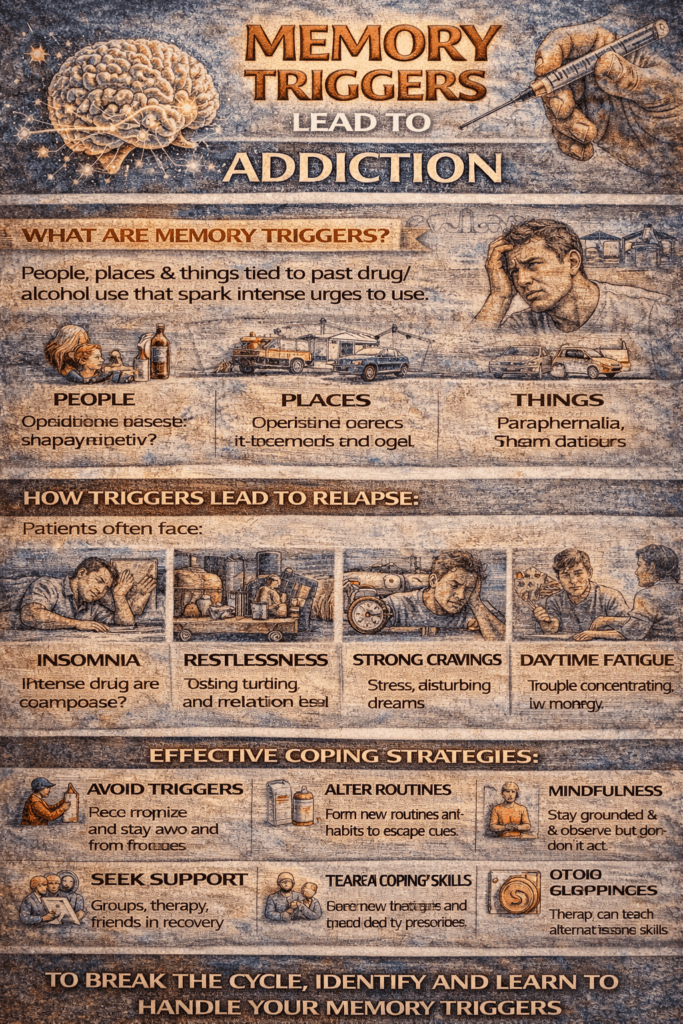
Memory triggers can powerfully influence addiction and relapse by activating brain pathways involved in craving, emotion, and reward. Cues like people, places, or emotions can reignite urges through regions such as the amygdala and hippocampus. Managing these triggers requires self-awareness and tools like mindfulness, routines, and cognitive strategies. Family support through open communication and clear boundaries, along with community resources such as peer groups and recovery programs, can provide vital structure and connection. Together, these strategies help reduce the impact of triggers and support long-term recovery.
How Memory Triggers Fuel Addiction: The Brain Science Behind Cravings and Relapse
Memory triggers can play a decisive role in addiction by activating brain pathways associated with craving, emotional regulation, and learned behavior. Here’s how this process unfolds—and how it can be managed in recovery.
🧠 1. Addiction and Memory Are Neurobiologically Linked
Addiction is not just a chemical dependence—it’s also a learning and memory disorder. Substances like drugs and alcohol “hijack” the brain’s reward system, particularly:
- The amygdala (emotional memory)
- The hippocampus (contextual memory)
- The nucleus accumbens (reward and craving)
Over time, repeated substance use creates strong neural associations between the drug and specific environments, emotions, or experiences.
🔁 2. Triggers as Conditioned Cues
A trigger is any internal or external cue that reminds the brain of drug use. Common examples include:
- People (e.g., old friends)
- Places (e.g., a bar, a particular street corner)
- Objects (e.g., lighters, syringes)
- Emotions (e.g., stress, sadness, excitement)
- Sensory cues (e.g., the smell of alcohol, certain music)
Through classical conditioning, the brain learns a pattern:
Trigger ➝ Memory of Use ➝ Craving ➝ Behavior (use again)
Even years into sobriety, exposure to these cues can reactivate old neural circuits, causing intense cravings or a relapse episode.
