Polydrug use—the mixing of substances like opioids, alcohol, or stimulants—dramatically increases the risk of overdose and addiction. Governments respond with interventions such as harm reduction programs, monitoring systems, and treatment expansion. However, people may still turn to polydrug use for relief, more potent effects, or due to tolerance and availability. Preventing escalation requires self-management skills, supportive families, and community resources that provide education, care, and safe alternatives.
Polydrug Use: Why People Mix Substances and Why It Matters
Polydrug use—the act of combining two or more substances—poses one of the most serious risks in addiction and overdose today. To understand why people mix drugs despite the dangers, it’s essential to look at the behavioral, physiological, and situational factors that drive this behavior.
1. Pharmacological Criteria
Some individuals intentionally combine drugs because of how they interact in the body:
- Synergistic effects: Certain drugs amplify each other’s impact, such as alcohol and benzodiazepines, which together greatly intensify sedation.
- Balancing effects: Users may mix stimulants and depressants (e.g., cocaine and alcohol) to feel alert yet less anxious, or sedated but not excessively drowsy.
- Potentiation: Some substances increase the strength or absorption of others, like alcohol and opioids, which dangerously heighten respiratory depression.
2. Tolerance and Dependence
As tolerance develops, one drug may no longer produce the desired high. This can lead users to:
- Combine multiple drugs to achieve more potent effects.
- Turn to cross-tolerance—mixing substances from related drug classes when one loses potency.
3. Psychological and Behavioral Factors
Behavior and mental health play a significant role in polydrug use:
- Chasing new highs: A single drug may no longer satisfy, leading people to mix substances for a novel experience.
- Coping mechanisms: Some combinations are used to self-medicate—for example, stimulants to offset alcohol’s depressive effects, or depressants to reduce stimulant-induced anxiety.
- Social influence: Peer groups, cultural norms, and party settings can encourage experimenting with combinations.
4. Risk Perception
Many individuals believe specific mixes are “safe” if they’ve used them before without immediate harm. However, this perception is misleading—pharmacologically, these combinations remain highly dangerous.
5. Situational Factors
External circumstances often shape drug mixing:
- Availability: People use what’s accessible, sometimes unintentionally combining substances.
- Setting and intent: Social events may encourage stimulant–alcohol combinations for energy, while self-medication might involve depressants for sleep or stress relief.
⚠️ The Reality Check
While some people perceive “benefits” from mixing substances, the risks are profound. Combining central nervous system depressants—such as opioids, alcohol, and benzodiazepines—can suppress breathing to fatal levels. Mixing opioids with stimulants (like cocaine or methamphetamine) puts extreme strain on the heart and body. Ultimately, polydrug use magnifies the danger of overdose, organ failure, and death.
✅ Key Takeaway:
Understanding the behavioral, physiological, and situational reasons behind polydrug use is essential for prevention and intervention. By recognizing these drivers, individuals, families, and communities can take steps toward healthier coping strategies and safer choices.
Government Interventions to Prevent Multidrug Overdoses
Preventing multidrug overdoses is complex because many overdoses now involve multiple substances—like opioids combined with benzodiazepines, alcohol, or stimulants. Governments have implemented a variety of interventions at the local, state, and federal levels. Here’s a structured overview:
1. Harm Reduction Strategies
- Naloxone Distribution: Programs expand public access to naloxone (Narcan), giving first responders, families, and communities a life-saving tool. Multiple doses may be needed in polydrug cases.
- Supervised Consumption Sites (SCS): Safe injection facilities allow trained staff to monitor use, provide sterile supplies, and respond immediately to overdoses.
- Drug Checking Services: Fentanyl test strips and drug analysis programs reduce the risk of accidental mixing with lethal adulterants.
2. Prescribing and Pharmaceutical Policies
- Prescription Drug Monitoring Programs (PDMPs): Track prescribing of opioids, stimulants, and benzodiazepines to prevent dangerous combinations.
- Safer Prescribing Guidelines: Policies discourage co-prescribing opioids and benzodiazepines to lower overdose risks.
