Opioids and opiates are both substances that bind to opioid receptors in the brain. Still, while opiates are naturally derived from the opium poppy (e.g., morphine), opioids also include synthetic drugs like fentanyl. Both carry a high potential for addiction, as they trigger the release of dopamine, leading to physical dependence. Managing addiction requires effective self-management strategies, such as mindful pain management and exploring alternatives. Family support is crucial in providing emotional backing, fostering communication, and encouraging professional treatment. Community resources, including education, treatment centers, and support groups, offer essential services to help individuals prevent and recover from opioid and opiate addiction.
Understanding the Difference Between Opiates and Opioids
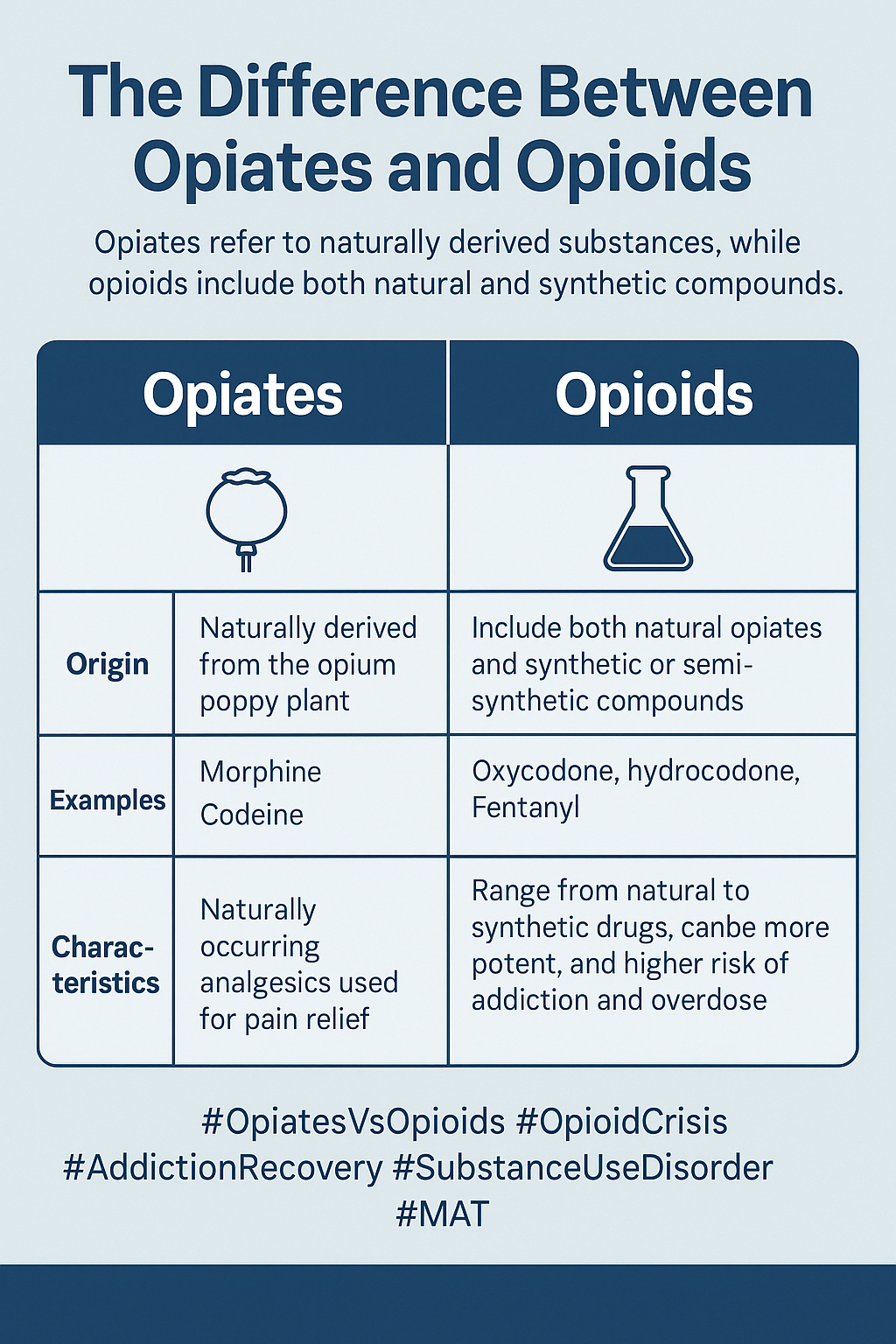
The terms “opiate” and “opioid” are often used interchangeably, but they refer to different categories of substances. Understanding the distinction between these terms is crucial, particularly in discussions about pain management, addiction, and public health policies.
Opiates: Naturally Derived Compounds
Definition: Opiates specifically refer to natural substances that are directly derived from the opium poppy plant (Papaver somniferum). These compounds occur naturally in the plant and have been used for centuries for their analgesic (pain-relieving) and sedative properties.