🔄 3. Emotional Memory and Relapse Risk
Emotionally charged memories—especially those tied to trauma, euphoria, shame, or loss—can resurface during high-stress moments and increase relapse risk, particularly when:
- Coping mechanisms are underdeveloped
- The person is socially isolated
- The trigger is unexpected or frequent
Example:
A recovering alcoholic hears a song from a euphoric night of drinking. That emotional memory—combined with current life stress—can spark a powerful craving.
🔬 4. Cue-Induced Craving (Scientific Term)
This phenomenon is called cue-induced craving. Brain imaging studies (like fMRI) show that even sober individuals exhibit activity in the brain’s reward and emotional centers when exposed to drug-related stimuli. These cravings are not imagined—they reflect a lasting imprint of addiction on the brain.
🛡️ Prevention and Recovery Strategies
To combat memory-triggered cravings, individuals in recovery can benefit from:
- Cognitive Behavioral Therapy (CBT): Reframes responses to triggers
- Mindfulness Training: Improves awareness and regulation of thoughts and emotions
- Trigger Mapping: Helps identify and prepare for personal triggers
- Exposure Therapy: Gradually desensitizes individuals to triggers under supervision
- Support Networks: Connection to others reduces isolation and emotional vulnerability
🔚 In Summary
Triggers activate learned memory circuits that associate drug use with pleasure, relief, or escape. These memories can be vivid, emotional, and persistent, even long after the last use. Understanding the science behind these triggers—and using strategies to manage them—is essential for preventing relapse and building long-term recovery.
10 Powerful Self-Management Strategies to Prevent Triggers and Relapse in Addiction Recovery
Cravings and triggers are inevitable in addiction recovery—but they don’t have to lead to relapse. Here are effective self-management strategies to help prevent and manage triggers, build resilience, and maintain long-term sobriety. These tools empower individuals to respond to cravings constructively rather than impulsively.
🔑 Self-Management Strategies for Trigger Control & Relapse Prevention
🧘♀️ 1. Mindfulness and Grounding Techniques
Learn to recognize triggers in the moment—without reacting to them.
- Mindfulness Meditation – observe thoughts and cravings non-judgmentally.
- 5-4-3-2-1 Technique – ground yourself using your five senses.
- Deep Breathing or Progressive Muscle Relaxation – instantly reduces stress and tension.
🧠 Why it works: These techniques break the automatic cycle between trigger and substance use.
📓 2. Trigger Awareness & Mapping
Become aware of your personal high-risk moments and emotions.
- Keep a trigger journal.
- Use daily check-ins to monitor stress, mood, and environment.
- Try a weekly Trigger Mapping Worksheet to stay proactive.
🧠 Why it works: Knowing your triggers ahead of time helps you prepare and respond calmly.
📞 3. Reach Out (Support System Activation)
Build a reliable network you can turn to when cravings hit.
- Contact a sponsor, therapist, or sober friend when feeling triggered.
- Join peer support groups like AA, NA, or SMART Recovery.
- Set up weekly accountability check-ins with someone you trust.
🧠 Why it works: Connection and support reduce the isolation that often leads to relapse.
🚪 4. Avoidance + Escape Plan
Sometimes, the best move is simply walking away.
- Avoid people or places known to be triggering.
- If caught in a risky setting, leave early or excuse yourself.
- Prepare an “emergency script” like, “Sorry, I have an early morning.”
🧠 Why it works: Creating physical distance gives your brain time to cool down.
🎯 5. Create New Habits and Daily Routines
Structure is protective in early and long-term recovery.
- Build a daily schedule that includes regular meals, sleep, movement, and responsibilities.
- Engage in positive, enjoyable activities like reading, art, or nature walks.
- Watch for HALT: Hungry, Angry, Lonely, Tired—states that increase relapse risk.
🧠 Why it works: A filled, purpose-driven life leaves less room for cravings.
