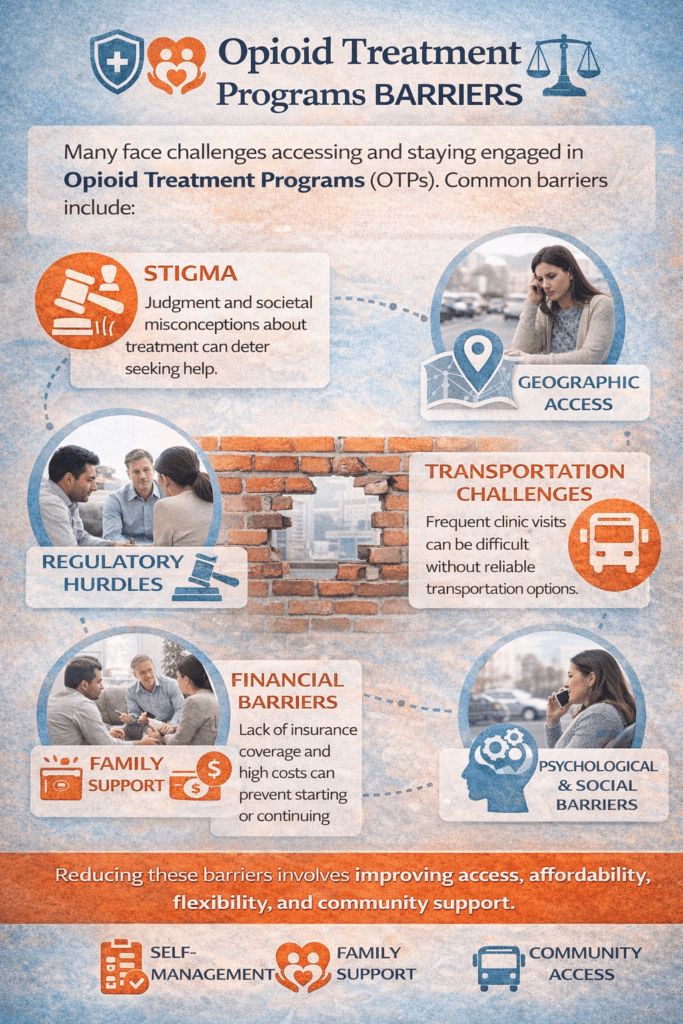
Opioid Treatment Programs (OTPs) are evidence-based and lifesaving for individuals with opioid use disorder (OUD), yet many people encounter significant barriers that limit access and retention. These barriers include stigma, transportation difficulties, financial constraints, regulatory requirements, fragmented healthcare systems, and emotional resistance rooted in fear or shame. When individuals are unable to engage consistently in treatment, the risk of relapse and overdose increases. Addressing OTP barriers requires more than policy reform alone—it demands coordinated strategies at the individual, family, and community levels to create sustainable access to care.
Opioid Treatment Program Barriers: Why Access to Care Remains a Challenge
Opioid Treatment Programs (OTPs) are a cornerstone of care for individuals with opioid use disorder (OUD), offering medication-assisted treatment (MAT) such as methadone or buprenorphine alongside counseling and support services. Despite strong evidence that these programs reduce overdose risk, improve stability, and support long-term recovery, significant barriers continue to limit access and engagement.
One of the most persistent barriers is stigma. Individuals seeking treatment often face judgment from employers, family members, and even healthcare professionals. Misunderstandings about MAT—such as the belief that it “replaces one drug with another”—discourage people from initiating or remaining in care. Internalized shame can also prevent individuals from seeking help early.
Geographic access remains another major challenge. Rural and underserved communities may have few or no OTPs within a reasonable travel distance. Because some programs require frequent in-person visits—especially early in treatment—transportation limitations can impede consistent attendance. For individuals without reliable transportation or access to public transit, this barrier can be insurmountable.
