Insurance companies use prior authorization (PA) to approve healthcare services, including medications and therapies. While it aims to control costs, PA can delay care and create administrative challenges, especially in addiction treatment. Self-management strategies help individuals navigate the process, while family support provides advocacy. Community resources, such as publicly funded programs and integrated care, can reduce reliance on PA and ensure timely access to treatment. Together, these approaches help minimize delays and barriers to necessary care.
The Impact of Prior Authorizations on Addiction Treatment and Medication Access
Prior authorization (PA) is a cost-containment strategy used by health insurance companies to regulate access to certain medications, treatments, and services. While PA intends to ensure appropriate and necessary use of healthcare resources, it often creates significant barriers for patients seeking timely addiction treatment. This blog explores the challenges posed by prior authorization in addiction treatment, its implications for patient care, and potential solutions to improve access to life-saving interventions.
Understanding Prior Authorization: Prior authorization requires healthcare providers to obtain approval from an insurance company before prescribing certain medications or treatments. This process is widespread for high-cost, high-risk, or potentially misused medications such as opioid use disorder (OUD) treatments, benzodiazepines, and certain psychiatric drugs. Insurers review the request based on clinical guidelines, medical history, and policy criteria before granting or denying coverage.
Barriers to Addiction Treatment Access
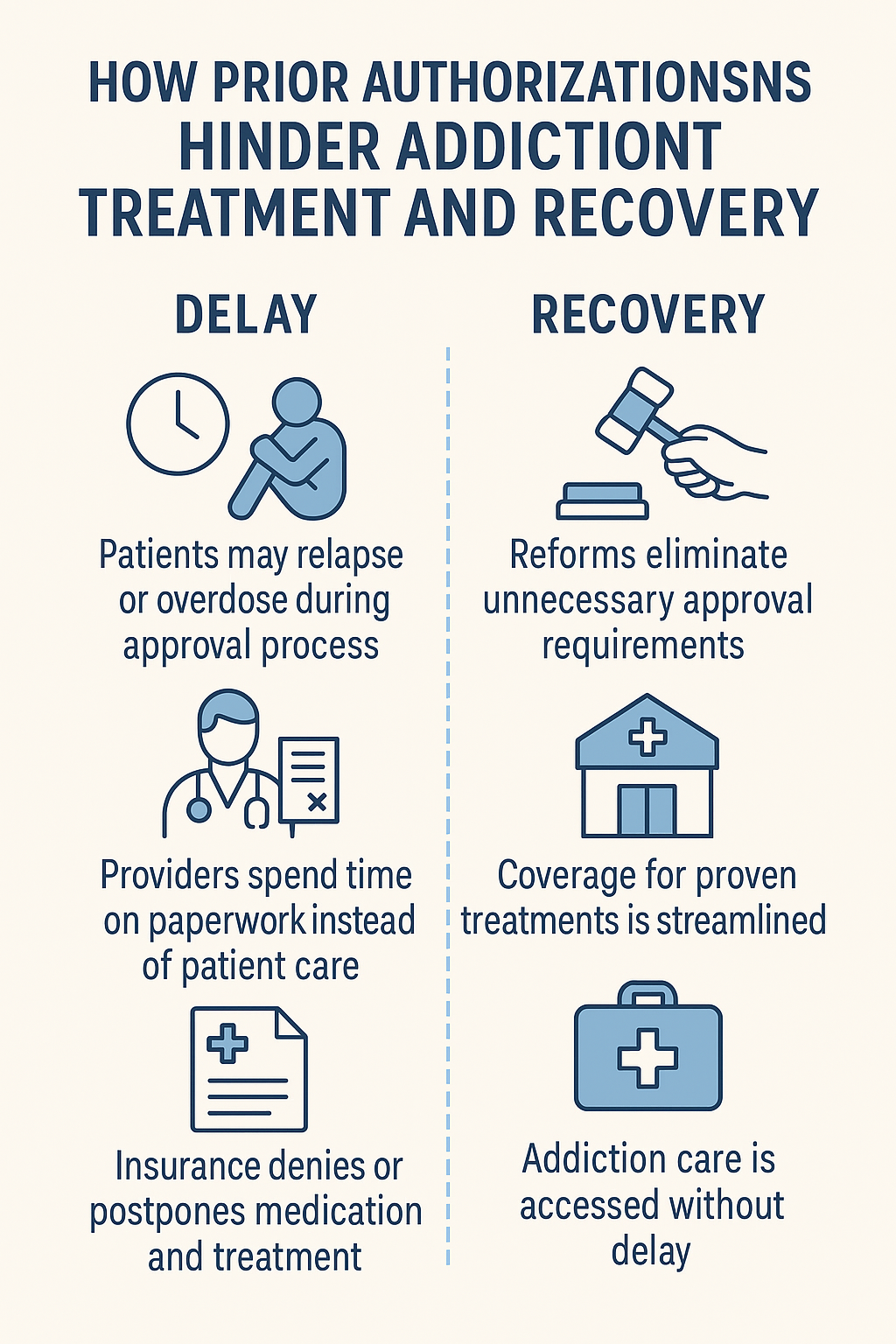
- Delays in Care: The PA process can take days or even weeks, delaying access to crucial medications like buprenorphine, methadone, or naltrexone, which are essential for opioid addiction treatment. Such delays can increase the risk of relapse, overdose, and even death.