💡 6. Cognitive Restructuring (CBT Techniques)
Challenge the irrational thoughts that lead to unhealthy behaviors.
- Identify common cognitive distortions like “Just once won’t hurt.”
- Replace them with realistic self-talk: “This feeling will pass.”
- Use thought logs to catch and reframe impulsive thinking patterns.
🧠 Why it works: Rewriting the internal script gives you back control over your choices.
🏋️♂️ 7. Exercise and Physical Movement
Engage your body to reset your brain.
- Walk, stretch, dance, or do yoga—especially during or after a triggering event.
- Choose easy and accessible forms of movement to stay consistent.
🧠 Why it works: Physical activity releases dopamine and lowers anxiety naturally.
📱 8. Crisis Tools and Digital Apps
Let technology support your recovery.
- Use sobriety apps like I Am Sober, Sober Grid, or Reframe.
- Keep emergency coping notes or affirmations on your phone.
- Have access to 24/7 hotlines for real-time emotional support.
🧠 Why it works: Support is available instantly—even when you’re alone.
✍️ 9. Relapse Prevention Planning
A written plan can be a robust safety net.
- Know your early warning signs (e.g., missing meetings, irritability).
- List actions to take when feeling tempted.
- Keep an emergency contact list handy at all times.
🧠 Why it works: Having a plan provides clarity during chaotic emotional moments.
🕊️ 10. Self-Compassion and Acceptance
Don’t punish yourself for having cravings—they’re part of the process.
- Use affirmations like: “I am not my addiction,” or “This will pass.”
- If you slip, practice non-judgmental awareness and get back on track with support.
🧠 Why it works: Compassion short-circuits shame, which is a significant relapse risk.
💬 Final Thoughts
Managing addiction triggers is not about perfection—it’s about preparation, presence, and persistence. With the right tools, you can face cravings without fear and build a recovery that lasts.
10 Family Support Strategies to Prevent and Manage Addiction Triggers
When a loved one is in addiction recovery, families play a crucial role—not just emotionally, but in helping prevent relapse. These family support strategies can help identify, manage, and reduce triggers, creating a safer and more stable environment for healing.
💬 1. Open, Nonjudgmental Communication
Encourage honest conversations about cravings, triggers, and emotional struggles.
- Use active listening: “Tell me how you’re feeling.”
- Avoid blame or guilt-based language.
- Speak with “I” statements: “I noticed you’ve seemed stressed lately.”
🧠 Why it works: Builds trust and creates a safe space for vulnerability—before a crisis occurs.
📚 2. Educate the Family About Triggers and Relapse
Learn about the science and patterns of addiction together.
- Attend family psychoeducation or support groups, such as Al-Anon or SMART Recovery Family & Friends.
- Understand the difference between a slip and a relapse.
- Learn about the biological and emotional roots of cravings.
🧠 Why it works: Informed families can catch warning signs early and respond supportively.
🚫 3. Remove or Reduce Environmental Triggers
Make your home a recovery-friendly space.
- Remove alcohol, drugs, and paraphernalia.
- Limit exposure to people who enable substance use.
- Avoid activities that could trigger, such as certain parties or shows.
🧠 Why it works: Reducing visual and social cues minimizes cravings.
🛑 4. Establish Boundaries and Consistency
Healthy boundaries are essential for everyone’s safety and growth.
- Say: “We support your recovery, but not your use.”
- Maintain consistent rules and routines.
- Avoid enabling (e.g., covering up consequences).
🧠 Why it works: Predictability and structure reduce stress and chaos, which are relapse risks.
🧘 5. Support Healthy Coping and Routine
Help build a lifestyle that supports sobriety.
- Engage in healthy activities together (walks, cooking, volunteering).
- Encourage regular meals, sleep, and responsibilities.
- Normalize emotional self-care, such as journaling or talking.
🧠 Why it works: Stable routines reduce impulsivity and boost emotional resilience.
☎️ 6. Be an Accountability Partner
Support your loved one without micromanaging them.
- Check in regularly: “How are you feeling today?”