Regulatory requirements can also complicate access. While safeguards are designed to ensure safety and prevent diversion, strict rules governing daily dosing, documentation, and compliance may impose burdens on individuals balancing work, childcare, or unstable housing. Although regulations have evolved in recent years, administrative complexity continues to affect engagement.
Financial barriers add another layer of difficulty. While Medicaid and insurance coverage have expanded, gaps remain. Prior authorizations, limited provider networks, copayments, and lack of insurance coverage in some regions delay treatment initiation. For uninsured individuals, out-of-pocket costs can deter care-seeking.
Psychological and social barriers are equally important. Fear of withdrawal, concerns about side effects, co-occurring mental health conditions, and mistrust of systems can prevent sustained participation. Additionally, individuals involved in the criminal justice system or child welfare cases may experience fragmented care coordination.
Cultural and systemic inequities further complicate access. Communities disproportionately affected by opioid misuse often face reduced healthcare infrastructure and social resources. Language barriers, immigration concerns, and discrimination can prevent individuals from seeking services.
Addressing OTP barriers requires multifaceted solutions. Expanding telehealth, increasing mobile treatment units, integrating addiction care into primary healthcare, improving insurance coverage, and reducing stigma through public education are essential steps. Trauma-informed care and peer support models can also enhance trust and retention.
Opioid Treatment Programs are evidence-based and lifesaving—but only if they are accessible. Removing structural, financial, and social barriers is not simply a healthcare priority; it is a public health imperative. Expanding equitable access to treatment is one of the most powerful tools available to reduce overdose deaths and support long-term recovery.
Self-Management Strategies to Overcome Opioid Treatment Program Barriers
Opioid Treatment Programs (OTPs) provide evidence-based care for opioid use disorder (OUD), yet many individuals encounter barriers such as stigma, transportation challenges, scheduling conflicts, financial stress, and emotional resistance. While systemic reform is essential, self-management strategies can help individuals navigate obstacles and remain engaged in treatment.
One of the most powerful strategies is proactive planning. Mapping out appointment schedules, transportation options, and backup plans reduces missed visits. Setting reminders, arranging rides in advance, or coordinating with employers early can prevent avoidable disruptions. Structured daily routines also stabilize recovery and reduce last-minute stress.
Education is another key tool. Understanding how medication-assisted treatment (MAT) works—whether methadone or buprenorphine—can reduce internalized stigma and strengthen motivation. When individuals recognize that MAT supports brain stabilization and lowers overdose risk, adherence often improves. Asking providers questions and staying informed increases confidence in the process.
Stress management is critical when facing barriers. Anxiety about court requirements, work schedules, or family responsibilities can increase relapse risk. Practicing mindfulness, exercise, journaling, or breathing techniques strengthens emotional regulation during high-pressure situations. Recognizing stress early and using coping skills reduces impulsive decision-making.
Building a recovery support network also enhances resilience. Peer recovery groups, sponsors, recovery coaches, and supportive family members can help problem-solve barriers. Sharing experiences with others who have navigated similar challenges reduces isolation and builds accountability.
Financial navigation skills are equally important. Exploring Medicaid eligibility, payment plans, sliding-scale options, or community assistance programs can ease cost concerns. Many clinics have case managers who can help identify local resources—proactively engaging with them is part of effective self-management.
Communication plays a central role. Informing providers about scheduling conflicts, transportation limitations, or side effects allows for collaborative adjustments. Many programs now offer telehealth components or modified dosing schedules when clinically appropriate. Transparent dialogue prevents small issues from becoming treatment interruptions.
Finally, maintaining a long-term perspective matters. Barriers may feel overwhelming in the moment, but consistent engagement in treatment significantly reduces overdose risk and improves life stability. Recovery is a process, not a single event. Viewing challenges as obstacles to navigate—rather than signs of failure—builds persistence.
While systemic change is necessary to eliminate structural barriers, individuals can strengthen their ability to remain in care through planning, education, stress regulation, communication, and support. Self-management transforms barriers into manageable challenges and sustains recovery.