- Increased Administrative Burden: Healthcare providers must complete extensive paperwork and follow up with insurers, diverting time away from patient care. The administrative workload can discourage physicians from prescribing necessary medications.
- Denial of Medically Necessary Treatment: Some patients are denied coverage based on stringent or outdated insurance criteria. This can force individuals to seek alternative, often less effective, treatments or abandon care altogether.
- Financial Strain on Patients: If a medication is denied, patients may have to pay out-of-pocket, which is not feasible for many individuals with substance use disorders (SUD). The high cost of alternative treatments can lead to discontinuation of therapy.
Implications for Patient Health and Recovery
- Higher Risk of Relapse: Interruptions in treatment can lead to withdrawal symptoms, increased cravings, and a return to substance use.
- Increased Overdose Rates: Without timely access to medication-assisted treatment (MAT), patients face a higher risk of fatal overdoses.
- Strain on Healthcare Systems: Delayed or denied treatment can lead to more emergency department visits, hospitalizations, and involvement with the criminal justice system.
Potential Solutions
- Streamlining PA Processes: Implementing electronic prior authorization (ePA) systems can reduce delays and administrative burdens.
- Legislative Reforms: Several states have passed laws to limit PA requirements for MAT, and further policy changes at the federal level could improve access.
- Gold Card Programs: Some insurers offer PA exemptions for providers with a history of appropriate prescribing, reducing barriers for established addiction specialists.
- Advocacy and Awareness: Patients and providers must advocate for reforms by engaging with policymakers and insurance companies to highlight the urgent need for improved access to addiction treatment.
While prior authorization is intended to regulate healthcare costs and ensure appropriate treatment, its application in addiction treatment often creates unnecessary barriers to care. Policymakers, healthcare providers, and insurers must work together to reform PA policies and ensure that individuals with substance use disorders receive timely, effective, and affordable treatment. Addressing these challenges is crucial in combating the addiction crisis and improving public health outcomes.
How Prior Authorizations Hinder Addiction Treatment and Recovery
Prior authorization (PA) can significantly hinder addiction treatment by creating barriers to timely and effective care. While intended to control healthcare costs and ensure appropriate use of treatments, the PA process often results in delays, financial burdens, and restricted access to essential medications and therapies. This blog explores how prior authorization impedes addiction treatment and what can be done to improve access.
1. Delays in Access to Treatment
- Time-Consuming Process: Obtaining prior authorization can be lengthy, delaying access to critical addiction treatments. This is particularly harmful for individuals experiencing withdrawal or in crisis who need immediate intervention.
- Interruption of Treatment: If approval is slow or denied, patients may experience treatment disruptions, exacerbating symptoms and increasing the risk of relapse.
2. Limited Access to Necessary Medications
- Restricting Access to Medications: Medications such as methadone, buprenorphine, or certain detoxification drugs often require a PA. Delays or denials can prevent individuals from receiving the medications they need to manage withdrawal and cravings.
- Alternative Medications May Not Be Effective: Insurers may approve only certain medications or generic alternatives that may not work as well for a patient’s specific needs, potentially leading to inadequate treatment and higher relapse rates.
3. Financial Barriers
- Increased Out-of-Pocket Costs: PA can sometimes result in higher costs for patients, especially if insurers deny coverage for a preferred medication, forcing patients to either pay out of pocket or forgo treatment.
- Treatment Disruption Due to Cost Issues: High costs or lack of coverage may lead patients to delay or discontinue care, worsening addiction and increasing the likelihood of relapse.
4. Limitation of Treatment Options
- Inflexible Treatment Plans: PA requirements may limit available treatment options, forcing patients into less effective therapies that do not align with their medical needs.
- Restricting Access to Comprehensive Care: Effective addiction treatment often requires a combination of medication, therapy, and support services. PA can limit access to this full spectrum of care, making long-term recovery more difficult.