- Celebrate milestones, even small ones.
- Encourage them to stick to their recovery plan—but avoid policing.
🧠 Why it works: Encouragement with respect helps maintain motivation and self-awareness.
💥 7. Help Manage Conflict or Stress
Family tension is one of the most common triggers—address it directly.
- Practice family problem-solving techniques.
- Learn conflict de-escalation skills.
- Encourage talking through issues before stress builds.
🧠 Why it works: A calm home reduces emotional triggers that could lead to relapse.
🛟 8. Have a Family Emergency Plan
Know what to do if a relapse or craving crisis happens.
- Discuss what support they want during cravings (talking, distraction, leaving).
- Agree on a response plan after a slip.
- Keep emergency contacts nearby (sponsor, therapist, hotline).
🧠 Why it works: A calm, structured response limits the damage and helps recovery resume faster.
❤️ 9. Offer Compassion, Not Control
Your role isn’t to fix everything—to walk beside them.
- Use affirmations like: “I know you’re trying,” or “I believe in your strength.”
- Avoid rescuing or trying to control the situation.
- Respect their autonomy, while staying engaged.
🧠 Why it works: Compassion builds intrinsic motivation rather than fear or shame.
🧩 10. Engage in Family Recovery Together
Addiction affects the entire family—and recovery should, too.
- Attend family therapy together.
- Reflect as a family on how addiction has impacted each member.
- Focus on rebuilding trust and connection, not just preventing relapse.
🧠 Why it works: Healing the family system creates a stronger foundation for lasting sobriety.
🧠 Final Thought:
Supporting someone in recovery is not about control—it’s about compassion, education, structure, and connection. When families show up with empathy and awareness, they become powerful partners in relapse prevention.
10 Community-Based Strategies to Prevent and Manage Addiction Triggers
Community resources are essential in preventing and managing addiction triggers by offering external structure, social support, meaningful engagement, and professional tools to navigate recovery. These strategies strengthen a person’s safety net and reduce isolation—two key factors in relapse prevention.
🏘️ Community Resource Strategies to Prevent or Manage Triggers in Addiction
🤝 1. Peer Support Groups
Why it helps:
Shared experiences reduce shame and isolation while offering proven coping tools.
Examples:
- 12-Step Programs (AA, NA, Al-Anon)
- SMART Recovery (science-based, CBT-informed)
- Celebrate Recovery (faith-based)
- LifeRing, Women for Sobriety
How to use:
- Attend regularly, even during stable periods
- Use as safe spaces to discuss triggers, cravings, and emotional struggles
- Build a sober network for support outside meetings
🧑⚕️ 2. Outpatient and Recovery Programs
Why it helps:
Structured treatment and ongoing therapy keep individuals focused and supported.
Examples:
- Intensive Outpatient Programs (IOP)
- Recovery Community Organizations (RCOs)
- Day treatment centers, sober living support
- MAT clinics (Medication-Assisted Treatment)
How to use:
- Engage in individual and group therapy
- Follow relapse prevention modules and aftercare
- Build coping skills and structured routines
📞 3. 24/7 Crisis and Support Hotlines
Why it helps:
Immediate support during intense urges or emotional distress.
Examples:
- SAMHSA’s National Helpline: 1-800-662-HELP (4357)
- Peer warmlines and local mental health lines
- Crisis Text Line (Text 741741)
How to use:
- Call/text during high-risk or emotional overwhelm
- Use when peer or family support isn’t available
- Get referrals for shelters, detox, or counseling
🏠 4. Sober Living Homes and Transitional Housing
Why it helps:
Provides a structured, substance-free environment with accountability.
Features:
- Curfews, drug testing, peer support
- Life skills development
- Connection to outpatient care and support meetings
How to use:
- Use during early recovery or post-rehab
- Surround yourself with people committed to sobriety
📚 5. Community Centers & Libraries
Why it helps:
Offer structured, engaging activities that reduce idle time—a common relapse risk.
Examples:
- Art, job training, meditation, fitness groups
- Book clubs, events, and computer labs
How to use:
- Build a weekly routine with non-triggering activities
- Reduce loneliness and explore new interests and roles
💼 6. Employment & Vocational Support Services
Why it helps:
Having purpose reduces emotional triggers like financial stress or boredom.
Examples:
- Vocational rehabilitation
- Recovery-friendly employers, job fairs
- Reentry programs (especially post-incarceration)
How to use:
- Seek job coaching, résumé help, or certifications
- Build independence and self-worth
🧠 7. Faith-Based or Spiritual Groups
Why it helps:
Provides connection, guidance, and a sense of meaning.
Examples:
- Church, temple, or mosque recovery groups
- Celebrate Recovery, Dharma Recovery
- Pastoral counseling, prayer circles
How to use:
- Attend weekly services or meetings
- Use faith/spiritual tools during emotional triggers
🏞️ 8. Recreational and Wellness Programs
Why it helps:
Promotes mental health and offers drug-free stress relief.
Examples:
- Parks & Rec classes (yoga, sports, art therapy)
- Hiking clubs, meditation groups
- Community gardens, dance classes
How to use:
- Schedule wellness during high-risk times
- Use movement or creativity as emotional outlets
🧾 9. Legal, Housing, and Financial Support Services
Why it helps:
Life instability is a significant relapse risk. These services offer critical stabilization.
Examples:
- Community legal aid
- Housing programs and shelters
- Financial coaching or benefit help
How to use:
- Seek help before stress becomes unmanageable
- Work with advocates or case managers for support
📆 10. Create a Personalized Community Recovery Calendar
Why it helps:
Predictable structure prevents relapse by reducing downtime and impulsivity.
Tips:
- Schedule weekly therapy, support groups, fitness, and social time
- Use apps or planners to track healthy habits and avoid triggers
✅ Final Takeaway:
Recovery doesn’t have to be done alone. Whether it’s a support group, spiritual community, wellness center, or job service, community resources reduce vulnerability to addiction triggers by providing structure, connection, and purpose.
Frequently Asked Questions
Here are some common questions:
Question: Provide a trigger mapping worksheet.
Answer: Trigger Mapping Worksheet
Understanding and Managing Your Triggers for Recovery
Section 1: Identify Your Triggers
List common external and internal triggers that lead to cravings or urges to use.
| Type | Trigger Description | Example |
|---|---|---|
| People | e.g., Old using friends | |
| Places | e.g., A club, neighborhood | |
| Things/Objects | e.g., Lighter, bottle, pill bottle | |
| Emotions | e.g., Stress, sadness, loneliness | |
| Situations | e.g., Fights, payday, being alone | |
| Sensory Cues | e.g., Smell of alcohol, song, certain lighting |
Section 2: Trigger → Memory Link
Describe what memory or emotional association the trigger brings up. This helps uncover the underlying connection.
| Trigger | Associated Memory or Feeling | Strength of Craving (1–10) |
|---|---|---|
Section 3: Automatic Thought and Urge
When triggered, what automatic thoughts or urges arise?
| Trigger | Thought/Belief (“I need it”, “Just once won’t hurt”) | Urge to Use (Low/Medium/High) |
|---|---|---|
Section 4: Coping Strategy Plan
Create a plan to respond healthily when faced with each trigger.
| Trigger | Coping Strategy | Support Person or Tool to Use |
|---|---|---|
| e.g., Deep breathing, call sponsor, leave place | e.g., Friend, journal, hotline | |
Section 5: Weekly Trigger Tracker
Use this tracker to reflect on your week.
| Date | Trigger Encountered | Response | Was the Coping Strategy Effective? (Y/N) | Notes |
|---|---|---|---|---|
💬 Reflection Prompt
What did you learn about your triggers this week?
What worked well? What needs improvement?
✍️ Write here:
Question: Provide a relapse prevention plan template.
Answer: Here is a Relapse Prevention Plan Template designed to help individuals in recovery identify risks, develop healthy coping strategies, and maintain long-term sobriety. It can be used in therapy, support groups, or as a self-help tool. Let me know if you’d like this as a fillable or printable PDF with calming visuals.
🌱 Relapse Prevention Plan Template
🧠 1. Personal Warning Signs
List your early warning signs that may signal a risk of relapse (emotional, physical, behavioral):
| Emotional | Physical | Behavioral |
|---|---|---|
| e.g., Irritability, sadness | e.g., Fatigue, headaches | e.g., Skipping meetings, isolating |
🔍 2. Common Triggers
Identify external or internal situations that trigger cravings:
| People | Places | Situations | Emotions |
|---|---|---|---|
🛠️ 3. Coping Strategies for Triggers
List healthy ways you will respond to each trigger:
| Trigger | Coping Strategy | Example |
|---|---|---|
| Deep breathing, call a friend | When I feel lonely, I’ll go for a walk and call my sponsor. | |
| Mindfulness or distraction | When I’m anxious, I’ll journal or listen to calming music. |
📅 4. Daily and Weekly Recovery Routine
Structure keeps you anchored. Outline your positive daily habits:
| Daily Self-Care | Weekly Goals |
|---|---|
| Sleep schedule, meals, physical activity | Attend 3 meetings, connect with support network |
🤝 5. Support System
List people and resources you can turn to when you feel triggered or at risk:
| Name | Role | Contact Info |
|---|---|---|
| Sponsor, friend, therapist |
📲 6. Emergency Plan
What will you do immediately if you feel you might relapse?
- Call: ______________________________________
- Go to: _____________________________________
- Use coping skill: ____________________________
- Remind myself: _____________________________
💬 7. Motivational Reminders
Write personal reasons for staying sober:
- “I want to be there for my family.”
- “I’ve come too far to go back.”
- “I’m learning to love myself without substances.”
🧭 8. If I Slip…
Slips can happen. What will you do to recover quickly?
- I will tell: _________________________________________
- I will return to: ____________________________________
- I will learn from the slip by: __________________________
☑ “A slip is a signal, not a failure.”
🧘 9. Affirmations & Positive Self-Talk
List phrases to use when triggered:
“I am in control of my choices.”
“This feeling is temporary.”
“I don’t have to act on every craving.”
Question: Provide a family relapse prevention checklist.
Answer: comprehensive and practical Family Relapse Prevention Checklist—designed to help families actively support a loved one in recovery, manage triggers, and respond to early warning signs. Let me know if you’d like a printable or fillable PDF version with a calming design and icons.
✅ Family Relapse Prevention Checklist
🧠 Use this regularly to check in, prepare, and respond as a family unit.
🟢 1. Communication & Connection
- We regularly check in with our loved one using open, nonjudgmental questions.
- We actively listen and avoid criticism, blame, or lecturing.
- We talk about recovery goals and struggles when appropriate.
- We use “I” statements to express concerns calmly and respectfully.
🟠 2. Understanding Triggers
- We are aware of our loved one’s known people, places, and emotional triggers.
- We avoid exposing them to high-risk environments (e.g., alcohol at family events).
- We help them track and reflect on emerging stressors or cravings.
- We understand that relapse is a process, not a single event.
🧹 3. Creating a Safe Environment
- We have removed alcohol, drugs, and paraphernalia from the home.
- We maintain a calm and predictable home environment.
- We help establish a daily routine that includes meals, sleep, and self-care.
- We respect their boundaries while providing structure and encouragement.
💬 4. Crisis & Relapse Response Plan
- We know the early warning signs of relapse (isolation, irritability, lying, etc.).
- We have a plan for how to respond if a relapse or slip occurs.
- We have a list of emergency contacts: sponsor, therapist, and crisis hotline.
- We know how to offer support without enabling or shaming.
💞 5. Emotional & Social Support
- We remind them they are loved, valued, and not alone.
- We encourage healthy social connections and activities.
- We celebrate milestones and small wins in recovery.
- We support them in attending meetings or therapy sessions.
🛑 6. Boundaries & Accountability
- We have clearly stated and mutually agreed-upon boundaries.