Family Support Strategies to Overcome Opioid Treatment Program Barriers
Opioid Treatment Programs (OTPs) are highly effective in treating opioid use disorder (OUD), yet many individuals face barriers such as stigma, transportation challenges, financial strain, regulatory requirements, and emotional stress. Family support can play a decisive role in helping individuals overcome these obstacles and remain engaged in care.
One of the most immediate ways families can help is through practical support. Providing transportation to appointments, assisting with childcare, or helping manage work schedules reduces logistical stress. Early treatment often requires frequent visits, and reliable family assistance can prevent missed doses or program discharge due to nonattendance.
Emotional support is equally important. Stigma remains one of the largest barriers to treatment. When families view medication-assisted treatment (MAT) as legitimate medical care rather than “replacing one drug with another,” they reinforce recovery rather than undermine it. Encouraging words, nonjudgmental listening, and reassurance during setbacks help sustain motivation.
Families can also assist by helping organize documentation and communication. Court requirements, insurance paperwork, or program compliance expectations can feel overwhelming. A supportive family member who helps track appointments, medication schedules, and case requirements reduces anxiety and improves adherence.
Education strengthens family effectiveness. Learning about opioid use disorder as a chronic brain-based condition fosters compassion and realistic expectations. Understanding relapse risk, treatment timelines, and recovery milestones helps families respond calmly rather than reactively during challenges.
Boundary-setting is another essential strategy. Support should not turn into enabling. Clear expectations regarding treatment attendance, sobriety goals, and respectful behavior protect both the individual and the family system. Balanced boundaries promote accountability while maintaining encouragement.
Participation in family therapy or support groups further enhances outcomes. Programs such as family counseling sessions and peer-led family support groups provide guidance on communication skills, stress management, and relapse-prevention strategies. These settings also allow family members to process their own fears and frustrations in a healthy way.
Finally, families can advocate at the community level. Encouraging employers to understand treatment schedules, helping navigate insurance coverage, or connecting loved ones with local recovery resources strengthens long-term stability.
Overcoming OTP barriers is rarely a solo effort. When families provide structured support, education, practical assistance, and compassionate accountability, they significantly increase the likelihood of sustained treatment engagement. Strong family involvement transforms barriers into manageable challenges and reinforces a stable path toward recovery.
Community Resource Strategies to Overcome Barriers in Opioid Treatment Programs
Opioid Treatment Programs (OTPs) are one of the most effective interventions for opioid use disorder (OUD), yet many individuals face structural barriers that limit access and retention. These barriers include geographic distance, stigma, transportation limitations, regulatory complexity, financial strain, and fragmented care systems. Community resource strategies are essential to closing these gaps and ensuring equitable access to lifesaving treatment.
One of the most effective strategies is to expand geographic access. Mobile treatment units and satellite clinics help serve rural and underserved communities where traditional OTP facilities may be scarce. Bringing services directly into neighborhoods reduces travel burdens and increases early engagement in care.
Transportation assistance programs are another critical community-level intervention. Partnerships with public transit systems, ride-share vouchers, and nonprofit transportation services can significantly reduce missed appointments. For many individuals, lack of reliable transportation is a primary reason for treatment discontinuation.
Telehealth integration has also become a powerful tool in reducing barriers. Virtual counseling sessions, remote check-ins, and hybrid treatment models improve flexibility for individuals balancing employment, childcare, or court obligations. When implemented appropriately, telehealth increases retention while maintaining safety standards.
Financial accessibility remains central. Communities can support sliding-scale payment options, expand Medicaid enrollment assistance, and connect individuals to grant-funded programs. Outreach workers and case managers play a key role in helping patients navigate insurance enrollment and benefit eligibility.
Stigma reduction initiatives are equally important. Public education campaigns, recovery-friendly workplace programs, and community forums can reshape perceptions of medication-assisted treatment (MAT). When communities understand that MAT reduces overdose risk and supports long-term stability, individuals feel safer seeking care.
Integrated care models further reduce fragmentation. Collaboration between primary care providers, mental health services, social services, and OTPs ensures comprehensive treatment. Addressing co-occurring mental health conditions, housing instability, and employment challenges strengthens recovery outcomes.
Peer recovery networks add another essential layer. Community recovery centers, peer mentors, and support groups provide lived-experience guidance, encouragement, and accountability. These networks help individuals navigate barriers in real time and maintain motivation during setbacks.
Ultimately, overcoming OTP barriers requires systemic coordination. Community strategies that improve access, affordability, flexibility, and public understanding transform treatment from a limited service into a comprehensive support network. When communities invest in accessible and integrated care, they not only reduce overdose deaths but also build sustainable pathways toward long-term recovery and stability.
Frequently Asked Questions
Here are some common questions:
1. What are Opioid Treatment Programs (OTPs)?
OTPs are specialized programs that treat opioid use disorder (OUD) using medication-assisted treatment (MAT) such as methadone or buprenorphine, combined with counseling and supportive services.
2. What are the most common barriers to accessing OTPs?
Common barriers include stigma, transportation challenges, limited geographic access (especially in rural areas), financial constraints, insurance limitations, regulatory requirements, and psychological resistance to treatment.
3. Why is stigma such a major barrier?
Many individuals face judgment or misconceptions about MAT, including the belief that it “replaces one addiction with another.” This stigma can discourage people from seeking or continuing treatment.
4. How does transportation affect treatment participation?
Some OTPs require frequent in-person visits, particularly during early stabilization. Without reliable transportation, patients may miss appointments, risking program discharge or relapse.
5. Are financial issues a common obstacle?
Yes. Insurance gaps, prior authorizations, copayments, and the lack of Medicaid coverage in certain areas can delay or prevent access to treatment.
6. Do regulations make it harder to stay in treatment?
In some cases, yes. Strict dosing schedules, daily clinic visits, documentation requirements, and compliance rules can create scheduling conflicts for individuals balancing work, childcare, or legal obligations.
7. How do mental health conditions impact OTP engagement?
Co-occurring anxiety, depression, trauma, or untreated psychiatric conditions can reduce motivation and make consistent participation more difficult.
8. Are rural communities affected differently?
Yes. Rural areas often have fewer OTP facilities, greater distances to travel, and limited public transportation, thereby increasing access barriers.
9. What strategies can help overcome these barriers?
Solutions include expanding telehealth services, deploying mobile treatment units, providing transportation assistance, implementing integrated care models, offering insurance enrollment support, reducing stigma, and supporting peer recovery programs.
10. Can family involvement reduce barriers?
Absolutely. Family members can provide transportation, childcare, emotional support, accountability, and assistance in navigating financial or administrative challenges.
11. Why is addressing OTP barriers so important?
Removing barriers increases treatment retention, reduces overdose risk, improves long-term recovery outcomes, and strengthens public health overall.
12. Is overcoming OTP barriers possible?
Yes. With coordinated efforts at the individual, family, and community levels, many barriers can be reduced or eliminated, making treatment more accessible and sustainable.
Conclusion
Overcoming barriers to Opioid Treatment Programs is most effective when self-management, family support, and community resources work together. Individuals who proactively schedule appointments, manage stress, communicate openly with providers, and establish recovery routines strengthen their ability to remain engaged in care. Families who provide practical assistance, education, encouragement, and structured accountability reduce logistical and emotional obstacles. Communities that expand access through telehealth, transportation services, integrated care models, financial assistance, and stigma-reduction efforts create an environment in which treatment is accessible rather than burdensome. When these layers align, barriers become manageable challenges—and recovery becomes a realistic, sustainable path forward.
Video: Help Exists, But Not for Everyone #opioidcrisis #inequity #publichealth