- Medication-Assisted Treatment (MAT): Expanding access to methadone, buprenorphine, and naltrexone helps stabilize people with opioid use disorder, lowering polydrug risks.
3. Public Health Education
- Awareness Campaigns: Public campaigns highlight the dangers of polysubstance use and educate on overdose recognition.
- Community Outreach: Targeted education in high-risk communities encourages safer behaviors and increases naloxone readiness.
4. Surveillance and Early Warning Systems
- Overdose Surveillance: Real-time monitoring identifies overdose spikes and emerging polydrug trends.
- Alert Systems: Public health agencies issue warnings about dangerous batches of drugs or spikes in fentanyl contamination.
5. Policy and Legal Interventions
- Good Samaritan Laws: Protect people calling 911 during overdoses from legal repercussions, encouraging timely help.
- Decriminalization & Diversion Programs: Shift people from incarceration to treatment and harm reduction services.
- Funding Addiction Treatment: Expanding mental health and SUD services increases access to ongoing care.
6. Research and Innovation
- Governments and research institutions fund studies on drug interactions, overdose trends, and effective interventions to guide more innovative policies.
✅ Key Takeaway:
Multidrug overdose prevention requires a combined approach—harm reduction, safer prescribing, treatment access, education, legal protections, and research. No single intervention is enough on its own, but together they create a safety net to reduce deaths.
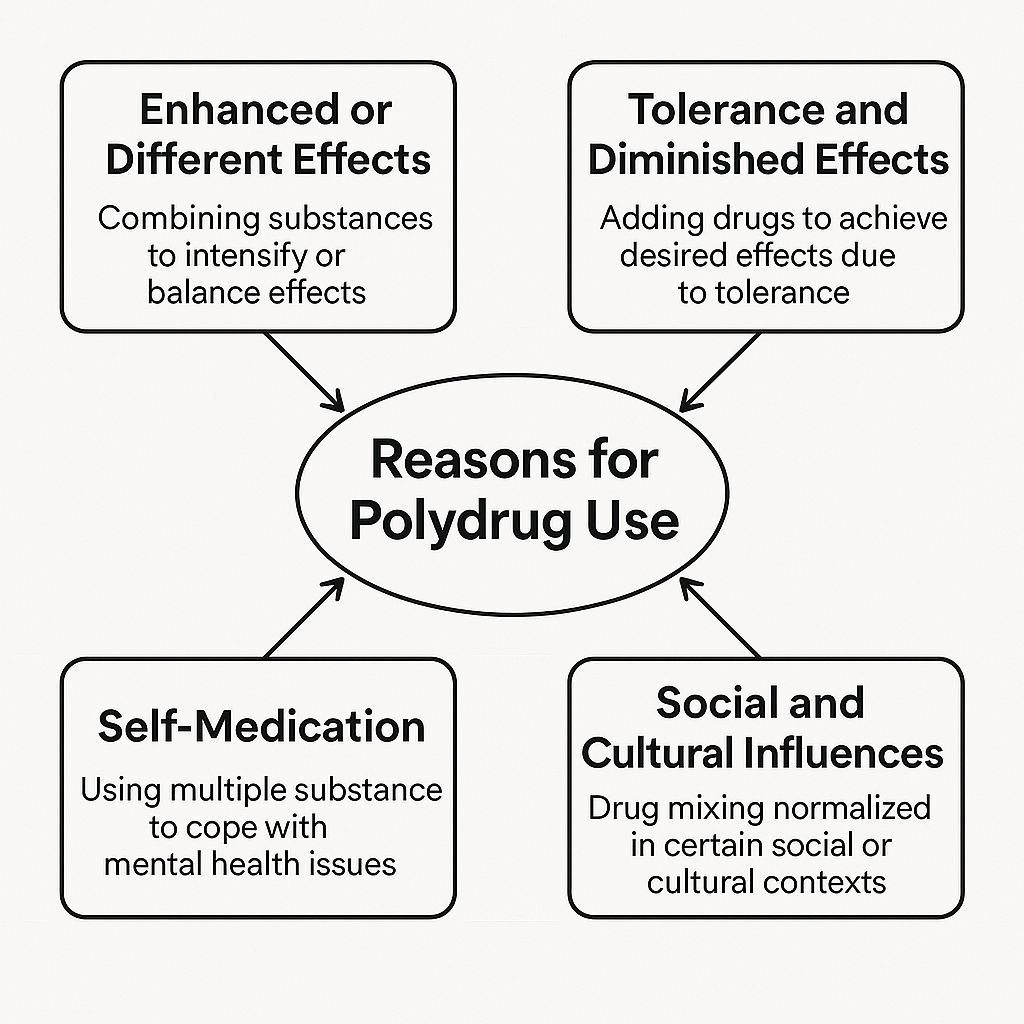
Even though polydrug use is dangerous, people struggling with addiction may still combine substances for several reasons:
Why People Engage in Polydrug Use Despite the Dangers
Polydrug use—mixing two or more substances—is one of the most dangerous patterns in addiction, yet many people still engage in it. The reasons are often complex, blending biology, psychology, environment, and culture. Here’s a closer look at the main drivers:
1. Enhanced or Different Effects
- Some mix drugs to intensify the high, such as combining opioids with benzodiazepines for more profound sedation.
- Others aim to balance effects—for example, using cocaine with alcohol or opioids to reduce jitters while still feeling energized.
2. Tolerance and Diminished Effects
- Over time, tolerance builds, and a single drug no longer produces the same effect.
- To compensate, people add other substances to regain the initial intensity they once felt.
3. Self-Medication
- Many use drug combinations to cope with mental health challenges like trauma, anxiety, or depression.