5. Stigma and Misunderstanding of Addiction
- Underestimating the Necessity of Treatment: Some insurers may not fully recognize addiction as a medical condition, leading to unnecessary delays or denials.
- Difficulties with Medication-Assisted Treatment (MAT): MAT is crucial for treating opioid and alcohol use disorders, but often faces stringent PA requirements, preventing timely access to stabilizing medications.
6. Complicated Approval Processes
- Increased Administrative Burden: Providers must navigate complex PA requirements, submitting extensive documentation that delays treatment and adds frustration for both patients and clinicians.
- Possibility of Denial: Even after meeting all requirements, insurers may still deny PA requests, forcing patients into cycles of appeals and delays that prevent them from receiving the necessary care.
Prior authorization creates significant barriers to addiction treatment, delaying access to crucial medications and therapies while adding financial and administrative burdens. These obstacles can worsen addiction and make sustained recovery more difficult. Efforts to reform PA policies, streamline approval processes, and advocate for greater recognition of addiction as a medical condition are essential in ensuring individuals receive the care they need without unnecessary delays or restrictions.
Government Strategies to Reduce Prior Authorization Barriers in Addiction Treatment
Government strategies to reduce the need for and burden of prior authorization (PA) for addiction treatment can help ensure that individuals receive timely and effective care. These strategies aim to streamline the approval process, reduce barriers to treatment, and increase access to necessary services. This blog explores key government initiatives that can improve access to addiction treatment by addressing PA challenges.
1. Policy Reforms to Simplify Prior Authorization
- Standardization of Prior Authorization Processes: Governments can advocate for standardized and simplified PA procedures across insurance companies to reduce administrative complexity. A more streamlined process would lead to faster decisions and reduce delays in accessing addiction treatment.
- Automatic Approvals for Evidence-Based Treatments: Policies could be implemented that automatically approve specific evidence-based addiction treatments, such as medication-assisted treatment (MAT), detoxification services, and rehabilitation programs, without requiring prior authorization. This would help ensure that these proven interventions are accessible without unnecessary delays.
2. Expanding Access to Medication-Assisted Treatment (MAT)
- Incentivizing MAT Coverage: Governments can require insurers to cover MAT without prior authorization or at lower cost, particularly for individuals with opioid or alcohol use disorders. Ensuring that medications like methadone, buprenorphine, and naltrexone are easily accessible can significantly reduce dependency on PA for treatment access.
- Increasing Funding for MAT Programs: Expanding public funding for MAT programs can help reduce the reliance on private insurance and prior authorization processes. Public health programs, such as those funded by the Substance Abuse and Mental Health Services Administration (SAMHSA), can provide MAT directly to underserved populations, bypassing the need for PA altogether.
3. Strengthening Parity Laws
- Enforcing Mental Health and Addiction Parity: The Mental Health Parity and Addiction Equity Act (MHPAEA) mandates that insurance coverage for mental health and addiction treatment must be comparable to that of other medical treatments. Governments can strengthen enforcement of this law to ensure that addiction treatment, including MAT and rehabilitation services, is covered on the same terms as other medical conditions. This could reduce the need for prior authorization, especially for essential treatments.
- State-Level Parity Enforcement: State governments can implement their own laws and regulations to ensure that health insurers comply with parity requirements, making addiction treatment more accessible without cumbersome prior authorization processes.
4. Encouraging Alternative Payment Models
- Value-Based Care Models: Governments can promote value-based care, where healthcare providers are reimbursed based on patient outcomes rather than the number of services rendered. In these models, addiction treatment may be prioritized, with less reliance on prior authorization for specific treatments. Providers would have more flexibility to offer comprehensive addiction care tailored to the patient’s needs without waiting for approval.
- Bundled Payments for Addiction Treatment: Bundled payment models, in which a single payment is made for a full course of addiction treatment (including detox, therapy, and MAT), can reduce the need for individual prior authorizations for each treatment component. This can help ensure that individuals receive the entire continuum of care without delays.
5. Increasing the Availability of Public Health Programs
- Publicly Funded Treatment Programs: Expanding the availability of public health programs that provide addiction treatment, such as those funded by SAMHSA and Medicaid, can reduce dependence on private insurance and prior authorization. These programs can offer immediate access to MAT, therapy, and rehabilitation without requiring PA, ensuring that individuals can start treatment without delays.
- Integration of Addiction Services into Primary Care: Governments can encourage the integration of addiction treatment services into primary healthcare settings, where individuals may not require prior authorization for addiction-related care. This could include screening for substance use disorders, offering MAT, and providing counseling within the primary care context, improving access and reducing bureaucracy.
6. Incentivizing Insurance Reforms
- Reducing PA Requirements for Addiction Services: Governments can incentivize insurance companies to reduce or eliminate prior authorization for addiction treatments, particularly for medications and therapies that are proven to be effective. This can be done through regulations, such as offering financial incentives or penalties for adherence to best practices in addiction treatment coverage.
- Support for Non-Profit and Community-Based Providers: Providing funding and regulatory support to non-profit or community-based addiction treatment providers can ensure individuals have access to necessary care without insurance-related barriers. These providers often serve marginalized communities and can play a key role in offering treatment without the need for PA.
7. Promoting Transparency in PA Requirements
- Transparent and Timely Communication of PA Requirements: Governments can mandate that insurance companies clearly communicate their PA requirements and approval processes to both healthcare providers and patients. This would help ensure that patients and providers know upfront whether PA is required, reducing unnecessary delays and confusion.
- Public Reporting of PA Outcomes: Requiring insurers to publicly report on PA approval rates, processing times, and denial reasons could increase accountability and encourage faster, more efficient handling of addiction treatment requests. This could motivate insurers to streamline their processes and reduce unnecessary barriers to treatment.
8. Emergency Access to Addiction Treatment
- Emergency Treatment Provisions: Governments can ensure that addiction treatment services are available on an emergency basis, allowing for immediate access to necessary care without waiting for PA. This is especially important for individuals experiencing withdrawal symptoms or those in acute crisis.
- Fast-Track Programs for High-Risk Patients: Certain high-risk populations, such as those with severe opioid use disorder or co-occurring mental health issues, could be designated for fast-track PA processes, allowing for quicker access to treatment.
Government strategies to reduce the need for prior authorization for addiction treatment focus on simplifying the approval process, expanding access to medications and services, strengthening parity laws, and incentivizing insurance reforms. By reducing bureaucratic barriers and ensuring that addiction treatment is readily available, governments can improve access to care, support long-term recovery, and address the public health crisis related to substance use disorders.
Self-Management Strategies for Navigating Prior Authorization in Addiction Treatment
Self-management strategies can help individuals navigate the challenges of prior authorization (PA) for addiction medication and therapy services by empowering them to advocate for their care, improve communication with healthcare providers, and maximize available resources. While self-management cannot eliminate the need for PA, it can reduce delays and barriers, ensuring that individuals receive timely and effective treatment.
1. Stay Informed About Insurance Coverage
- Understand Insurance Policies: Review your insurance policy to understand specific requirements for addiction treatment, including medication-assisted treatment (MAT) and therapy services. Knowing which medications and treatments require prior authorization helps in planning.
- Check for Covered Services: Confirm which medications and therapies your insurance covers. Understanding your benefits allows you to work with your provider to prescribe covered treatments and reduce the need for prior authorization requests.
2. Collaborate with Healthcare Providers
- Work Closely with Providers: Build a proactive relationship with healthcare providers, including doctors, therapists, and addiction specialists. Providers familiar with your treatment needs can navigate the PA process more efficiently.
- Prepare Documentation in Advance: Ensure your healthcare provider has all necessary documentation, such as medical records, assessments, and treatment plans, ready when submitting the prior authorization request. Complete and thorough documentation can improve the chances of approval.
- Request Evidence-Based Treatment Plans: Work with your provider to develop an evidence-based treatment plan that includes medications and therapies supported by clinical research. Insurance companies are more likely to approve treatments backed by established guidelines.
3. Advocate for Yourself
- Be an Advocate for Your Care: If you believe a particular treatment or medication is necessary, discuss this with your insurance company. Persistent advocacy can sometimes result in quicker approval or an expedited review process.
- Appeal Denials Promptly: If a prior authorization request is denied, be prepared to file an appeal. Understand the appeal process in your insurance policy and ensure that you follow it promptly. Work with your provider to submit additional documentation or medical justification.
- Know Your Rights: Familiarize yourself with federal and state laws, such as the Mental Health Parity and Addiction Equity Act (MHPAEA), which ensures addiction treatment coverage is comparable to other medical services. If your treatment is denied or delayed, you may have legal recourse.
4. Explore Alternative Treatment Options
- Consider Alternative Medications or Therapies: If a specific medication or therapy is delayed due to PA, discuss alternative options with your healthcare provider that may not require prior authorization.
- Use Generic Medications: If brand-name medications are delayed, consider generic alternatives, which may be approved more quickly. Discuss with your provider whether a generic substitute is suitable for your treatment plan.
- Seek Non-Pharmacological Approaches: Consider therapies such as cognitive-behavioral therapy (CBT), mindfulness, or support groups that may not require PA. A comprehensive approach to addiction treatment can include both medication and behavioral therapies.