Examples:
- Morphine – A powerful pain reliever commonly used in medical settings.
- Codeine – Often found in prescription cough syrups and mild pain relievers.
- Thebaine – A less common alkaloid that serves as a precursor for the synthesis of some semi-synthetic opioids.
Opioids: A Broader Category
Definition: Opioids encompass a broader class of drugs that includes not only natural opiates but also semi-synthetic and fully synthetic substances that act on the opioid receptors in the brain and body. These substances are designed to mimic the effects of natural opiates, often with greater potency or different pharmacological properties.
Examples:
- Semi-Synthetic Opioids:
- Oxycodone – Found in medications such as OxyContin and Percocet.
- Hydrocodone – Commonly prescribed in combination with acetaminophen (e.g., Vicodin).
- Heroin – An illegal opioid synthesized from morphine.
- Fully Synthetic Opioids:
- Fentanyl – A highly potent synthetic opioid, often used for severe pain management and sometimes found in illicit drug markets.
- Methadone – Used in both pain management and opioid addiction treatment.
- Buprenorphine – A partial opioid agonist used in medication-assisted treatment (MAT) for opioid dependence.
Summary and Modern Usage
- Opiates refer specifically to natural opioids derived directly from the opium poppy plant.
- Opioids are a more inclusive term that covers all substances (natural, semi-synthetic, and synthetic) that act on opioid receptors.
- In contemporary medical and public health discussions, “opioid” is often used as the umbrella term to describe all drugs that affect the opioid receptors, whether natural or synthetic.
The Importance of Understanding These Terms
The distinction between opiates and opioids is more than just a matter of terminology—it has significant implications in medicine, addiction treatment, and law enforcement. The opioid crisis has led to increased awareness of these substances, their risks, and the need for effective strategies to address opioid addiction and misuse. Understanding these terms helps facilitate more accurate discussions and informed decision-making regarding pain management and substance use policies.
Are Opiates and Opioids the Same?
No, opiates and opioids are not the same, though they are closely related. Understanding their differences is essential for discussions on pain management, addiction, and medical treatment.
What Are Opiates?
Definition: Opiates refer specifically to natural substances derived directly from the opium poppy plant (Papaver somniferum). These compounds are extracted from the plant and have been used for centuries to relieve pain and induce sedation.
Examples of Opiates:
- Morphine – A naturally occurring alkaloid used for severe pain relief.
- Codeine – Commonly found in prescription cough syrups and mild pain medications.
- Thebaine – A natural compound used as a precursor for semi-synthetic opioids.
What Are Opioids?
Definition: Opioids are a broader term that includes all substances—natural, semi-synthetic, and synthetic—that interact with opioid receptors in the brain and body. While opiates are a type of opioid, the term “opioid” encompasses a much wider range of drugs, including synthetic versions designed to mimic the effects of natural opiates.
Types of Opioids:
- Natural Opiates (e.g., morphine, codeine)
- Semi-Synthetic Opioids – These are chemically modified derivatives of natural opiates.
- Oxycodone – Found in medications like OxyContin and Percocet.
- Hydrocodone – Used in medications such as Vicodin.
- Heroin – An illegal opioid synthesized from morphine.
- Synthetic Opioids – Entirely man-made substances that act on opioid receptors.
- Fentanyl – A highly potent synthetic opioid used for severe pain management.
- Methadone – Often used in opioid addiction treatment and pain management.
- Buprenorphine – Used in medication-assisted treatment (MAT) for opioid dependence.
Key Takeaways
- Opiates are natural substances derived directly from the opium poppy.
- Opioids are an umbrella term that includes all opiates, as well as semi-synthetic and synthetic drugs that act on opioid receptors.
- All opiates are opioids, but not all opioids are opiates.
Why Does This Distinction Matter?
The opioid crisis has brought increased awareness to the dangers of opioid misuse and addiction. Understanding the difference between opiates and opioids helps in making informed decisions regarding pain management, addiction treatment, and public health policies. Whether discussing prescription painkillers, illicit drugs, or addiction recovery strategies, using the correct terminology fosters more transparent communication and better awareness of these powerful substances.
Similarities Between Opiates and Opioids
Opiates and opioids share many similarities in their effects, mechanisms of action, and risks. While they differ in origin—opiates being naturally derived from the opium poppy and opioids including both natural and synthetic substances—their impact on the body is essentially the same. Here are the key similarities between these two classes of drugs:
1. Pain Relief
Both opiates and opioids are primarily used for their analgesic (pain-relieving) properties. They bind to opioid receptors in the brain and spinal cord, blocking pain signals and altering the perception of pain. This makes them highly effective in managing both acute and chronic pain.
2. Addictive Potential
Both substances have a high potential for addiction. They can produce feelings of euphoria and relaxation, which, when misused, can lead to physical dependence and addiction. The pleasurable effects of these drugs increase the risk of abuse, making long-term use potentially dangerous without medical supervision.
3. Mechanism of Action
Both opiates and opioids work by binding to opioid receptors—primarily the mu, delta, and kappa receptors—in the brain and central nervous system. This binding triggers the release of dopamine, a neurotransmitter associated with pleasure and reward. Over time, repeated exposure can lead to physical and psychological dependence.
4. Similar Side Effects
Opiates and opioids share common side effects, including:
- Drowsiness
- Constipation
- Nausea
- Respiratory depression
- Euphoria
These side effects contribute to both their therapeutic benefits and their potential for abuse and overdose.
5. Withdrawal Symptoms
When someone who has been using opiates or opioids regularly stops taking them, they may experience withdrawal symptoms. These include:
- Muscle aches
- Irritability
- Sweating
- Insomnia
- Cravings
Withdrawal occurs because both drug types affect the same opioid receptors in the body, leading to similar dependence and withdrawal patterns.
In summary, both opiates and opioids act on the same opioid receptors, provide pain relief, carry a risk of addiction, and cause similar side effects and withdrawal symptoms. The main distinction lies in their source: opiates are naturally derived, while opioids encompass both natural and synthetic substances. Despite their differences, their effects on the human body remain largely the same, underscoring the need for careful and responsible use in medical settings.
The Addictive Properties of Opiates and Opioids
Both opioids and opiates share similar addictive properties due to the way they interact with the brain’s reward system and opioid receptors. Understanding these addictive properties is essential for recognizing the risks associated with their use and the potential for dependency and addiction.
1. Interaction with the Brain’s Reward System
Opioids and opiates both bind to opioid receptors (mu, delta, and kappa receptors) in the brain and spinal cord, particularly the mu-opioid receptor, which plays a key role in the brain’s reward system.
- When these substances bind to these receptors, they trigger the release of dopamine, a neurotransmitter responsible for feelings of pleasure and reward.
- This dopamine release creates a sense of euphoria and well-being, reinforcing the behavior of using the substance and increasing the risk of addiction.
2. Euphoric Effects
Both opioids and opiates can produce intense feelings of pleasure and relaxation.
- This euphoric effect makes individuals want to use the substance repeatedly to experience these pleasurable feelings again.
- Repeated use can lead to psychological dependence, where the individual craves the drug even when it is no longer needed for pain relief.
3. Tolerance Development
Tolerance occurs when the body adapts to a substance, requiring higher doses to achieve the same effect.
- Both opioids and opiates can cause tolerance quickly, especially with regular or high-dose use.
- As tolerance builds, individuals may take larger amounts, increasing their risk of overdose and dependency.
4. Physical Dependence
Prolonged opioid or opiate use can lead to physical dependence, where the body becomes reliant on the substance to function normally.
- When someone dependent on opioids or opiates stops using them or reduces their dosage, they experience withdrawal symptoms such as:
- Muscle aches
- Nausea
- Anxiety
- Sweating
- Severe cases can include seizures or respiratory distress.
- The discomfort of withdrawal often drives continued use, reinforcing addiction.
5. The Addictive Cycle
The combination of euphoria, tolerance, and withdrawal creates a cycle that is difficult to break.
- Individuals continue using opioids or opiates to avoid withdrawal symptoms and chase the pleasurable high.
- Over time, dependence deepens, and drug use may take priority over work, relationships, and overall health, signaling addiction.
6. Psychological Dependence
Beyond physical dependence, opioids and opiates can lead to psychological addiction.
- Individuals may feel they need the substance to cope with emotional pain, stress, or anxiety.
- Cravings can be triggered by environmental cues (such as places where they previously used the drug) or emotional states (such as depression or stress).
7. Potential for Abuse
Both opioids and opiates are highly addictive, particularly when taken in non-prescribed ways, such as:
- Snorting or injecting the substance.
- Taking higher-than-prescribed doses.
- Using opioids obtained illegally.
Prescription opioids like oxycodone and hydrocodone are frequently misused for their euphoric effects, contributing to widespread addiction issues.
8. Overdose Risk
As tolerance increases, individuals may take dangerously high doses, significantly raising the risk of overdose.
- Opioid overdoses can cause respiratory depression, where breathing slows or stops entirely.
- Without immediate medical intervention, overdose can lead to death.
Both opioids and opiates are highly addictive due to their effects on dopamine release, which creates pleasurable feelings and reinforces continued use. Their potential for tolerance, physical dependence, and psychological cravings strengthens the cycle of addiction. Over time, the need to avoid withdrawal symptoms and the desire for euphoria can drive individuals to increase their usage, putting them at greater risk of overdose and severe health consequences.
Self-Management Strategies for Opiates and Opioids
Preventing opioid and opiate addiction requires a combination of proactive self-management strategies that promote overall well-being and reduce the risk of misuse. Here are several effective self-management strategies:
1. Education and Awareness
- Learn About Risks: Understanding the dangers of opioid and opiate use, including how addiction develops, the signs of misuse, and the potential for overdose, can help individuals make informed decisions about their health.
- Know Your Prescriptions: If prescribed opioids or opiates for pain management, it’s essential to be fully aware of the potential risks, dosing guidelines, and safe usage instructions.
2. Follow Medical Advice Carefully
- Strict Adherence to Prescription Guidelines: Always take opioids as directed by a healthcare professional. Never take more than the prescribed dose or use them for longer than necessary.
- Regular Check-ups with Healthcare Providers: Schedule follow-up appointments to monitor progress and assess the need for continued opioid use. Discuss alternative pain management strategies or tapering options if opioids are no longer necessary.
3. Non-Opioid Pain Management Alternatives
- Explore Alternatives: Consider non-addictive pain management options, including over-the-counter medications, physical therapy, acupuncture, chiropractic care, and mindfulness-based techniques.
- Physical Activity: Regular exercise can help manage chronic pain and improve mood. Activities like yoga, stretching, or walking can naturally increase endorphin production and reduce pain.
4. Mindfulness and Stress Management
- Mindfulness Meditation: Techniques like meditation, deep breathing, and progressive muscle relaxation can help manage stress, pain, and cravings.
- Cognitive Behavioral Strategies: Cognitive Behavioral Therapy (CBT) can help identify and challenge negative thought patterns that contribute to opioid misuse or cravings.
5. Develop Healthy Coping Mechanisms
- Healthy Outlets for Emotions: Develop healthier strategies, such as journaling, creative expression (art, music, etc.), or spending time in nature, instead of turning to opioids for emotional relief.
- Social Support: Stay connected with supportive friends, family members, or peers who can offer encouragement and accountability.
6. Set Boundaries and Avoid Triggers
- Avoid Risky Environments: Stay away from environments or social situations that may trigger opioid misuse.
- Recognize Triggers: Identify personal emotional, environmental, or social triggers and develop coping strategies, such as reaching out to a supportive friend or engaging in relaxation techniques.
7. Practice Self-Discipline
- Limit Access: Store prescription opioids securely and only take them when necessary. Avoid hoarding or misusing leftover prescriptions.
- Be Honest About Use: If you start to feel dependent on opioids or notice patterns of misuse, acknowledge it and seek help immediately.
8. Use Support Resources
- Peer Support Groups: Groups like Narcotics Anonymous (NA) or other peer recovery groups provide shared experiences, emotional support, and coping strategies.
- Therapy and Counseling: Regular therapy sessions, such as CBT, Dialectical Behavioral Therapy (DBT), or Motivational Interviewing (MI), can help address underlying mental health issues that may increase the risk of addiction.
9. Focus on Overall Well-Being
- Sleep Hygiene: Prioritize a healthy sleep routine to reduce stress and emotional imbalance.
- Balanced Nutrition: Eating a well-balanced diet supports mental and physical health, reducing stress and improving resilience.
- Engage in Healthy Hobbies: Pursuing activities that bring joy and fulfillment can reduce boredom or negative emotions that might trigger substance use.
10. Early Intervention
- Recognize Early Signs: Be aware of early signs of opioid misuse, such as increased tolerance, withdrawal symptoms, or cravings, and seek treatment early.
- Seek Professional Help: If there are signs of opioid misuse or a history of substance use disorder, seeking early intervention from healthcare providers or addiction specialists can prevent escalation.
11. Relapse Prevention Planning
- Develop a Relapse Plan: In case of a setback, have a plan in place, such as contacting a support group, therapist, or sponsor for immediate assistance.
By incorporating these self-management strategies into daily life, individuals can reduce their risk of opioid or opiate addiction and improve their ability to manage pain and emotional challenges without turning to harmful substances.
Family Support Strategies for Opiate and Opioid Use
Family support plays a critical role in preventing opioid and opiate addiction. A supportive family environment can help individuals manage pain, stress, and emotional challenges without resorting to substance misuse. Here are some effective family support strategies:
1. Open Communication
- Encourage Honest Conversations: Foster an environment where open, non-judgmental communication is encouraged. This allows individuals to express concerns or fears about using opioids, and it helps family members identify potential issues early.
- Discuss Risks of Opioid Use: Provide education about the dangers of opioid misuse and the risk of addiction, helping the individual understand the importance of responsible use and the consequences of misuse.
2. Support Healthy Choices
- Encourage Non-Opioid Alternatives: Support individuals in seeking non-opioid pain management strategies, such as physical therapy, exercise, mindfulness techniques, and over-the-counter medications.
- Promote Healthy Lifestyles: Encourage healthy habits like regular physical activity, nutritious eating, and maintaining a balanced routine. These habits can reduce the need for opioids and contribute to overall well-being.
3. Set Boundaries and Limits
- Help Manage Prescription Use: Monitor opioid prescriptions to ensure they are taken as prescribed and not misused. This includes limiting access to the medications and ensuring they are stored safely and securely.
- Establish Clear Expectations: Discuss and set clear expectations around the use of opioids, such as using them only when necessary, according to a doctor’s prescription, and under close supervision.
4. Encourage Professional Help
- Facilitate Access to Healthcare Providers: Assist with scheduling appointments to discuss alternative pain management strategies or the need for opioid prescriptions. Help the individual follow up with medical providers if they have concerns about their prescription or dependence.
- Support Therapy and Counseling: Encourage the individual to seek counseling or therapy if there are concerns about opioid misuse or a history of substance use disorder. Family therapy can also be beneficial to address underlying emotional or relational issues contributing to the risk of addiction.
5. Offer Emotional Support
- Provide a Strong Emotional Foundation: A supportive family can offer reassurance, understanding, and a sense of security, reducing stress or anxiety that may contribute to opioid misuse.
- Acknowledge and Validate Feelings: Validate the emotions of individuals, especially those dealing with chronic pain, trauma, or emotional distress. Feeling heard and understood can reduce the reliance on substances as a coping mechanism.
6. Educate the Family
- Learn About Addiction and Risk Factors: Educate family members about addiction, the signs of opioid misuse, and how to recognize the early warning signs of dependence. This enables early intervention and practical support.
- Promote Coping Skills: Teach healthy ways to manage stress, anxiety, and pain. Families can model these skills and encourage the individual to use them as alternatives to substance use.
7. Create a Supportive Home Environment
- Minimize Triggers: Work together to reduce potential triggers that could lead to substance misuse. For example, if someone in the family struggles with addiction or misuse, it may be helpful to create physical or emotional distance from that person if they present a trigger for relapse.
- Encourage Positive Relationships: Surround the individual with positive, supportive relationships. Family members can encourage connections with sober peers, role models, or others who are committed to healthy lifestyles.
8. Foster Accountability
- Encourage Responsibility: Help the individual stay accountable by setting regular check-ins or discussing progress regarding pain management and opioid use. Encouraging responsibility for their health and choices can reinforce positive behavior.
- Celebrate Progress: Acknowledge and celebrate small victories, such as using non-opioid alternatives for pain management, attending therapy, or sticking to the prescribed medication plan. Positive reinforcement boosts confidence and reduces the risk of relapse.
9. Assist with Medication Management
- Monitor Medication Usage: Ensure that opioids are only taken as prescribed, with no misuse or diversion. Please keep track of when medications are dispensed and ensure they are only taken for the prescribed duration.
- Dispose of Unused Medications Properly: Help with the safe disposal of unused or expired medications to reduce the risk of misuse or theft.
10. Build a Support Network
- Seek Support for the Family: Families should take care of themselves, too. Participating in support groups such as Al-Anon or Nar-Anon can help family members understand addiction better, learn coping strategies, and find emotional support from others facing similar challenges.
- Encourage Social Support: Connecting the individual to sober communities or support groups like Narcotics Anonymous (NA) can provide them with ongoing encouragement, reducing the likelihood of turning to opioids in times of crisis.
Family support is essential in preventing opioid and opiate addiction. Through open communication, promoting healthy lifestyle choices, setting clear boundaries, and encouraging professional help, families can provide the foundation for a person to manage pain responsibly without falling into addiction. By staying educated, offering emotional support, and fostering accountability, families play a crucial role in both prevention and recovery.
Strengthening Communities: Strategies for Preventing Opioid and Opiate Addiction
Community resources play a vital role in preventing opioid and opiate addiction by providing education, support, and access to effective interventions. Through comprehensive strategies, communities can help individuals make informed choices, access treatment, and find long-term support. Below are key community-based strategies to prevent opioid addiction and promote overall well-being.
1. Public Education and Awareness Campaigns
- Informing the Public: Community programs should educate the public about the risks of opioid use, the signs of addiction, and the dangers of misuse. Local media campaigns, workshops, and school programs can help raise awareness.
- Targeted Outreach: High-risk groups, including individuals with chronic pain, veterans, and those with a history of substance abuse, benefit from targeted education on alternative pain management strategies and addiction risks.
2. Access to Pain Management Alternatives
- Non-Opioid Pain Relief Programs: Communities should offer alternatives such as physical therapy, acupuncture, cognitive behavioral therapy (CBT), and mindfulness-based stress reduction (MBSR).
- Collaboration with Healthcare Providers: Encouraging local healthcare professionals to recommend and provide non-opioid treatments can expand accessibility to safer pain management options.
3. Substance Use Education in Schools and Workplaces
- Preventive Education in Schools: Schools should implement evidence-based programs that teach students about opioid risks, healthy coping mechanisms, and how to resist peer pressure.
- Workplace Programs: Employers can educate employees on substance abuse prevention and offer support services, such as Employee Assistance Programs (EAPs), to address mental health and addiction concerns.
4. Community Support Groups
- Support Groups for Individuals: Organizations like Narcotics Anonymous (NA) and SMART Recovery provide safe spaces for individuals to share experiences, receive support, and develop coping strategies.
- Family Support Groups: Groups like Al-Anon and Nar-Anon help families understand addiction, develop coping mechanisms, and foster supportive home environments.
5. Medication-Assisted Treatment (MAT) Programs
- Access to MAT: MAT combines medications (methadone, buprenorphine, naltrexone) with counseling to treat opioid addiction effectively.
- Expanding MAT Availability: Increasing the number of clinics offering MAT can reduce treatment barriers and improve recovery outcomes.
6. Overdose Prevention and Naloxone Distribution
- Naloxone Access: Distributing naloxone to first responders, at-risk individuals, and families can save lives.
- Overdose Education: Community programs should teach individuals to recognize overdose signs and administer naloxone effectively.
7. Collaboration with Law Enforcement
- Reducing the Supply of Illicit Opioids: Law enforcement agencies should work with communities to curb illegal drug trafficking.
- Diversion Programs: Instead of incarceration, drug diversion programs can direct individuals toward rehabilitation and treatment services.
8. Prescription Drug Monitoring Programs (PDMPs)
- Monitoring Prescriptions: PDMPs track opioid prescriptions, identify potential misuse, and prevent doctor-shopping.
- Doctor and Pharmacist Training: Training healthcare professionals to recognize opioid misuse and prescribe safer alternatives is crucial.
9. Treatment and Recovery Services
- Access to Addiction Treatment: Communities should ensure accessible inpatient and outpatient rehab programs, detox services, and recovery support.
- Support for Long-Term Recovery: Sober living houses, vocational training, and mental health services help individuals maintain sobriety.
10. Community-Based Harm Reduction Programs
- Harm Reduction Services: Needle exchange programs, supervised injection sites, and substance use education can prevent overdoses and disease transmission.
- Safe Disposal of Opioid Medications: Encouraging the proper disposal of unused opioids helps prevent diversion and misuse.
11. Strengthening Community Networks
- Building a Supportive Community: Creating strong peer networks, mentorship programs, and community centers fosters a sense of belonging and reduces the risk of addiction.
- Access to Social Services: Housing support, employment assistance, and mental health care address underlying factors contributing to opioid misuse.
Community-based strategies are essential in preventing opioid and opiate addiction. By focusing on education, prevention, treatment, and harm reduction, communities can create a supportive environment that promotes health and recovery. With increased access to non-opioid pain management, prescription monitoring, and long-term recovery support, individuals at risk of addiction have the resources they need to make healthier choices and build a brighter future.
Frequently Asked Questions
Here are some common questions:
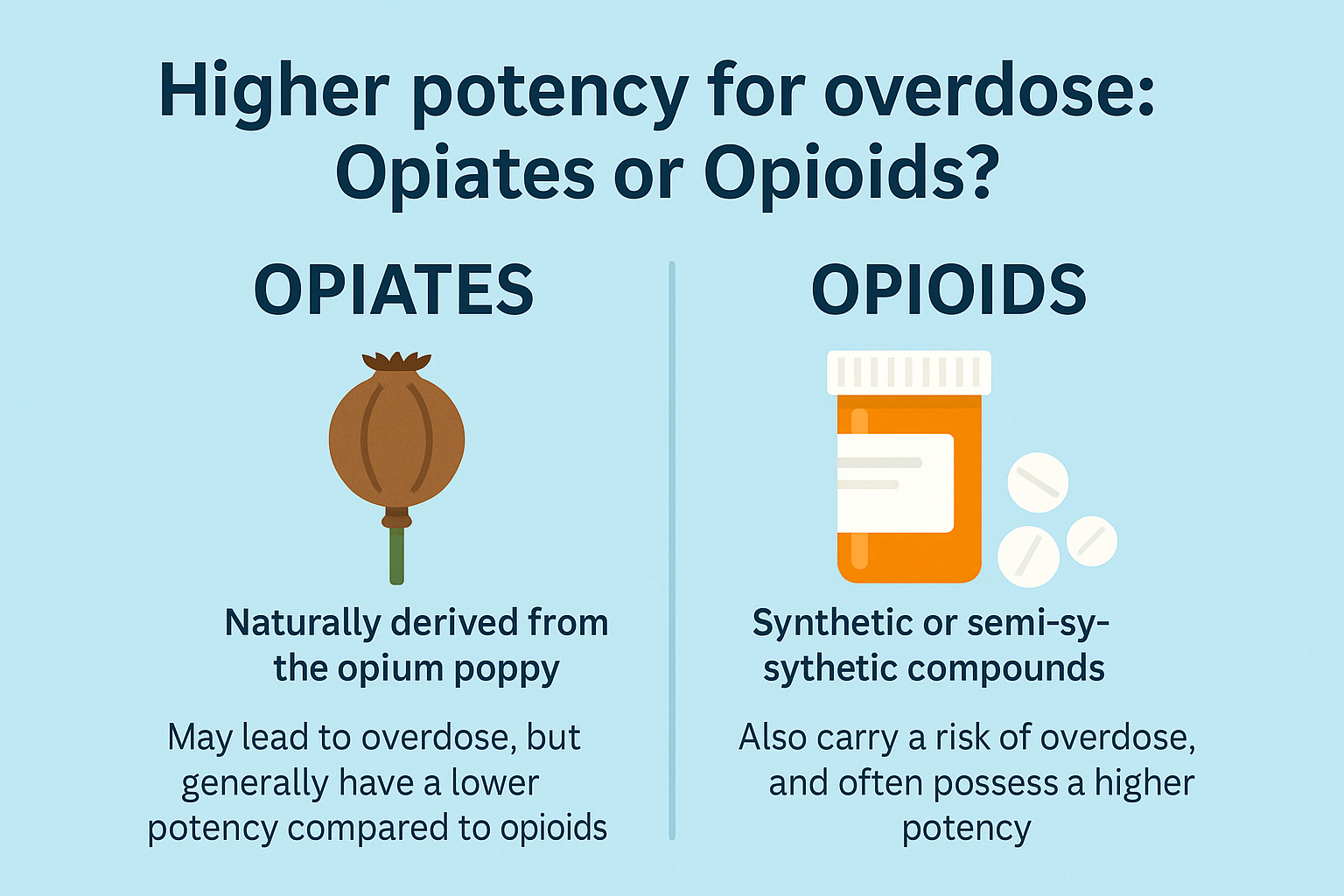
Question: Which has high potency for overdose, opiates or opioids?
Answer: Opioids generally have a higher potency for overdose than opiates. Here’s why:
- Opiates (e.g., morphine, codeine) are naturally derived from the opium poppy and have a limited potency range. While they can cause an overdose, they tend to be less potent than many synthetic opioids.
- Opioids (including synthetic and semi-synthetic versions like fentanyl, oxycodone, and heroin) can be significantly more potent. For example, fentanyl is up to 50-100 times more powerful than morphine and is a major driver of opioid-related overdoses.
Key Overdose Risk Factors:
- Synthetic opioids (like fentanyl and carfentanil) have an extremely high potency, meaning even small amounts can cause respiratory depression and overdose.
- Illicit opioids (e.g., heroin laced with fentanyl) pose a higher overdose risk because users may not know the potency.
- Mixing opioids with other depressants (like alcohol or benzodiazepines) greatly increases overdose potential.
While both opiates and opioids carry overdose risks, synthetic opioids (a subset of opioids) have the highest potency and overdose potential, especially fentanyl and its analogs.
Question: What government interventions to limit the use of opiates and opioids?
Answer: Governments have implemented various interventions to limit opiate and opioid usage, aiming to prevent misuse, addiction, and overdose deaths. These strategies include regulations on prescribing, public health initiatives, harm reduction programs, and law enforcement actions. Here are some key government interventions:
1. Prescription Regulations and Monitoring
- Prescription Drug Monitoring Programs (PDMPs): These state-run databases track opioid prescriptions to prevent “doctor shopping” and overprescription.
- CDC Guidelines for Prescribing Opioids: The U.S. Centers for Disease Control and Prevention (CDC) has issued guidelines recommending limits on opioid prescriptions for chronic pain.
- Mandatory Prescription Limits: Some states have enacted laws restricting the quantity and duration of opioid prescriptions, especially for acute pain.
- Mandatory Physician Training: Many governments require healthcare providers to undergo training on safe opioid prescribing and recognizing signs of addiction.
2. Law Enforcement and Drug Supply Control
- Regulating Pharmaceutical Companies: Lawsuits and regulations have targeted opioid manufacturers for misleading marketing and oversupply of opioids. Companies like Purdue Pharma have faced legal consequences.
- Restricting Opioid Production Quotas: Agencies like the U.S. Drug Enforcement Administration (DEA) set production limits on prescription opioids to reduce overall availability.
- Crackdowns on Illicit Drug Trafficking: Governments work to disrupt heroin and synthetic opioid (e.g., fentanyl) trafficking networks, including partnerships with international law enforcement.
- Regulating Online Pharmacies and Dark Web Sales: Efforts to shut down illegal online sales of opioids have increased.
3. Public Health and Harm Reduction Initiatives
- Naloxone Distribution Programs: Many governments provide naloxone (Narcan), an overdose-reversing drug, to first responders, healthcare workers, and at-risk individuals.
- Good Samaritan Laws: These laws protect individuals from legal consequences when seeking medical help for an overdose.
- Supervised Consumption Sites: Some countries and cities have introduced safe injection sites where people can use drugs under medical supervision to prevent overdoses.
- Needle Exchange Programs: These programs help prevent the spread of diseases like HIV and hepatitis while connecting users to treatment services.
4. Expanding Access to Addiction Treatment
- Medication-Assisted Treatment (MAT) Programs: Governments support access to medications like methadone, buprenorphine, and naltrexone for opioid addiction.
- Funding for Rehabilitation Services: Increased investment in addiction treatment centers, including inpatient and outpatient rehab programs.
- Integration of Behavioral Health Services: Expanding mental health and counseling services to address the underlying causes of addiction.
5. Public Awareness and Prevention Campaigns
- Educational Programs in Schools: Teaching youth about the dangers of opioid misuse and alternative pain management strategies.
- Community Awareness Campaigns: Public service announcements and campaigns (e.g., “The Truth About Opioids”) educate people on addiction risks and treatment options.
- Employer and Workplace Training: Programs aimed at helping businesses recognize and address opioid misuse among employees.
6. Legal and Policy Reforms
- Decriminalization and Diversion Programs: Some jurisdictions focus on treating opioid addiction as a health issue rather than a criminal offense, offering treatment instead of jail time.
- Expanding Medicaid and Insurance Coverage: Increasing access to addiction treatment services through government-funded healthcare programs.
- Research and Development for Non-Opioid Pain Management: Funding research into alternative pain relief methods, such as physical therapy, acupuncture, and non-addictive medications.
Government interventions to limit opioid and opiate use involve a multi-pronged approach that includes regulation, law enforcement, harm reduction, treatment expansion, and public education. The goal is to prevent new cases of addiction while providing support for those affected. The most effective strategies often combine strict prescription control with accessible treatment and harm reduction measures to balance public health and safety.
Question: How does Narcan work to reverse the effects of opiate and opioids?
Answer: Narcan (naloxone) is an opioid antagonist that rapidly reverses the effects of opioid overdose, including life-threatening respiratory depression. Here’s how it works:
1. Mechanism of Action
- Opioids (such as heroin, fentanyl, and oxycodone) bind to opioid receptors in the brain, slowing breathing and causing sedation.
- Naloxone competes with opioids by binding to the same opioid receptors but without activating them. This displaces opioids from the receptors, blocking their effects.
- Since naloxone has a stronger affinity for opioid receptors than most opioids, it can rapidly reverse overdose symptoms within minutes.
2. Effects on the Body
- Restores Breathing: The primary danger of opioid overdose is respiratory depression (slow or stopped breathing). Narcan restores normal breathing within 2-3 minutes.
- Reverses Sedation & Unconsciousness: It can quickly wake up an unconscious person experiencing an overdose.
- Triggers Withdrawal Symptoms: Because it rapidly removes opioids from the receptors, it can cause sudden withdrawal symptoms, such as nausea, sweating, agitation, and muscle pain.
3. Administration Methods
- Nasal Spray (Narcan): A single-dose, easy-to-use spray administered into one nostril.
- Injection (Intramuscular or Intravenous): Healthcare professionals may administer naloxone by injection to achieve faster effects.
- Auto-Injector (Evzio): A prefilled device that delivers a set dose with voice-guided instructions.
4. Limitations & Considerations
- Short Duration: Naloxone works for 30–90 minutes, but some opioids (especially fentanyl) last longer, so multiple doses may be needed.
- Not a Cure: It reverses an overdose temporarily but does not treat opioid addiction. Medical attention is still required.
- No Effect on Non-Opioid Overdose: Naloxone only works on opioid-related overdoses; it does not counteract other drugs like benzodiazepines or alcohol.
5. Availability & Access
- In many places, Narcan is available without a prescription and distributed to first responders, harm reduction programs, and individuals at risk of overdose.
- Good Samaritan Laws often protect individuals who administer naloxone in an emergency.
Narcan saves lives by quickly reversing opioid overdoses and restoring normal breathing. However, it is not a substitute for medical treatment or addiction recovery. After naloxone administration, emergency medical help should always be sought to ensure long-term safety.
Conclusion
While opioids and opiates differ in their origin, both share similar addictive properties due to their impact on the brain’s reward system, making them highly prone to misuse and dependence. Effective management of addiction involves self-management strategies like exploring non-opioid alternatives and adhering to prescribed treatments. Family support plays a key role by offering emotional assistance, fostering communication, and guiding individuals toward professional help. Additionally, community resources, such as education, treatment services, and support groups, are vital in providing the tools and support needed to prevent and overcome opioid and opiate addiction. Together, these approaches form a comprehensive strategy for addressing this widespread issue.
Videos: Opiates vs Opioids The REAL Difference EXPLAINED
The DEADLY Truth About Natural Opiates vs Synthetic Opioids
Video: