Veterans working through recovery often face tough challenges, especially when unexpected triggers show up and threaten to throw everything off course. These nightmare triggers aren’t always obvious, but can pull the rug out from under steady progress. I’ve learned how surprising and powerful these triggers can be, so understanding what they are and how they work is super important for anyone who wants to support veterans or steer them through recovery themselves.
What Makes a Trigger for Veterans?
For a lot of veterans, triggers are deeply personal. They can be anything that causes old memories, emotions, or physical sensations to rush back. Sometimes these triggers are tied to trauma or challenging experiences from service, but they often show up in day-to-day life without much warning. A trigger might bring about cravings, flashbacks, or intense emotions, making it challenging to stay on the recovery path. Everyone’s situation is different, so what trips one person up might not even register to someone else.
Statistics from the U.S. Department of Veterans Affairs show that PTSD, depression, and substance use disorders often go together for veterans. Spotting these triggers is vital in preventing setbacks and building long-lasting recovery.
Common Nightmare Triggers That Lead Veterans to Relapse
Triggers can sneak up from different directions, especially during vulnerable moments. Here are some of the more common nightmare triggers I’ve seen, plus what makes them so tough to handle:
- Anniversaries of Difficult Events: Dates with emotional weight, like the day of a deployment or tragic loss, can stir up tough memories.
- Loud Noises or Sudden Sounds: Fireworks, construction, or sirens can return memories from combat or active service.
- Isolation: Feeling separated from friends and family can set off feelings of loneliness, making cravings worse.
- Conflict at Home or Work: Arguments or stressful interactions can overwhelm the coping tools built in recovery.
- Certain Smells or Sights: Scents like diesel fuel, bonfires, or certain foods can trigger flashbacks or strong emotions.
- Change in Routine: Moving, switching jobs, or even traveling can shake up the structure that helps keep recovery on track.
A small detail can make all the difference; it doesn’t always take a big event to send someone reeling. Wanting to steer clear of triggers is normal, but knowing how to face them can be more helpful in the long run. In fact, simply preparing for triggers can grow your confidence in recovery.
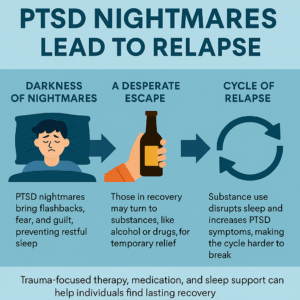
How Triggers Turn Into Relapse
When a trigger sets off anxiety, anger, or loneliness, old ways of coping might start looking tempting again. For some, this means falling back into substance use or unhealthy habits. I’ve seen how triggering experiences can snowball quickly: a loud noise on July 4th leads to poor sleep, which leads to high stress during the workday, and pretty soon, the urge to use or pick up old habits can feel impossible to fight off.
The chain reaction often goes like this. A trigger shows up, routine strategies stop working as well, negative thinking ramps up, and before long, relapse feels like the only way out. That’s why it’s so important to have tools ready to handle all kinds of triggers and be comfortable reaching out for help when things get rough. Sometimes, talking through a trigger as soon as it hits can keep everything from snowballing.
Warning Signs: Noticing When You’re Headed for Trouble
Some veterans learn to spot the early warning signs that show up before a full-blown relapse. Others catch the signals only after the fact. Here are a few red flags that could mean a nightmare trigger is building up:
- Changes in Mood: More irritability, anger, sadness, or anxiety than usual.
- Poor Sleep Patterns: Trouble falling asleep or staying asleep right after an upsetting memory or trigger.
- Withdrawing from Support: Skipping out on meetings, dropping off from group chats, or pulling away from close friends.
- Obsessive Thoughts: Playing the same memory repeatedly, fixating on the past, or racing thoughts about the trigger.
- Routine Falling Apart: Schedules are chaotic, essential tasks are forgotten, or self-care is neglected.
Getting real about these warning signs isn’t always easy, but checking in on how you feel daily is a great way to prevent a relapse. Writing down moods and thoughts in a journal can help you track these warning signs and stay aware.
Common Barriers That Make Triggers Harder to Handle
Handling triggers involves more than just willpower. Several significant challenges can catch veterans off guard and make relapse more likely when triggers show up:
- Stigma: Many people avoid sharing what’s happening because they fear being judged or misunderstood. The fear of seeming “weak” can also prevent someone from asking for support, even when it is badly needed.
- Limited Access to Care: Not everyone has a VA hospital or counselor nearby, especially in rural areas. Some veterans may feel cut off from real help, even if ready to reach out.
- Self-blame: It’s easy to blame yourself for slipping up. This can cause problems to snowball instead of getting better, creating a negative feedback loop.
- Lack of Understanding by Family or Friends: Not everyone understands how a harmless event can feel like a crisis for a veteran. Sometimes, triggers seem minor to others but pack a huge emotional punch.
Facing these barriers head-on often means asking for help, finding peer support, or learning how to explain to others what these triggers really feel like. Communication with your team or loved ones can smooth the way during high-stress moments.
Practical Ways to Manage or Prevent Nightmare Triggers
No one can sidestep every trigger, but plenty of strategies can help manage them. I’ve picked up a few that seem to work for many veterans:
- Build a Strong Support Network: Regularly talking with other veterans, a counselor, or family members helps you spot tricky times before they get worse.
- Practice Grounding Techniques: Simple things like focusing on your breathing or touching something cold can release the grip of panic or flashbacks and bring you back into the present.
- Stick to a Routine: A predictable schedule makes it easier to get through stressful days without falling into old patterns. Routine gives a sense of control when everything else feels unpredictable.
- Use Journaling: Writing out thoughts and feelings after a trigger helps you process what happened and figure out how to cope better next time. It can also help you spot trends in what types of triggers are the toughest.
- Prepare for Anniversaries and High-Stress Times: Look ahead and plan extra support for tough days. Mark them on a calendar and let trusted friends know when you need a backup.
- Get Professional Help When Needed: Reaching out for therapy, medication, or support groups doesn’t mean you failed. It can keep small triggers from piling up and triggering major setbacks later.
Organizations like the Veterans Crisis Line and the PTSD VA offer more resources and coping techniques. These places are worth bookmarking for anyone in recovery or supporting someone who is. They offer guides, helplines, and groups that can give a boost when things get rough.
Challenges Veterans Face, and Real-World Coping Strategies
Life after service has a lot of ups and downs, especially during recovery. I’ve heard from veterans who say the civilian world brings challenges, like feeling out of place at events or bumping into reminders from the past at places they least expect. Recovery is never a one-size-fits-all adventure. Here are some strategies that veterans have shared with me that could be worth trying:
- Peer Groups: Local or online veteran support groups can be game changers. Hearing from people with similar experiences can help you feel less alone. Sometimes, a simple message from a peer group can change your outlook.
- Mindfulness and Meditation: Spending a few minutes daily focusing on breathing or listening to relaxing sounds can lower anxiety and help you stay centered.
- Pets: Some veterans find comfort and emotional grounding in caring for a pet. Pets offer routine, responsibility, and unconditional companionship.
- Creative Outlets: Art, music, writing, or working with your hands can be safe ways to process triggers outside of talking. Making something with your hands can focus your thoughts on the present.
- Physical Activities: Exercise, hiking, or yoga help reset the mind and provide a healthy way to handle stress or restless energy. Moving your body is an underrated way to break a stress cycle.
Combining a few of these ideas may help some veterans build resilience against nightmare triggers and find more peace in their daily lives. There’s no wrong way to use these strategies; the key is steady practice and seeing what works best for you. New hobbies or skills picked up during recovery can also add meaning and structure when things get rocky.
Frequently Asked Questions
Here are some common questions I hear from veterans and their families about nightmare triggers and relapse:
What are some warning signs that a veteran is about to relapse?
Answer: Mood changes, increased isolation, disrupted sleep, and dropping old routines are common signs. Checking in early with a buddy or counselor can make a big difference.
Can families help prevent triggers from causing a relapse?
Answer: Absolutely. Offering nonjudgmental support, learning about common triggers, and keeping communication open all help veterans feel safer talking things out.
Are there resources for veterans dealing with tough triggers?
Answer: Yes, organizations like the Veterans Crisis Line and VA PTSD program have hotlines, therapy, and group options. Local VFWs and online veteran communities are great places to start when seeking support and information.
Key Takeaways for Veterans and Supporters
Nightmare triggers can challenge even the strongest recovery. Recognizing what they are and how they work is a solid step in handling them. Having a support network, a daily routine, and some backup strategies ready can make those challenging moments more manageable. You’re definitely not alone. Help is out there; sometimes, talking to someone who gets it can turn the whole day around. The path of recovery is an adventure filled with small wins, setbacks, and unexpected turns. Still, with the proper support and preparation, every veteran can build a life that feels steady and meaningful.
Video: Why Nightmares Make Recovery So Hard