5. Leverage Patient Assistance Programs
- Utilize Manufacturer Assistance Programs: Some pharmaceutical companies offer patient assistance programs that provide medications at reduced or no cost, helping reduce the financial burden of drugs subject to PA.
- Access Community Resources: Explore community resources and public health programs that offer addiction treatment without a PA, such as state-funded MAT programs, local rehabilitation centers, or non-profit organizations.
6. Keep a Record of Treatment and Correspondence
- Document All Communications: Keep a detailed record of all communications with your insurance company, healthcare providers, and other relevant parties. This includes emails, phone calls, and written correspondence, which can be helpful in case of disputes or delays.
- Track Treatment Progress: Maintain a record of your treatment progress, including medications used, therapy sessions, and any challenges encountered. This information can support justifications for continued treatment or appeals.
7. Stay Flexible and Open to Changes
- Adapt to Treatment Adjustments: Be open to adjusting your treatment plan if prior authorization is delayed or denied. Staying flexible can help you continue recovery while awaiting approval.
- Use Temporary Solutions: If a necessary treatment is delayed, ask your provider about temporary solutions to manage symptoms, such as short-term medications or alternative therapies that do not require PA.
8. Build Support Networks
- Engage in Peer Support Groups: Support groups, whether in-person or online, can offer practical advice and emotional support from others who have navigated the prior authorization process.
- Involve Family and Loved Ones: If appropriate, involve family members or loved ones in advocating for your care. They can assist in communication with your insurance company, provide emotional support, and help ensure timely access to necessary treatment.
In summary, self-management strategies can empower individuals to navigate the complexities of prior authorization for addiction treatment. By understanding insurance policies, collaborating with healthcare providers, advocating for appropriate care, and exploring alternative options, individuals can reduce the impact of PA requirements and access the treatment they need on time. Additionally, using patient assistance programs and keeping detailed records can further streamline the process, ensuring that addiction care is not unnecessarily delayed or hindered.
Family Support Strategies for Navigating Prior Authorization in Addiction Treatment
Family support plays a crucial role in helping individuals navigate the prior authorization (PA) process for addiction medication and therapy services. While family members cannot directly eliminate the need for PA, they can provide emotional support, advocate for timely access to care, and assist with the administrative aspects of the process. Below are several family support strategies to help decrease the impact of prior authorization on addiction treatment.
1. Advocate for Timely Treatment
- Assist with Communication: Family members can help by contacting insurance companies and healthcare providers to advocate for the quick processing of prior authorization requests. Ensuring that requests are submitted promptly and that required documentation is complete can prevent unnecessary delays.
- Help File Appeals: If a PA request is denied, family members can assist in gathering necessary documentation, such as medical records and treatment plans, and ensure appeals are submitted within the required timeframe.
2. Understand Insurance Policies
- Review Insurance Coverage Together: Helping the individual understand their insurance policy, including which treatments require a PA, ensures they can prepare in advance and avoid unexpected delays.
- Monitor Coverage for Addiction Treatment: Staying informed about changes in insurance policies can help family members anticipate potential PA issues and address them proactively.
3. Support the Patient’s Self-Advocacy
- Encourage Active Involvement: Support the individual in advocating for their care by encouraging them to ask about medications or therapies that may not require PA.
- Assist with Documentation: Helping maintain records of all communications with insurers and healthcare providers can be invaluable if an appeal is needed.
4. Offer Emotional and Logistical Support
- Provide Emotional Support: The PA process can be stressful. Family members can offer encouragement and reassurance, helping individuals stay focused on their recovery goals.
- Manage Logistics: Family members can help organize appointments, follow up with providers, and ensure that all necessary forms are submitted on time.
5. Work with Healthcare Providers
- Facilitate Communication: Ensuring the healthcare provider is aware of the insurer’s requirements and can provide complete documentation for the PA can improve the chances of approval.
- Ensure Treatment Plan Alignment: Working with providers to ensure that prescribed treatments align with insurance requirements can help avoid unnecessary delays.
6. Explore Alternative Treatment Options
- Encourage Flexibility: If PA delays occur, family members can support exploring alternative medications or therapies that may not require prior approval.
- Assist in Finding Public Health Programs: Researching state-funded addiction treatment programs that bypass PA requirements can help ensure continued access to care.
7. Promote Advocacy at the Policy Level
- Join Support Networks: Engaging with advocacy groups focused on addiction treatment reform can help push for systemic changes to PA processes.
- Support Legislative Efforts: Advocating for reduced PA requirements or streamlined approval processes can help decrease barriers for others in similar situations.
8. Help with Financial Support and Resources
- Identify Financial Assistance Programs: Many pharmaceutical companies and nonprofit organizations offer programs that help individuals access medications despite PA delays or high costs.
- Seek State-Funded Options: Exploring Medicaid and state-funded treatment services can provide alternative pathways to necessary care without PA hurdles.
9. Ensure Continuity of Care
- Support Ongoing Treatment During PA Delays: If PA delays interrupt treatment, family members can encourage continued participation in therapy or support groups to maintain progress.
- Prevent Relapse by Maintaining Stability: Providing a stable, supportive environment throughout the PA process can help individuals stay engaged in their recovery journey.
Family support is essential in navigating the challenges posed by prior authorization for addiction treatment. By understanding insurance policies, advocating for timely approvals, assisting with documentation, and offering emotional and logistical support, families can help reduce barriers to accessing necessary medications and therapies. Working with healthcare providers and exploring alternative treatment options can also minimize delays. With strong family involvement, individuals can stay focused on their recovery while overcoming the obstacles presented by prior authorization.
Community Resource Strategies to Reduce the Impact of Prior Authorization in Addiction Treatment
Community resource strategies can play a significant role in helping to decrease the impact of prior authorization (PA) requirements for addiction medication and therapy services. These strategies focus on creating local support systems, fostering collaboration among healthcare providers, and enhancing access to services that reduce dependency on insurance-based approval processes.
1. Develop Publicly Funded Treatment Programs
- State and Local Government-Funded Services: Community-based programs funded by state or federal agencies, such as Medicaid and SAMHSA (Substance Abuse and Mental Health Services Administration), can provide access to addiction medication and therapy services without prior authorization.
- Expand Access to Medication-Assisted Treatment (MAT): Community health centers can integrate MAT into their services, ensuring individuals receive these essential treatments quickly, bypassing the need for private insurance.
2. Promote Community Health Clinics and Non-Profit Organizations
- Access to Immediate Care through Community Health Clinics: These clinics cater to underinsured or uninsured populations and provide addiction treatment, including therapy and MAT, with minimal insurance barriers.
- Non-Profit Partnerships: Many non-profits offer addiction recovery services without requiring a PA, reducing treatment wait times.
3. Increase Collaboration Between Healthcare Providers
- Integrated Care Models: Coordinated treatment between primary care providers, addiction specialists, and mental health professionals can minimize the need for PA.
- Coordinated Treatment Plans: A well-documented treatment plan ensures smooth insurance approval and minimizes delays.
4. Leverage Telemedicine and Virtual Therapy Services
- Telemedicine for Addiction Treatment: Some insurers have fewer restrictions for telehealth services, providing quicker access to addiction care.
- Virtual Support Groups and Counseling: Online therapy and peer support groups offer essential addiction care with fewer bureaucratic hurdles.
5. Offer Education and Support for Patients and Families
- Educational Campaigns: Community organizations can provide resources to help individuals understand insurance rights and PA requirements.
- Support for Navigating the Insurance System: Case management services help individuals secure PA and appeal denials efficiently.
6. Encourage State and Local Policy Advocacy
- Advocate for Policy Change: Community groups can lobby for streamlined PA requirements or reduced insurance barriers for addiction treatment.
- Focus on Mental Health and Addiction Parity: Advocacy for more vigorous enforcement of the Mental Health Parity and Addiction Equity Act (MHPAEA) can lead to reduced PA requirements.
7. Increase Awareness and Use of Crisis and Emergency Services
- Emergency Access to Treatment: Crisis centers provide immediate addiction treatment without PA requirements.
- Crisis Stabilization Units: Emergency rooms and stabilization centers can ensure quick access to addiction care.
8. Improve Access to Affordable and Accessible Medication
- Medication Assistance Programs: Pharmaceutical programs provide reduced-cost medications to those struggling with PA delays.
- Bulk Purchasing and Discounted Medications: Community health centers can negotiate bulk purchases to lower medication costs.
9. Utilize Peer Support and Recovery Coaching
- Peer Support Networks: Groups like Narcotics Anonymous (NA) and Alcoholics Anonymous (AA) provide continuous recovery support.
- Recovery Coaches: These trained individuals assist with navigating insurance issues and ensuring adherence to treatment plans.
10. Foster Partnerships with Employers and Labor Unions
- Workplace Support for Addiction Treatment: Partnerships with employers and labor unions can create workplace policies that reduce PA requirements for addiction treatment services.
Community resource strategies play a vital role in reducing the impact of prior authorization for addiction medication and therapy services. By developing publicly funded treatment options, increasing collaboration among healthcare providers, utilizing telemedicine, and advocating for policy change, communities can ensure that individuals receive timely and effective care. Support systems, such as peer networks, recovery coaching, and educational resources, also help individuals navigate the challenges of prior authorization while maintaining their recovery journey. These strategies aim to improve access to addiction care, making it easier for individuals to overcome bureaucratic hurdles and receive the support they need.
Frequently Asked Questions
Here are some common questions:
Question: What are the ethical dilemmas with prior authorization in addiction treatment?
Answer: Prior authorization (PA) in addiction treatment raises several ethical dilemmas that impact patient care, access to treatment, and provider autonomy. Some key ethical concerns include:
1. Delays in Access to Life-Saving Treatment
- Ethical Dilemma: Addiction is a chronic, often life-threatening condition. PA requirements can delay access to medications like buprenorphine or methadone, increasing the risk of overdose, relapse, or withdrawal-related complications.
- Ethical Principle Involved: The principle of beneficence (acting in the patient’s best interest) is compromised when bureaucratic hurdles delay necessary care.
2. Discrimination and Stigma in Addiction Treatment
- Ethical Dilemma: PA requirements for addiction treatment are often more restrictive compared to other chronic conditions, reinforcing stigma and implying that addiction treatment is less medically necessary.
- Ethical Principle Involved: Justice (fair and equal treatment) is violated when addiction treatment is subject to greater scrutiny than treatments for other medical conditions.
3. Conflict Between Medical Decision-Making and Insurance Policies
- Ethical Dilemma: Physicians and addiction specialists recommend treatment based on clinical evidence, but insurance companies can override these decisions through PA denials or restrictions.
- Ethical Principle Involved: Autonomy (both patient and provider autonomy) is undermined when insurers dictate care instead of medical professionals.
4. Burden on Patients and Families
- Ethical Dilemma: Many individuals in addiction recovery struggle with financial instability, cognitive challenges, or a lack of resources. PA processes often require extensive paperwork, appeals, and follow-ups, placing undue stress on patients and their families.
- Ethical Principle Involved: Non-maleficence (not harm) is challenged when administrative barriers create harm through unnecessary stress, delays, or financial burdens.
5. Economic Incentives vs. Patient Well-Being
- Ethical Dilemma: PA is often used by insurance companies to control costs, but this may come at the expense of patient health. Denials or delays may be financially motivated rather than medically justified.
- Ethical Principle Involved: Fidelity (loyalty to patient well-being) is compromised when cost-saving measures take precedence over evidence-based treatment.
6. Impact on Vulnerable Populations
- Ethical Dilemma: PA requirements disproportionately affect marginalized populations, including low-income individuals, people experiencing homelessness, and those with limited health literacy. These individuals may struggle more with navigating PA requirements, leading to higher rates of treatment interruption.
- Ethical Principle Involved: Justice is at stake when PA requirements create disparities in access to addiction treatment.
7. Risk of Relapse Due to Treatment Gaps
- Ethical Dilemma: Many patients require uninterrupted medication-assisted treatment (MAT) to maintain recovery. Delays due to PA can lead to withdrawal symptoms and relapse, increasing overdose risk.
- Ethical Principle Involved: Non-maleficence is violated when PA policies contribute to treatment disruptions and potential harm.
8. Transparency and Accountability Issues
- Ethical Dilemma: PA decisions are often opaque, with little accountability from insurance companies regarding denials or delays. Patients and providers may struggle to understand the reasoning behind rejections, making appeals difficult.
- Ethical Principle Involved: Autonomy and justice are compromised when patients and providers lack transparency and access to transparent decision-making processes.
The ethical dilemmas surrounding PA in addiction treatment highlight the need for reforms that prioritize patient well-being over bureaucratic hurdles. Policymakers, healthcare providers, and insurers must work together to create a system that balances cost control with ethical obligations to provide timely, equitable, and effective addiction treatment.
Question: Why is prior authorization necessary to treat addiction?
Answer: Prior authorization (PA) is often required in addiction treatment for several reasons, primarily driven by cost control, safety concerns, and regulatory oversight. However, its necessity remains a contentious issue because of the delays and barriers it can cause. Here are the key reasons why insurers and healthcare systems implement PA in addiction treatment:
1. Cost Control and Utilization Management
- Insurance companies use PA to limit unnecessary spending by ensuring that treatments, especially high-cost medications, are used appropriately.
- Addiction medications like buprenorphine and extended-release naltrexone can be expensive, and insurers aim to prevent overuse or misuse by requiring prior approval.
- PA helps ensure that lower-cost alternatives are considered before approving more expensive treatments.