- A typical example: opioids for physical pain paired with alcohol or benzodiazepines to manage stress or anxiety.
4. Availability and Environment
- Sometimes, polydrug use isn’t planned—it’s about what’s available at the moment.
- Street drugs are often adulterated, such as cocaine laced with fentanyl, leading to unintended mixing.
5. Social and Cultural Influences
- Specific mixes, like “speedballing” (heroin + cocaine), carry a cultural reputation.
- Peer influence and party settings can normalize polydrug use, making it seem less risky than it is.
6. The Addiction Cycle
- Addiction itself drives compulsive use despite obvious risks.
- The brain’s reward system prioritizes short-term relief or pleasure over long-term safety, making rational decision-making very difficult.
✅ Key Takeaway
People who engage in polydrug use don’t necessarily seek danger—they seek relief, intensity, or escape. Unfortunately, combining substances overwhelms the body, especially the brain, heart, and lungs, greatly increasing the risk of overdose and death.
Self-Management Strategies to Prevent Polydrug Use and Addiction
Preventing polydrug use from escalating into addiction begins with the individual. By building awareness, developing healthier coping mechanisms, and creating supportive systems, people can make safer decisions and reduce their risks. Here are practical self-management strategies:
1. Awareness & Education
- Understand the risks: Mixing drugs like opioids and benzodiazepines can dangerously suppress breathing.
- Know drug interactions: Even prescribed medications combined with alcohol can be harmful.
- Track use: Journaling substance use patterns can highlight early signs of escalation.
2. Healthy Coping Mechanisms
- Stress management: Replace substances with mindfulness, yoga, breathing exercises, or journaling.
- Physical health routines: Regular exercise, balanced nutrition, and quality sleep strengthen resilience.
- Creative outlets: Engage in art, music, writing, or sports as positive alternatives for emotional release.
3. Behavioral Strategies
- Set limits: Define personal boundaries (e.g., no mixing, no use on weekdays).
- Delay and distract: Pause during cravings and shift to another activity.
- Avoid high-risk settings: Steer clear of environments where polydrug use is the norm.
4. Mental Health Support
- Therapy and counseling: Address depression, anxiety, or trauma that may fuel substance use.
- Mindfulness-based relapse prevention: Strengthens awareness of triggers and teaches acceptance over reaction.
5. Social & Accountability Systems
- Peer support groups: Programs like SMART Recovery help build healthier habits early on.
- Accountability partners: Share goals with a trusted friend or family member.
- Build sober networks: Surround yourself with people who model healthy coping instead of drug use.
6. Safety Planning
- Have naloxone available: Prepare for emergencies in case of opioid exposure.
- Check medications: Always consult a doctor before combining prescriptions or drinking alcohol.
- Set emergency steps: Know who to call and what to do if the risk of relapse escalates.
✅ Key Takeaway
Preventing polydrug addiction isn’t only about avoiding drugs—it’s about self-awareness, healthier coping skills, and supportive networks. By taking intentional steps, individuals can reduce their risks and build resilience for long-term well-being.
Family Support Strategies to Prevent Polydrug Use
Families can play a critical role in preventing polydrug use before it progresses into addiction. Here are key strategies broken down into practical approaches:
1. Education and Awareness
- Share accurate information: Talk openly about the dangers of mixing substances, including prescription meds with alcohol.
- Model healthy behaviors: Caregivers should avoid normalizing heavy drinking, drug use, or mixing medications at home.
- Early intervention: Watch for warning signs such as secretive behavior, sudden mood changes, or risky peer groups.
2. Communication and Emotional Support
- Open dialogue: Create safe spaces for honest conversations about stress and peer pressure.
- Active listening: Listen with empathy instead of lecturing to reduce shame and encourage honesty.
- Address underlying issues: Support loved ones in managing anxiety, depression, or trauma that may fuel polydrug use.
3. Structure and Boundaries
- Clear expectations: Establish and consistently reinforce family rules around substance use.
- Monitor and supervise: Know where children are, who they’re with, and what medications are present.
- Medication safety: Securely store prescriptions to prevent misuse or accidental mixing.
4. Encourage Healthy Alternatives
- Promote positive activities: sports, creative outlets, and volunteering provide a sense of belonging without substances.
- Family bonding: Shared meals, traditions, and outings strengthen relationships and reduce risky behaviors.
5. Build Protective Networks
- Connect with resources: Encourage participation in prevention workshops, mentoring, or youth programs.
- Peer support: Guide loved ones to sober, supportive peer groups.
- Seek help early: Use family therapy or counseling to reduce risks before substance use escalates.
6. Crisis and Safety Planning
- Know emergency steps: Families should recognize overdose signs and keep naloxone on hand if opioids are present.
- Good Samaritan awareness: Teach loved ones that calling for help during an overdose is legally protected in many states.
✅ Key Takeaway:
Families prevent polydrug use not by control, but by creating a foundation of trust, education, structure, and support, while promoting healthier ways to cope with life’s challenges.
Community Resource Strategies to Prevent Polydrug Use
Strong community resource strategies can help prevent polydrug use before it escalates into addiction. These focus on building networks of support, expanding prevention services, and creating safer environments where individuals can thrive.
1. Education and Prevention Programs
- School & youth programs: Provide evidence-based curricula to teach teens about the dangers of mixing substances.
- Public awareness campaigns: Local health departments can educate the public about safe medication practices, overdose prevention, and polydrug risks.
- Community workshops: Free sessions for families and individuals build awareness on stress management, coping skills, and warning signs.
2. Accessible Health & Mental Health Services
- Early intervention clinics: Offer screenings for mental health and substance use before problems escalate.
- Integrated care models: Community health centers combining medical, mental health, and addiction services help reduce treatment gaps.
- Telehealth services: Expands access to counseling and support, especially in underserved areas.
3. Peer and Recovery Support Networks
- Peer recovery coaches/mentors: People with lived experience guide others toward healthier choices.
- Support groups (SMART Recovery, AA/NA, secular groups): Provide safe spaces for discussing pressures and finding alternatives to drug use.
- Youth mentoring programs: Pairing at-risk youth with trusted adults lowers the likelihood of substance experimentation.
4. Harm Reduction Services
- Naloxone training and distribution: Ensures communities are prepared to respond to opioid-related overdoses.
- Drug-checking services: Allow individuals to test substances for fentanyl or other adulterants.
- Safe consumption and syringe programs: Reduce harm while linking people to treatment and recovery resources.
5. Policy and Environmental Supports
- Safe community spaces: Parks, recreation centers, and afterschool programs provide drug-free alternatives.
- Housing and employment resources: Stability in housing and work reduces pressures that can lead to polydrug use.
- Good Samaritan law promotion: Educating the public about legal protections encourages life-saving calls during overdoses.
6. Collaboration and Outreach
- Partnerships between schools, clinics, and nonprofits: Build prevention pipelines that catch risks early.
- Faith-based and cultural organizations: Deliver support that aligns with community values and traditions.
- Community coalitions: Local task forces track trends, share resources, and develop targeted strategies.
✅ Key Takeaway:
Preventing polydrug use is not just about restricting access to substances—it’s about building resilience, offering positive alternatives, and ensuring rapid access to help. Communities that combine education, health services, peer support, harm reduction, and policy change create safer, stronger environments for everyone.
Frequently Asked Questions
Here are some common questions:
Question: Provide a table about common polydrug combinations, why users take them, and the associated risks
Answer: A table summarizing common polydrug combinations, why users take them, and the associated risks:
| Extremely high overdose risk, heart failure, and respiratory depression | User’s Rationale / Desired Effect | Associated Risks |
|---|---|---|
| Alcohol + Benzodiazepines (Xanax, Valium) | Intensify relaxation, sedation, or “numb” emotions | Respiratory depression, coma, death, blackouts |
| Alcohol + Opioids (heroin, prescription painkillers) | Enhanced euphoria, stronger high | Respiratory failure, overdose, fatal synergistic effects |
| Cocaine + Alcohol | Balanced high: stimulant + depressant; longer-lasting euphoric effect | Cocaethylene formation (toxic metabolite), increased heart attack/stroke risk |
| Stimulants + Benzodiazepines | Counteract anxiety, crash, or “come down” from stimulant use | Unpredictable cardiovascular effects, overdose, impaired judgment |
| Opioids + Stimulants (“Speedball”) | Combine euphoria from opioid with energy from stimulant | Extremely high overdose risk, heart failure, respiratory depression |
| Cannabis + Alcohol | Intensify relaxation or euphoria | Increased nausea, dizziness, impaired motor control, risk of accidents |
| Prescription Stimulants + Alcohol | Reduce sedative effect of alcohol, prolong partying | Heart strain, impaired judgment, unpredictable intoxication |
| Multiple Prescription Medications (e.g., opioids + sedatives) | Manage pain, anxiety, or induce stronger sedation | High risk of overdose, dependency, liver or kidney damage |
✅ Key Takeaways:
- Most combinations are attempts to enhance or balance effects rather than purely experimental.
- Tolerance and psychological dependence drive many polydrug patterns.
- Even combinations perceived as “manageable” can be lethal, especially CNS depressants with alcohol or opioids.
- Risk is often underestimated due to social normalization or past non-lethal experiences.
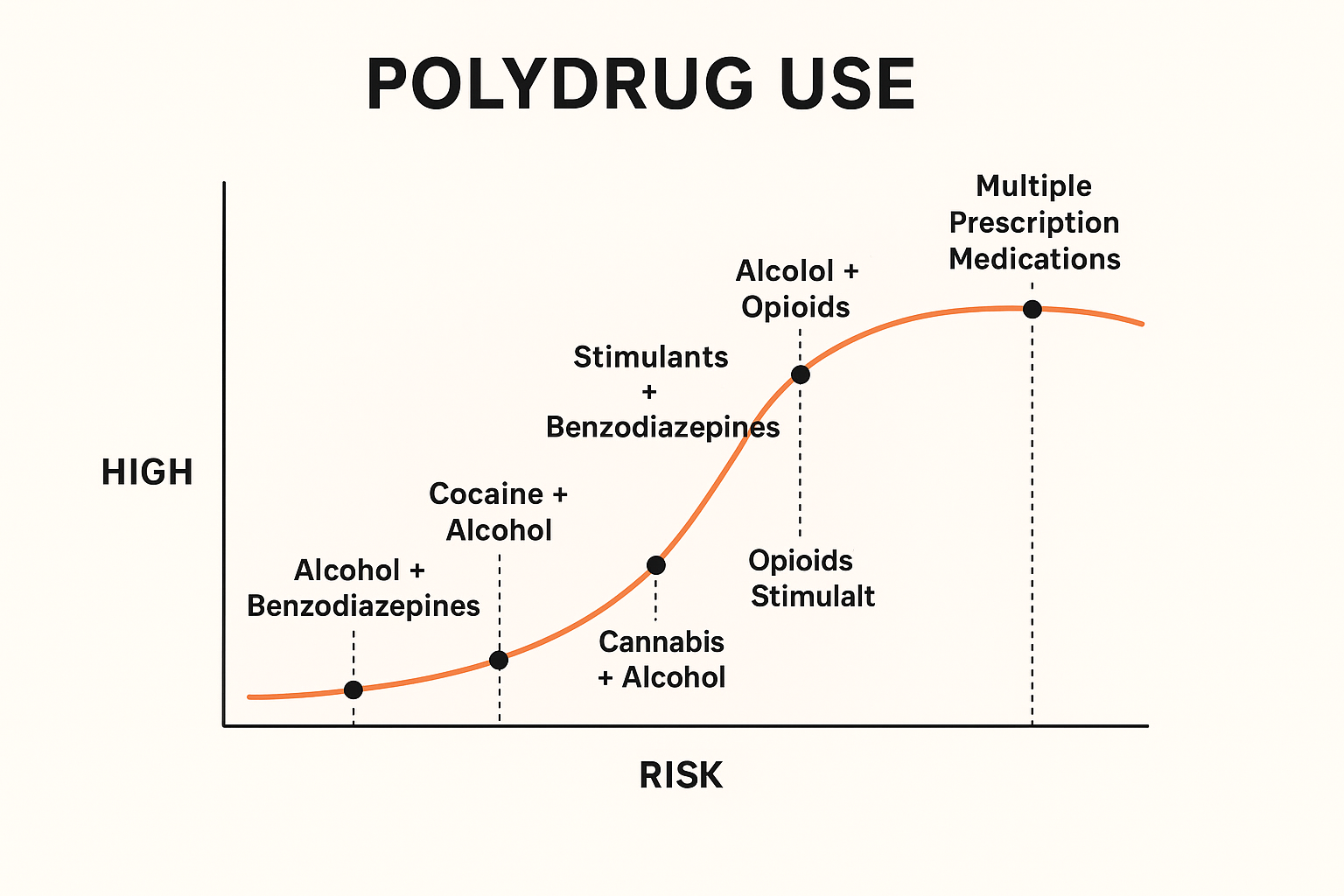
Question: Provide a graph about polydrug use in relation to the ability to get euphoric conditions.
Answer: Graph about the high vs risk” curve for the most common polydrug combinations
Question: Provide a flowchart showing how these interventions interact to prevent multidrug overdoses.
Answer: Flowchart showing how these interventions interact to prevent multidrug overdoses.
Conclusion
Polydrug use remains a pressing public health challenge, as the combination of substances magnifies both short-term risks like overdose and long-term risks of addiction. Addressing it requires more than awareness of its criteria or the dangers it poses—it demands a coordinated response. Government interventions provide structural safeguards through policies, monitoring systems, and harm-reduction measures, while individuals practice self-management to avoid risky combinations. Families strengthen this prevention by fostering open communication, safe environments, and supportive connections, and communities amplify these efforts through education, accessible health services, peer mentoring, and recovery networks. Together, these layers form a comprehensive defense against the cycle of polydrug use, ensuring that individuals at risk have the knowledge, support, and resources to choose healthier paths and reduce the likelihood of addiction.
Video: Can You Spot the Signs of a Multi-Drug Overdose and Save a Life?, Top 5 Dangers of Mixing Drugs, Why Mixing Drugs Is So Dangerous!
