The opioid crisis in the United States persists, and current drug therapies face challenges in making a significant impact. This difficulty arises due to a combination of factors: the cultural mindset towards addiction, logistical hurdles, and ideological barriers. Cultural stigmatization of substance use disorders, coupled with an individualistic approach to health, hinders comprehensive treatment. Logistical challenges include limited access to treatment, insurance obstacles, and a fragmented healthcare system. Ideological barriers rooted in historical perspectives on addiction complicate the development of practical solutions. Addressing these interwoven cultural, logistical, and ideological aspects is crucial for advancing interventions that can truly address the complexities of the opioid crisis.
Understanding Why the Opioid Crisis Persists Despite Treatment Efforts
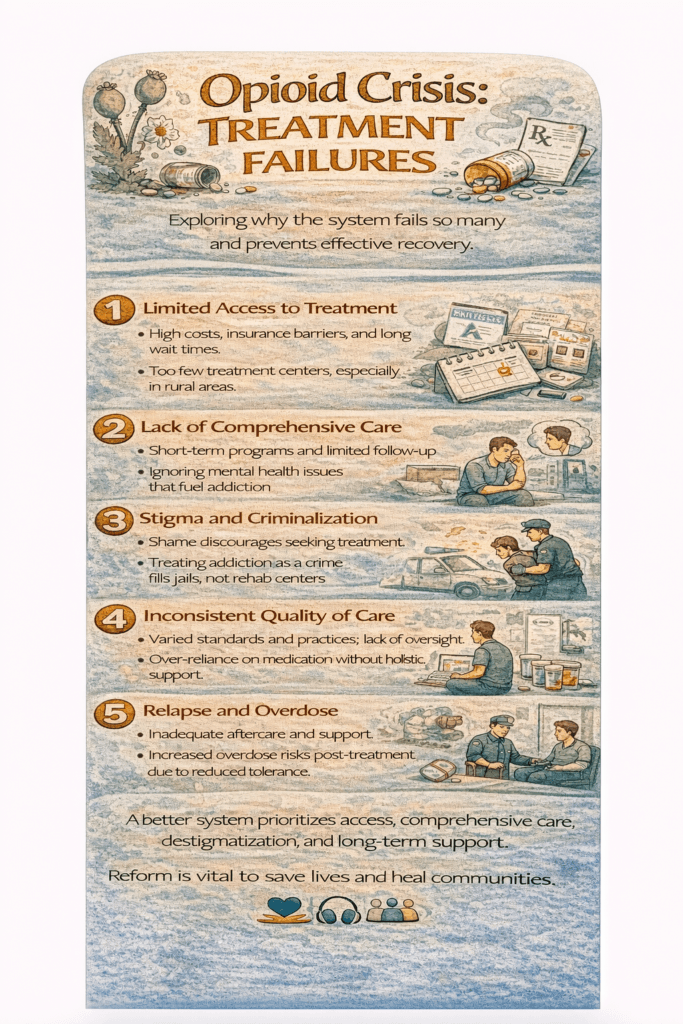
The opioid crisis remains a significant public health challenge, despite ongoing efforts to curb its impact through treatment and prevention initiatives. A deeper look at the barriers and complexities reveals why current approaches have yet to fully mitigate the crisis.
1. Access Barriers
Limited access to effective treatments, particularly medication-assisted treatment (MAT), is a significant obstacle. Issues such as a shortage of specialized facilities, inadequate healthcare coverage, and long waiting lists for treatment programs leave many individuals without timely care.
2. Stigma and Discrimination
Stigma surrounding opioid use disorder (OUD) continues to hinder progress. The societal perception of addiction as a moral failing rather than a medical condition discourages individuals from seeking help. Additionally, discrimination within healthcare settings can further deter access to treatment.
3. Poly-Substance Use
The co-use of multiple substances, such as opioids with stimulants or benzodiazepines, complicates treatment. Addressing poly-substance use requires tailored interventions that consider the unique risks and challenges posed by combining substances.
4. Treatment Gaps in Correctional Systems
Correctional facilities often fail to provide evidence-based treatments for individuals with OUD. Without proper care during incarceration, many individuals are at high risk of relapse and overdose upon release, perpetuating a cycle of addiction and reincarceration.
5. Social Determinants of Health
Factors like poverty, unemployment, lack of education, and unstable housing significantly contribute to substance use disorders. Addressing these root causes is essential, as focusing solely on the symptoms of addiction without tackling the underlying issues often limits treatment success.
6. Opioid Overprescribing Practices
Historical overprescribing of opioids played a critical role in fueling the crisis. Although stricter regulations and guidelines have been implemented, the long-term effects of this practice continue to ripple through affected communities, complicating recovery efforts.
7. Emergence of Synthetic Opioids
The rise of synthetic opioids like fentanyl has intensified the crisis. These substances are significantly more potent than traditional opioids, leading to increased overdose deaths and presenting new challenges for both prevention and treatment efforts.
8. Lack of Coordination in Care
Fragmentation within healthcare systems often results in disjointed treatment approaches. Without comprehensive and integrated care that addresses both physical and mental health needs, individuals with OUD may struggle to achieve sustained recovery.
9. Trauma and Co-occurring Disorders
Many individuals with OUD have experienced significant trauma or live with co-occurring mental health disorders. These complex cases require specialized care that addresses both addiction and underlying psychological issues, but such resources are often scarce.
10. Treatment Resistance and Innovation Gaps
Not all individuals respond effectively to existing treatments. This highlights the need for ongoing research to develop innovative, personalized treatment approaches that address a diverse range of needs and circumstances.
In summary, the persistence of the opioid crisis underscores the need for a multifaceted and adaptive response. Beyond increasing access to evidence-based treatments, efforts must address systemic issues, reduce stigma, and promote coordinated care. Tackling social determinants of health and adapting strategies to the evolving dynamics of the crisis—such as the rise of synthetic opioids—are equally critical.
A sustained and holistic approach that combines public health, policy, and community engagement holds the key to making significant strides against the opioid epidemic.
How Americans’ Cultural Mindset Affects Access to Treatment for Substance Use Disorders
Cultural values and attitudes in the United States play a significant role in shaping how substance use disorders, including opioid addiction, are understood and addressed. While efforts to combat addiction have grown, cultural barriers still impact access to treatment, perpetuating stigma and hindering progress.
1. Stigma and Shame
Cultural narratives often frame addiction as a personal failure, leading to stigma and shame for individuals seeking help. Many fear being judged as morally flawed or weak, which deters them from pursuing the professional treatment they need.
2. Addiction as a Moral Issue
The traditional view of addiction as a moral failing rather than a medical condition prevents widespread acceptance of evidence-based treatment. This moral framing shifts focus from recovery and rehabilitation to blame, further alienating those in need of care.
3. Emphasis on Individualism
The U.S. cultural emphasis on individualism places responsibility for addiction squarely on the individual, often ignoring systemic or societal factors. This mindset fosters the belief that overcoming addiction should be a solitary effort, discouraging individuals from seeking external support or treatment.
4. Reluctance to Disclose Struggles
Many Americans value privacy and may be reluctant to disclose personal challenges, including addiction. This reluctance can delay or entirely prevent individuals from seeking professional help, as they may avoid discussing their substance use issues even with trusted healthcare providers.
5. Mistrust of the Healthcare System
For marginalized communities, historical injustices and ongoing disparities in healthcare contribute to mistrust of treatment providers. This mistrust often translates to skepticism about addiction treatment programs, particularly among those who feel underserved or discriminated against by the healthcare system.
6. Lack of Cultural Competence in Treatment
Effective addiction treatment requires cultural competence among providers. When treatment programs fail to align with individuals’ cultural values or lack understanding of diverse cultural backgrounds, patients may feel disconnected or misunderstood, reducing their engagement and commitment to recovery.
7. Delayed Treatment-Seeking
The cultural expectation of self-reliance often leads individuals to delay seeking treatment, attempting instead to “tough it out” or manage addiction on their own. This delay can exacerbate the condition, making eventual recovery efforts more challenging.
8. Limited Public Dialogue
In many cultural contexts, discussions about mental health and addiction remain limited. This lack of open dialogue perpetuates stigma and reduces awareness of available treatments, leaving many individuals and families unaware of where to turn for help.
9. Preference for Self-Help Approaches
Cultural preferences for self-help and self-reliance often lead individuals to seek non-professional methods, such as self-detoxification or unregulated support groups. While these approaches may provide temporary relief, they are often insufficient for addressing the complexities of substance use disorders.
10. Financial and Insurance Concerns
Beliefs about financial independence and self-sufficiency can influence decisions about whether to use insurance or seek financial assistance for treatment. Concerns about confidentiality, particularly in employer-based insurance plans, also deter many from accessing care.
Solutions to Cultural Barriers
To improve access to treatment for substance use disorders, it is crucial to:
- Promote Cultural Competence: Healthcare providers must be trained to deliver care that aligns with their patients’ diverse cultural values and needs.
- Reduce Stigma: Public education campaigns and advocacy can help reframe addiction as a health issue rather than a moral failing.
- Encourage Open Conversations: Normalizing discussions about mental health and addiction can reduce shame and make treatment-seeking more acceptable.
- Enhance Access to Resources: Expanding treatment availability and ensuring affordability can address economic barriers, while targeted outreach can build trust with marginalized communities.
Addressing the opioid crisis requires a cultural shift that acknowledges addiction as a complex health issue and fosters a supportive environment for seeking treatment. By challenging stigmatizing narratives and enhancing cultural competence in healthcare, we can improve access to effective interventions and create a more compassionate approach to combating addiction.
Logistical and Ideological Obstacles to Drug Dependency Treatment
Efforts to address substance use disorders (SUDs) face significant challenges due to logistical and ideological obstacles. These barriers, stemming from systemic inefficiencies, cultural beliefs, and policy decisions, complicate access to and the effectiveness of treatment. Understanding these challenges is essential for creating actionable solutions.
1. Treatment Accessibility
- Logistical Barrier: Access to treatment facilities is often limited, especially in rural or underserved areas. Long travel distances, sparse resources, and extended waiting periods can discourage individuals from seeking timely help.
- Ideological Barrier: While many believe treatment should be universally accessible, resource limitations and healthcare inequities expose the gap between this ideal and the reality of existing infrastructure.
2. Insurance Barriers
- Logistical Barrier: Many individuals face inadequate insurance coverage, high out-of-pocket costs, and restrictions on treatment types or duration. These financial obstacles significantly limit access to necessary, long-term care.
- Ideological Barrier: Ideological resistance to expanding healthcare coverage perpetuates restrictive policies, limiting the scope of benefits available for substance use disorder treatments.
3. Fragmented Healthcare System
- Logistical Barrier: A lack of coordination among mental health services, addiction treatments, and primary care creates fragmented and disjointed care, leaving individuals without comprehensive support.
- Ideological Barrier: Resistance to integrated care models reflects a historical and ideological separation of addiction treatment from general healthcare, hindering systemic improvements.
4. Stigma and Discrimination
- Logistical Barrier: Stigma surrounding addiction often discourages individuals from seeking help due to fear of judgment or social exclusion, even from healthcare providers.
- Ideological Barrier: Societal beliefs that addiction represents a moral failing or personal weakness perpetuate discriminatory attitudes and prevent the development of compassionate care environments.
5. Criminalization of Substance Use
- Logistical Barrier: Legal consequences of drug use often interrupt treatment efforts. Those facing incarceration may lose access to ongoing care, creating a cycle of relapse and punishment.
- Ideological Barrier: Viewing substance use as a criminal issue rather than a public health concern limits the adoption of harm reduction strategies and evidence-based treatments.