2. Preventing Overprescription and Misuse
- Some addiction treatment medications, such as buprenorphine, have the potential for diversion or misuse. PA requirements help monitor prescribing patterns and reduce the risk of inappropriate use.
- Insurers may require documentation to confirm that patients meet clinical criteria for certain medications or therapy services.
3. Ensuring Medical Necessity and Treatment Guidelines
- PA ensures that treatment aligns with evidence-based guidelines, requiring providers to document that a patient meets the criteria for medication-assisted treatment (MAT).
- Insurers may require proof that a patient has tried other treatment options before approving a specific medication or therapy.
4. Regulatory and Compliance Considerations
- Some addiction medications, mainly controlled substances, are subject to state and federal regulations that require additional oversight before dispensing.
- PA ensures that providers and pharmacies comply with these rules, reducing the risk of legal and regulatory violations.
5. Encouraging Coordinated and Stepwise Care
- Insurers may require PA to steer patients toward more comprehensive care, such as requiring counseling alongside MAT.
- By enforcing step therapy (where lower-cost or less-intensive treatments are tried first), PA helps insurers direct patients to standardized, phased treatment plans before escalating care.
Criticism and Challenges
While these reasons justify PA from a policy and financial perspective, many experts argue that it creates unnecessary delays, disproportionately affects vulnerable populations, and can ultimately worsen patient outcomes. Efforts to reduce PA barriers, particularly for addiction treatment, are ongoing to balance cost management with the urgent need for timely care.
Question: What can providers and patients do to prevent prior authorization for addiction treatment?
Answer: Providers and patients can take proactive steps to minimize or avoid prior authorization (PA) delays for addiction treatment. While PA is often required, strategic planning, advocacy, and knowledge of insurance policies can help streamline the process.
For Providers
- Choose Medications or Treatments Without PA Requirements
- Identify medications and therapies that do not require PA under a patient’s insurance plan.
- Some insurers may cover generic or preferred formulations without needing PA.
- Use Alternative or Low-Barrier Programs
- Consider state-funded or grant-based programs (e.g., SAMHSA-funded clinics) that do not require a PA for medications like buprenorphine or methadone.
- Submit Complete and Accurate Documentation
- Ensure all required clinical justifications, treatment plans, and past treatment attempts are well-documented.
- Use electronic prior authorization (ePA) systems to speed up processing.
- Appeal Denials Immediately
- Be prepared to challenge denials quickly by submitting appeals with supporting medical evidence.
- Use clinical guidelines, like ASAM (American Society of Addiction Medicine) criteria, to justify the necessity of treatment.
- Work with Pharmacists to Check PA Requirements in Advance
- Before prescribing, check whether a medication needs PA and explore alternative pharmacy programs that may offer coverage without insurance barriers.
- Leverage Telemedicine and Certified Programs
- Some insurers waive PA for telehealth services or in-network addiction specialists.
- Referring patients to in-network providers can sometimes eliminate PA requirements.
For Patients
- Choose an Insurance Plan with Fewer PA Barriers
- If possible, review health plan details before enrollment to check PA requirements for addiction medications and therapy.
- Look for plans that cover medication-assisted treatment (MAT) without PA.
- Request a PA Exception or Pre-Approval in Advance
- Patients can work with their provider to pre-submit PA requests before starting treatment to avoid unexpected delays.
- Some insurers allow expedited requests for urgent situations.
- Advocate for Step Therapy Waivers
- If an insurer requires step therapy (trying a lower-cost treatment first), patients can request a waiver if a prior treatment was ineffective.
- Use Manufacturer Assistance and State Programs
- Some pharmaceutical companies offer patient assistance programs that provide medication while waiting for PA approval.
- State-funded addiction treatment centers may bypass PA requirements.
- Stay Persistent with Appeals and Insurance Complaints
- If a PA request is denied, patients can file an appeal with the insurer and escalate complaints to state insurance regulators if necessary.
- Engaging patient advocacy groups can also put pressure on insurers to approve treatment.
By anticipating PA requirements and using proactive strategies, both providers and patients can reduce barriers and ensure faster access to addiction treatment.
Conclusion
While prior authorization (PA) serves to control healthcare costs, it can create significant barriers, particularly in addiction treatment, by causing delays and increasing administrative burdens. Self-management strategies, family support, and community resource initiatives offer practical ways to reduce the impact of PA. By empowering individuals to navigate the process, providing advocacy through family involvement, and utilizing publicly funded programs and integrated care, these strategies ensure more timely access to necessary treatment. Together, they help minimize the adverse effects of PA and improve overall access to care.
Video: How Insurance Delays Put Lives At Risk!