Naltrexone and Ozempic take different approaches to treating alcohol use disorder (AUD). Naltrexone is FDA-approved, affordable, and well-studied; Ozempic is promising but off-label, costly, and less researched. Ethical concerns include access, safety, and informed consent. Both have side effects, and choosing between them reflects the trade-off between innovation and proven care.
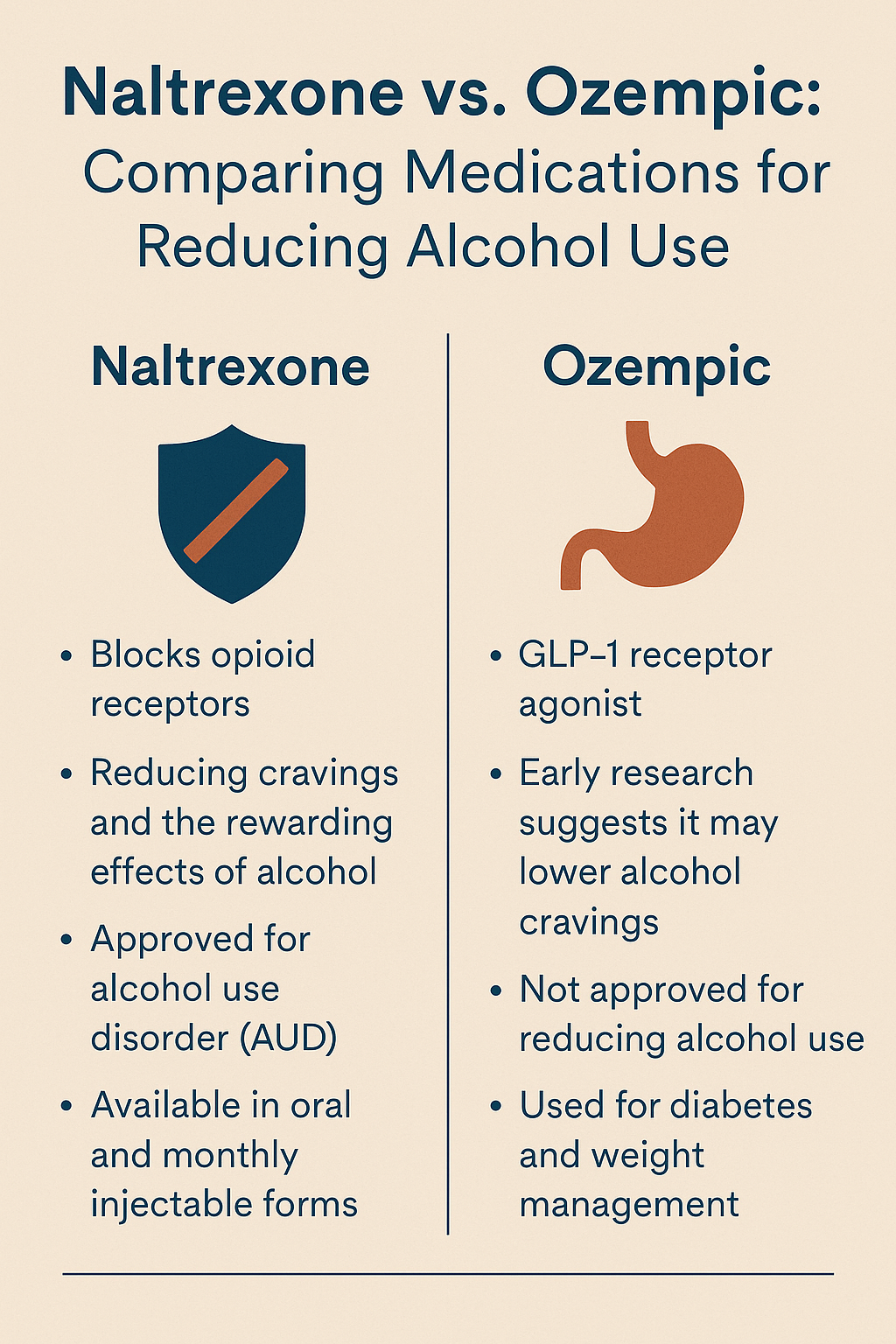
Naltrexone vs. Ozempic: Comparing Medications for Reducing Alcohol Use
Naltrexone and Ozempic (semaglutide) are both gaining attention for their roles in reducing alcohol consumption. Still, they differ significantly in how they work, their approval status, and the strength of supporting evidence.
🔬 Mechanism of Action
Naltrexone is FDA-approved for Alcohol Use Disorder (AUD). It works by blocking opioid receptors in the brain’s reward system, reducing the pleasurable effects of alcohol and cravings.
Ozempic, a GLP-1 receptor agonist approved initially for type 2 diabetes and weight loss, may influence alcohol intake by modulating dopamine signaling and satiety mechanisms—though this remains under study.
📊 Effectiveness in Reducing Alcohol Consumption
- Naltrexone has robust evidence from multiple large-scale trials, showing moderate effectiveness in reducing cravings and heavy drinking—especially in those with reward-driven patterns.
- Ozempic is still in the experimental stage for AUD, with promising results from animal models and early human case reports. Large clinical trials are ongoing.
⚖️ Side Effects & Considerations
- Naltrexone side effects include nausea, dizziness, and elevated liver enzymes. It is contraindicated in individuals with liver failure or those on opioid medications.
- Ozempic may cause gastrointestinal issues like nausea and diarrhea, and rare risks like pancreatitis. Its use for AUD is off-label, and access may be limited without a qualifying diagnosis like diabetes or obesity.
🔒 Regulatory Status
- Naltrexone: ✅ FDA-approved for treating AUD; part of standard medication-assisted treatment.
- Ozempic: ❌ Not approved for AUD; current use is experimental and limited to research contexts.
🧠 Summary
- Naltrexone is a well-established, first-line treatment for AUD—especially effective in people with intense cravings or binge-drinking behaviors.
- Ozempic shows early promise and may eventually be part of alcohol treatment options, particularly for individuals with metabolic conditions or poor impulse control. However, it is not yet an approved or proven treatment for AUD.
As research evolves, understanding the differences between these medications is essential for choosing the right strategy in treating alcohol use disorder.
Ethical Dilemmas in Using Naltrexone vs. Ozempic for Treating Alcohol Use Disorder
As interest grows in using Ozempic (semaglutide) to manage Alcohol Use Disorder (AUD), ethical concerns are emerging—particularly when compared to the established use of Naltrexone. These two medications differ not only in clinical status but also in how they raise questions around off-label use, equity, consent, and the evolving landscape of addiction treatment. Here’s a breakdown of key ethical considerations.
⚖️ Ethical Dilemmas: Naltrexone vs. Ozempic for AUD
1. 🧪 Evidence vs. Innovation
- Naltrexone is FDA-approved and backed by decades of research.
- Ozempic is off-label for AUD with minimal human data.
- Ethical dilemma: Is it responsible to offer an unapproved but promising treatment when an approved one already exists?
Key principles: Beneficence, Non-maleficence, Evidence-based care
2. 🧾 Informed Consent
- Patients prescribed Naltrexone can rely on well-established information.
- Ozempic users may not fully grasp that they’re part of an unproven treatment space.
- Ethical dilemma: Can proper informed consent be given without long-term data?
Key principles: Autonomy, Truthfulness (Veracity)
3. 💰 Equity and Access
- Naltrexone is low-cost and widely accessible.
- Ozempic is expensive and often not covered for addiction treatment.
- Ethical dilemma: Could access to Ozempic create new inequalities in addiction care?
Key principles: Justice, Distributive fairness
4. 💉 Prioritization and Misuse
- Off-label demand for Ozempic may limit availability for patients with diabetes.
- Ethical dilemma: Should access for AUD be limited until clinical evidence justifies broader use?
Key principles: Resource stewardship, Justice
5. 🧍♂️ Stigma and Labeling
- Naltrexone is often stigmatized due to its link with addiction treatment.
- Ozempic, associated with weight loss, may reduce stigma or mask addiction issues.
- Ethical dilemma: Does off-label use reduce stigma or dangerously blur diagnostic clarity?
Key principles: Respect for persons, Social justice
6. 🔄 Coercion in Vulnerable Populations
- People struggling with addiction may feel pressured to try unapproved treatments.
- Ethical dilemma: How can we ensure patients aren’t coerced into novel therapies, especially in mandated care settings?
Key principles: Autonomy, Protection of vulnerable populations
7. 📈 Promotion vs. Clinical Judgment
- Pharmaceutical influence could encourage premature adoption of Ozempic for addiction.
- Ethical dilemma: Should providers lead with caution or innovation?
Key principles: Professional integrity, Primum non nocere (no harm)
✅ Recommendations for Ethical Practice
- Provide explicit, transparent informed consent for off-label uses.
- Prioritize evidence-based care—begin with approved, accessible medications.
- Use shared decision-making tools to help patients weigh risks and goals.
- Advocate for research, insurance reform, and ethical pathways to expand future treatment options.
In summary, while Ozempic holds potential for treating alcohol use disorder, its ethical use must be grounded in transparency, fairness, and scientific rigor. Until further evidence emerges, Naltrexone remains the more ethical first-line option for most patients—ensuring both effectiveness and equity in care.
Naltrexone vs. Ozempic: A Side-by-Side Look at Side Effects and Use for Alcohol Use Disorder
💊 Naltrexone
Naltrexone is FDA-approved for treating both alcohol and opioid use disorders and has been in clinical use for decades.
🔄 Common Side Effects:
- Nausea
- Headache
- Dizziness
- Fatigue
- Insomnia
- Anxiety or restlessness
- Abdominal cramps
⚠️ Serious or Rare Side Effects:
- Liver toxicity (especially at higher doses)
- Injection site reactions (for long-acting injectable)
- Precipitated opioid withdrawal (if opioids are present in the system)
- Depression or suicidal thoughts (rare but documented)
💡 AUD-Specific Consideration:
Effective for reducing cravings and relapse in individuals with reward-driven alcohol use. Requires patients to be opioid-free before starting to prevent dangerous withdrawal.
💊 Ozempic (Semaglutide)
Originally developed and approved for type 2 diabetes and obesity, Ozempic is now being explored for its potential impact on alcohol consumption.
🔄 Common Side Effects:
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Stomach pain
- Decreased appetite
- Fatigue
⚠️ Serious or Rare Side Effects:
- Pancreatitis
- Gallbladder issues
- Kidney injury from dehydration
- Thyroid tumors (noted in animal studies; black box warning)
- Hypoglycemia (when combined with other diabetes medications)
- Possible mood changes (still being studied)
💡 AUD-Specific Consideration:
Appetite and reward suppression may help reduce cravings, but they could also worsen mood or nutritional status in people vulnerable to depression or eating disorders.
🔍 Side-by-Side Summary Table
| Feature | Naltrexone | Ozempic |
|---|---|---|
| Primary Use | Alcohol & opiod use disorder | Diabetes, weight loss |
| FDA-Approved for AUD? | ✅ Yes | ❌ No (off-label use) |
| Craving Reduction | Proven moderate effect | Early, unproven evidence |
| Common Side Effects | Nausea, headache, insomnia | GI issues, fatigue |
| Serious Risks | Liver toxicity, opioid withdrawal | Pancreatitis, thyroid tumors |
| Cost/Insurance | Low, widely covered | High, limited coverage |
| Contraindications | Liver failure, active opioid use | Thyroid cancer, GI conditions |
🧠 Key Takeaways
- Naltrexone remains the gold-standard medication for AUD, with well-documented benefits, especially for individuals with cravings or binge patterns. However, it carries risks for those with liver problems and cannot be used with opioids.
- Ozempic presents a novel but experimental option for AUD, with more gastrointestinal and metabolic risks. Its effect on alcohol intake remains under clinical investigation.
- Treatment choice should reflect each patient’s clinical profile, preferences, risk factors, and overall treatment goals. Until more evidence emerges, Naltrexone remains the safer and more ethical first-line option.
As research evolves, these insights will help both patients and providers make informed, individualized treatment decisions.
Cost Comparison: Naltrexone vs. Ozempic for Alcohol Use Disorder
The cost gap between Ozempic and Naltrexone is substantial, shaped by factors such as patent protection, insurance coverage, and the availability of generics. While both are being explored for reducing alcohol use, their price points make a significant difference in real-world accessibility.
💰 Cost Comparison: Naltrexone vs. Ozempic (U.S. Prices)
| Medication | Formulation | Typical Cash Price (Monthly) | Insurance Coverage | Generic Available? |
|---|---|---|---|---|
| Naltrexone | 50 mg oral tablet (daily) | $25–$80 | Widely covered | ✅ Yes |
| 380 mg injection (monthly) | $1,200–$1,500 | Often covered with prior authorization | ✅ Yes (but still costly) | |
| Ozempic | 0.25–2.0 mg weekly injection | $800–$1,200 | Often limited unless prescribed for diabetes/obesity | ❌ No |
🔎 Key Considerations
💊 Naltrexone
- Oral tablets are affordable, even without insurance.
- The injectable version is costly but frequently covered when medically indicated.
- FDA-approved for AUD, making insurance coverage much more likely.
💊 Ozempic (Semaglutide)
- Branded only: No generic available.
- Not FDA-approved for Alcohol Use Disorder (AUD), so off-label use is rarely covered.
- High out-of-pocket costs unless prescribed for approved indications like diabetes or obesity.
🧠 Bottom Line
- Ozempic is 10–40 times more expensive than oral Naltrexone.
- Naltrexone remains the more cost-effective and accessible choice for most people with alcohol use disorder.
- Ozempic may only be practical in research contexts or for patients with overlapping conditions like type 2 diabetes or obesity.
For now, Naltrexone is the more ethical, evidence-based, and financially sustainable choice—while Ozempic’s role in addiction treatment continues to be studied.
Frequently Asked Questions
Here are some common questions:
Question: How did Ozempic become the AUD choice?
Answer:
Ozempic (semaglutide) was never designed initially or approved to treat Alcohol Use Disorder. However, its emergence as a potential off-label treatment for AUD is rooted in a combination of scientific curiosity, serendipitous observations, and promising early data. Here’s how Ozempic became a surprising contender in addiction treatment:
🔍 1. GLP-1 Mechanisms and Brain Reward Pathways
Ozempic is a GLP-1 receptor agonist, a class of drugs primarily used to manage type 2 diabetes and obesity. But GLP-1 receptors are also found in key brain regions that regulate reward, motivation, and craving—the same circuits involved in substance use disorders. Researchers began to suspect that these medications might blunt dopamine-driven behaviors, including those tied to alcohol and other substances.
🧪 2. Animal Studies Showed Reduced Alcohol Intake
Early preclinical studies in rodents found that GLP-1 agonists reduced:
- Alcohol consumption
- Alcohol-seeking behavior
- Relapse-like behavior
This opened the door to exploring these effects in humans.
📉 3. Weight Loss Patients Report Drinking Less
Anecdotal reports began to emerge—patients prescribed Ozempic for weight loss or diabetes reported:
- Less desire to drink
- Reduced alcohol intake
- Even aversions to alcohol in some cases
These informal observations sparked interest among addiction researchers and clinicians.
👩⚕️ 4. Early Human Case Reports & Small Studies
Small pilot studies and case reports soon followed, suggesting that some individuals taking semaglutide or similar drugs experienced:
- Reduced cravings for alcohol
- Lower alcohol consumption, even without specific counseling
- Improved impulse control or mood stabilization
While not yet large-scale, these early signals generated excitement about a new pharmacologic pathway.
📚 5. Clinical Trials Now Underway
As of 2024–2025, several clinical trials are actively studying GLP-1 medications (including semaglutide and liraglutide) for alcohol and substance use disorders. One example:
- NCT05800241 – a trial specifically evaluating semaglutide’s impact on alcohol intake.
These trials aim to determine whether the early promise holds up under rigorous testing.
⚖️ 6. Why It’s Still Experimental
Despite the buzz, Ozempic:
- It is not FDA-approved for AUD
- Lacks large-scale, controlled human trials for this use
- Carries a high cost and access limitations for off-label prescribing
Thus, it remains a research-based or experimental option, not a frontline treatment.
In summary, Ozempic became a candidate for treating Alcohol Use Disorder through a unique convergence of neuroscience, patient reports, and curiosity-driven research. Its ability to regulate brain reward systems and reduce compulsive behaviors makes it an exciting—yet still unproven—tool. For now, Naltrexone remains the gold standard for AUD, but Ozempic may become part of the next generation of addiction treatments, pending further evidence.
Question: What other medications are considered to be used for AUD?
Answer:
In addition to Naltrexone and investigational interest in Ozempic (semaglutide), there are several medications currently used, approved, or being studied for Alcohol Use Disorder (AUD). They fall into three categories:
✅ FDA-Approved Medications for AUD
- Naltrexone (oral & extended-release injectable)
- How it works: Blocks opioid receptors to reduce alcohol’s pleasurable effects and cravings.
- Best for: People with intense cravings or binge drinking behavior.
- Acamprosate (Campral)
- How it works: Modulates glutamate and GABA to reduce post-acute withdrawal symptoms and stabilize mood.
- Best for: People who have already stopped drinking and want to maintain abstinence.
- Disulfiram (Antabuse)
- How it works: Blocks the enzyme that breaks down alcohol, causing a severe reaction if alcohol is consumed.
- Best for: Highly motivated individuals aiming for complete abstinence.
🧪 Off-Label or Emerging Medications
These drugs are not FDA-approved for AUD but are used off-label or under study due to observed benefits.
- Topiramate
- Use: Seizures, migraines
- AUD effect: Reduces cravings, especially in those with heavy drinking patterns
- Drawbacks: Cognitive side effects (e.g., memory problems, drowsiness)
- Gabapentin
- Use: Seizures, nerve pain, anxiety
- AUD effect: Helps with withdrawal symptoms, cravings, and sleep issues
- Best for: People with anxiety, insomnia, or mild withdrawal
- Baclofen
- Use: Muscle relaxant
- AUD effect: May reduce cravings and anxiety
- Best for: People with liver issues (safe in hepatic impairment)
- Varenicline (Chantix)
- Use: Smoking cessation
- AUD effect: Reduces alcohol consumption in some studies, possibly via dopamine modulation
- Ondansetron
- Use: Nausea (5-HT3 antagonist)
- AUD effect: May reduce cravings in early-onset or genetically predisposed AUD
- Best for: Early-onset AUD and those with specific genetic profiles (e.g., 5-HT3 variants)
🌱 Experimental & Future Candidates (Early Research)
- GLP-1 Agonists (e.g., Semaglutide, Liraglutide)
- Suppress appetite and modulate reward circuits
- Under clinical trials for reducing alcohol use
- Psilocybin (psychedelic therapy)
- Promising in small trials for promoting insight and behavior change
- Ketamine + Psychotherapy
- May reduce cravings and promote emotional flexibility during early recovery
- Neurosteroids (e.g., ganaxolone)
- Target GABAergic pathways involved in alcohol dependence
- Ibudilast
- An anti-inflammatory phosphodiesterase inhibitor under investigation for AUD and stimulant use
🧠 Summary Chart
| Medication | FDA-Approved for AUD? | Primary Effect | Best Use Case |
|---|---|---|---|
| Naltrexone | ✅ Yes | Reduces cravings/reward | Binge/craving drinkers |
| Acamprosate | ✅ Yes | Maintains abstinence | Post-detox mood stabilization |
| Disulfiram | ✅ Yes | Aversion therapy | Abstinence-focused individuals |
| Topiramate | ❌ No | Craving reduction | Heavy drinkers, not sensitive to side effects |
| Gabapentin | ❌ No | Withdrawal/craving/sleep aid | Anxious/insomniac or early recovery |
| Baclofen | ❌ No | Craving/anxiety reduction | Liver disease or co-occurring anxiety |
| Semaglutide | ❌ No | Appetite/reward modulation | Under research—co-occurring obesity/impulsivity |
| Varenicline | ❌ No | Reward system modulation | Smokers or those with dual addiction |
Question: What other medications affect the key brain regions that regulate reward, motivation, and craving to manage addiction?
Answer:
There are several medications—both approved and experimental—that target key brain regions involved in reward, motivation, and craving to help manage addiction. These regions include the mesolimbic dopamine system, the prefrontal cortex, the amygdala, and the nucleus accumbens, among others.
Below is a breakdown of primary brain targets and the medications that act on them, organized by mechanism and addiction type.
🧠 Key Brain Regions in Addiction
| Brain Region | Role in Addiction |
|---|---|
| Nucleus Accumbens | Reward, reinforcement, and pleasure |
| Ventral Tegmental Area (VTA) | Dopamine production; initiation of reward signaling |
| Prefrontal Cortex | Decision-making, impulse control |
| Amygdala | Emotion, stress, fear, and relapse |
| Hippocampus | Memory triggers associated with substance use |
💊 Medications That Target These Pathways
1. Dopamine Modulators
These drugs influence dopamine release or receptor activity—directly tied to reward and motivation.
| Medication | Action | Used For |
|---|---|---|
| Bupropion | Dopamine/norepinephrine reuptake inhibitor | Smoking cessation, stimulant cravings |
| Varenicline | Partial nicotinic agonist → modulates dopamine | Nicotine, alcohol (off-label) |
| Amantadine | Increases dopamine release | Cocaine use (limited evidence) |
| L-DOPA / Pramipexole | Dopamine agonists (experimental) | Stimulant use (in trials) |
2. Opioid System Modulators
Block the opioid receptors that enhance the effects of alcohol and drugs.
| Medication | Action | Used For |
|---|---|---|
| Naltrexone | Mu-opioid receptor antagonist | Alcohol, opioids |
| Nalmefene | Similar to naltrexone, longer-acting | Alcohol (Europe) |
| Buprenorphine | Partial opioid agonist | Opioid Use Disorder |
| Methadone | Full opioid agonist (regulated) | Opioid Use Disorder |
3. GABA and Glutamate Modulators
These neurotransmitters help balance excitatory and inhibitory signaling in reward and stress pathways.
| Medication | Action | Used For |
|---|---|---|
| Acamprosate | Modulates glutamate-GABA balance | Alcohol Use Disorder |
| Topiramate | Inhibits glutamate, enhances GABA | Alcohol, cocaine (off-label) |
| Gabapentin | Enhances GABA, reduces excitability | Alcohol withdrawal, cravings |
| Baclofen | GABA-B agonist | Alcohol, cocaine (off-label) |
| Memantine | NMDA antagonist (experimental) | Alcohol, stimulant cravings |
4. Serotonin Modulators
Target mood, impulse control, and craving.
| Medication | Action | Used For |
|---|---|---|
| SSRIs (e.g., fluoxetine) | Increase serotonin | AUD with depression/anxiety |
| Ondansetron | 5-HT3 antagonist | Early-onset alcoholism (off-label) |
| Buspirone | 5-HT1A partial agonist | Anxiety, cocaine/alcohol (studied) |
5. GLP-1 Receptor Agonists
Affect satiety and reward circuits.
| Medication | Action | Used For |
|---|---|---|
| Semaglutide (Ozempic) | GLP-1 agonist → affects dopamine | Under study for AUD, obesity |
| Liraglutide | Same class as semaglutide | AUD, nicotine (research stage) |
6. Anti-Inflammatory / Neuroimmune Modulators
Chronic substance use causes neuroinflammation, which may fuel craving and relapse.
| Medication | Action | Used For |
|---|---|---|
| Ibudilast | Phosphodiesterase inhibitor → reduces neuroinflammation | Alcohol, opioids, meth (in trials) |
| Minocycline | Antibiotic with anti-inflammatory effects | Cocaine, opioids (experimental) |
| N-acetylcysteine (NAC) | Glutamate modulator, antioxidant | Cannabis, cocaine, gambling (mixed results) |
7. Psychedelic-Assisted Therapies
Act on serotonin and the default mode network, potentially “resetting” reward systems.
| Substance | Action | Used For |
|---|---|---|
| Psilocybin | 5-HT2A receptor agonist | Alcohol, smoking, depression (clinical trials) |
| Ketamine | NMDA antagonist → neuroplasticity | Alcohol, cocaine, depression |
| Ibogaine | Modulates multiple neurotransmitters | Opioid, alcohol, stimulant withdrawal (not FDA-approved) |
🧠 Summary: Therapeutic Targets & Their Tools
| Target Pathway | Example Medications |
|---|---|
| Dopamine (Reward) | Bupropion, Varenicline, Amantadine |
| Opioid receptors | Naltrexone, Buprenorphine, Methadone |
| GABA/Glutamate Balance | Acamprosate, Gabapentin, Topiramate |
| Serotonin Modulation | Ondansetron, SSRIs, Psilocybin |
| Inflammatory Pathways | Ibudilast, NAC, Minocycline |
| GLP-1 and Satiety | Semaglutide, Liraglutide |
Conclusion
While both Ozempic and Naltrexone show potential in managing alcohol use disorder, they differ significantly in approval status, cost, and clinical evidence. Naltrexone remains the more accessible and validated option, whereas Ozempic’s use is experimental, costly, and ethically complex due to its off-label nature. Each presents unique side effects and risks that must be carefully weighed. As research continues, treatment decisions should be guided by clinical need, patient safety, affordability, and ethical prescribing practices to ensure equitable and effective care.
Video: Can Naltrexone and Ozempic REALLY Help You Stop Drinking for Good