6. Ideological Differences in Treatment Approaches
- Logistical Barrier: Divergent philosophies—such as abstinence-only versus harm reduction models—can hinder consensus on best practices, leading to inconsistent care.
- Ideological Barrier: Ideological opposition to harm reduction methods, like medication-assisted treatment (MAT), often impedes the adoption of proven, evidence-based interventions.
7. Lack of Cultural Competence
- Logistical Barrier: Treatment programs may fail to address the cultural and linguistic needs of diverse populations, leaving many individuals feeling alienated and less likely to engage in care.
- Ideological Barrier: Resistance to integrating culturally sensitive approaches stems from a failure to recognize the critical role of cultural competence in effective treatment delivery.
Strategies for Overcoming Obstacles
Addressing these barriers requires both systemic reforms and cultural shifts:
- Expand Treatment Access: Increase funding for treatment facilities, especially in underserved areas, and reduce wait times through policy changes.
- Improve Insurance Coverage: Advocate for broader coverage of evidence-based SUD treatments to reduce financial burdens.
- Integrate Care Models: Develop systems that combine addiction treatment, mental health support, and primary care for holistic care.
- Reduce Stigma: Launch educational campaigns to frame addiction as a treatable medical condition, promoting empathy and understanding.
- Decriminalize Substance Use: Shift from punitive legal frameworks to public health approaches, focusing on rehabilitation and harm reduction.
- Adopt Evidence-Based Practices: Promote policies and practices that align with scientific research, prioritizing harm reduction over ideological resistance.
- Enhance Cultural Competence: Train healthcare providers to deliver care that respects and integrates cultural values and diversity.
Substance use disorder treatment requires a multifaceted response that addresses both logistical and ideological obstacles. By fostering systemic collaboration, reducing stigma, and adopting evidence-based approaches, society can bridge the gap between the need for effective treatment and the barriers that currently limit access. Recognizing addiction as a complex health issue—and not a moral failing—remains central to creating a compassionate and equitable response to this ongoing crisis.
Comprehensive Interventions to Tackle the Opioid Crisis
The opioid crisis remains a complex and urgent public health challenge, demanding a multifaceted and coordinated response. Effective interventions must span prevention, treatment, harm reduction, and systemic reform. Here’s a breakdown of the key strategies to mitigate the crisis:
1. Education and Prevention
- Implement community and school-based programs to educate individuals about the dangers of opioid misuse and alternative pain management strategies.
- Train healthcare providers on responsible opioid prescribing and promote public awareness about the risks of misuse.
2. Prescription Monitoring Programs (PDMPs)
- Strengthen PDMPs to track opioid prescriptions and flag patterns of overprescribing.
- Ensure healthcare providers have real-time access to these databases to support informed decision-making.
3. Responsible Prescribing Practices
- Encourage prescribers to assess the necessity of opioids, opt for non-opioid pain management options when possible, and prescribe the lowest effective dose.
4. Medication-Assisted Treatment (MAT)
- Expand access to MAT, which integrates FDA-approved medications like methadone, buprenorphine, and naltrexone with behavioral therapies.
- Remove barriers such as regulatory restrictions and inadequate insurance coverage that limit access to MAT programs.
5. Naloxone Distribution Programs
- Increase the availability of naloxone, an opioid overdose reversal medication, by training first responders, community members, and healthcare professionals on its administration.
6. Harm Reduction Strategies
- Support harm reduction initiatives like syringe exchange programs, supervised injection sites, and the distribution of fentanyl test strips to minimize the risk of overdose and infectious disease transmission.
7. Telehealth Services
- Expand telehealth options for substance use disorder treatment, providing remote access to therapy, counseling, and MAT—especially in rural and underserved areas.
8. Treatment Funding and Access
- Allocate funds to increase the availability of residential and outpatient treatment facilities and recovery support services.
- Address insurance barriers to ensure equitable access to care for all individuals, regardless of socioeconomic status.
9. Crisis Response Teams
- Establish multidisciplinary crisis response teams that include mental health professionals and social workers to provide immediate assistance during substance use-related crises.