- We avoid enabling behaviors (e.g., covering up consequences).
- We respect their autonomy while holding them accountable (e.g., by checking in).
- We understand our role is to support—not control—their recovery.
🌱 7. Family Self-Care & Growth
- We are seeking our own support (Al-Anon, therapy, or education).
- We practice emotional regulation and stress management ourselves.
- We acknowledge and work on the impact addiction has had on us.
- We stay hopeful and recognize recovery is a long-term journey.
📌 Reminders for Families
✔️ You didn’t cause the addiction.
✔️ You can’t cure it—but you can support recovery.
✔️ Stay calm, connected, and consistent.
✔️ Your support matters more than you know.
Question: Provide a community resource strategy worksheet.
Answer: A structured and easy-to-use Community Resource Strategy Worksheet designed to help individuals in recovery—and their families—identify, organize, and engage with local resources to prevent or manage addiction triggers and reduce relapse risk.
🏘️ Community Resource Strategy Worksheet
Build your personalized support system for trigger and relapse prevention
🧠 Section 1: Personal Triggers You Need Support With
List your top 3–5 triggers or relapse risks that community resources could help with.
| Trigger or Challenge | Example |
|---|---|
| Emotional stress or isolation | Feeling lonely on weekends |
| Unemployment or boredom | No routine or job |
| Substance-using environments | Old hangout spots |
| Housing insecurity | Couch-surfing or eviction |
| Mental health symptoms | Anxiety, depression flare-ups |
🤝 Section 2: Support Resources by Category
Use this section to explore and map available community resources that can support your recovery.
🔄 A. Peer Support & Recovery Groups
| Program Name | Type (AA, SMART, etc.) | Location/Online Link | Meeting Times | Contact |
|---|---|---|---|---|
🧑⚕️ B. Therapy / Counseling / Outpatient
| Provider or Clinic | Service Type (IOP, MAT, etc.) | Frequency | Contact Info |
|---|---|---|---|
🏠 C. Safe Housing / Sober Living
| Program Name | Type (Transitional, Recovery House) | Cost / Coverage | Location | Contact |
|---|---|---|---|---|
💼 D. Employment, Job Readiness, or Education
| Program or Agency Name | Services Provided (e.g., job search, résumé help) | Location / Online | Contact |
|---|---|---|---|
💬 E. Spiritual / Wellness / Recreational Support
| Group / Center | Type (Faith, Fitness, Art, Nature) | Schedule | Notes |
|---|---|---|---|
📞 F. Emergency or Crisis Services
| Service Name | Type (Crisis Line, Housing, Hotline) | Contact Info | When to Use |
|---|---|---|---|
🔄 Section 3: Weekly Community Recovery Schedule
Plan a recovery-supportive weekly structure using these resources.
| Day | Activity / Resource | Time | Purpose (support, structure, connection) |
|---|---|---|---|
| Monday | |||
| Tuesday | |||
| … | |||
| Sunday |
🧭 Section 4: Reflection & Follow-Up
- Which community resource has helped the most in managing your triggers so far?
Example: “SMART Recovery has helped me stop isolating.”
✍️ _______________________________________________ - Are there any barriers to accessing support (transport, cost, fear)?
✍️ _______________________________________________ - What is one new community resource you will try this week?
✍️ _______________________________________________
📌 Final Reminder
Recovery doesn’t happen alone.
Your community is part of your treatment.
Conclusion
Memory triggers deeply influence addiction and relapse by reactivating brain circuits tied to craving and emotional memories, making recovery challenging. However, understanding these neural pathways empowers individuals to use self-management strategies such as mindfulness and cognitive reframing to manage urges. Family support offers crucial emotional stability and boundaries that reduce exposure to triggers, while community resources provide structure, social connection, and professional help. Together, these approaches create a comprehensive support system that addresses both the psychological and environmental factors of addiction, fostering lasting recovery and resilience.
Video: How Long Do Addiction Triggers Last #MemoryTriggers #AddictionRecovery #BrainScience