10. Community-Based Recovery Support
- Foster support networks such as peer-led recovery groups, recovery coaching, and sober housing to promote long-term recovery and reintegration into society.
11. Criminal Justice Reform
- Transition from punitive measures to rehabilitative approaches, including drug courts and diversion programs that emphasize treatment over incarceration.
12. Research and Innovation
- Invest in research to develop non-opioid pain management options, explore genetic and environmental influences on addiction, and innovate more effective treatments for opioid use disorder.
13. Public Awareness Campaigns
- Launch campaigns to combat stigma, promote understanding of addiction as a medical condition, and encourage individuals to seek treatment without fear of judgment.
14. Policy Changes
- Advocate for policies that prioritize evidence-based solutions, increase funding for addiction treatment, and address systemic barriers contributing to the opioid crisis.
15. Cultural Shifts
- Foster a societal understanding of addiction as a medical condition rather than a moral failing, emphasizing empathy and support for those in recovery.
Collaboration is Key
No single intervention can resolve the opioid crisis. It requires a cohesive, multi-pronged approach involving healthcare professionals, policymakers, community organizations, and individuals. Together, these efforts can create a sustainable framework to address the root causes, reduce the harm, and support recovery for those affected by this devastating epidemic.
Frequently Asked Questions
Here are some common questions:
What does “treatment failure” mean in the opioid crisis?
Treatment failure refers to situations where individuals do not achieve sustained recovery despite receiving addiction treatment. This may include relapse, dropping out of programs, or lack of access to effective care.
Why do many opioid treatment programs fail?
Failures often result from limited treatment availability, short program duration, inadequate follow-up care, stigma, financial barriers, and insufficient integration of mental health services.
Is relapse always a sign of treatment failure?
No. Relapse is a common part of chronic disease management. However, repeated relapse without treatment adjustment may indicate that care approaches are not meeting individual needs.
How does lack of access contribute to treatment failure?
Many communities lack affordable treatment centers, medication-assisted treatment providers, or transportation. Long waitlists and insurance limitations delay care when it is most needed.
Do short-term rehab programs contribute to poor outcomes?
Yes. Brief detox or 30-day programs without continued therapy and medication support often fail to address long-term recovery needs, increasing relapse risk.
How does stigma impact treatment success?
Stigma discourages individuals from seeking help, reduces family and community support, and can lead to discrimination in healthcare settings.
What role does mental health play in treatment failure?
Untreated trauma, depression, anxiety, and other mental health conditions often drive substance use. Without integrated mental health care, recovery is harder to sustain.
Are medications for opioid use disorder underused?
Yes. Evidence-based medications like buprenorphine, methadone, and naltrexone are proven effective, yet many programs still do not offer them due to policy or provider shortages.
How does the criminal justice system affect treatment outcomes?
Incarceration without treatment interrupts recovery. Upon release, lack of support and reduced tolerance increase overdose risk.
What improvements reduce treatment failure?
Long-term medication access, continuous counseling, peer support, harm-reduction services, housing stability, and family involvement significantly improve success rates.
Does treatment failure mean recovery is impossible?
No. Recovery is achievable. Treatment failures highlight system gaps, not personal weakness. Adjusted care and sustained support can lead to long-term recovery.
Conclusion
The persistently challenging landscape of the opioid crisis in the United States underscores the limitations of current drug therapies. Despite advancements, the efficacy of these treatments is hampered by deeply ingrained cultural attitudes towards addiction, logistical impediments, and ideological barriers. The reluctance to view addiction as a medical condition, coupled with limited treatment accessibility and systemic fragmentation, continues to impede progress. To forge a path forward, interventions must transcend not only the biological aspects of addiction but also address the intricate interplay of cultural, logistical, and ideological factors. By fostering a more supportive cultural mindset, dismantling logistical barriers, and embracing evidence-based policies, interventions can be tailored to better align with the complex realities of the opioid crisis, ultimately providing more effective and compassionate solutions.
Video: