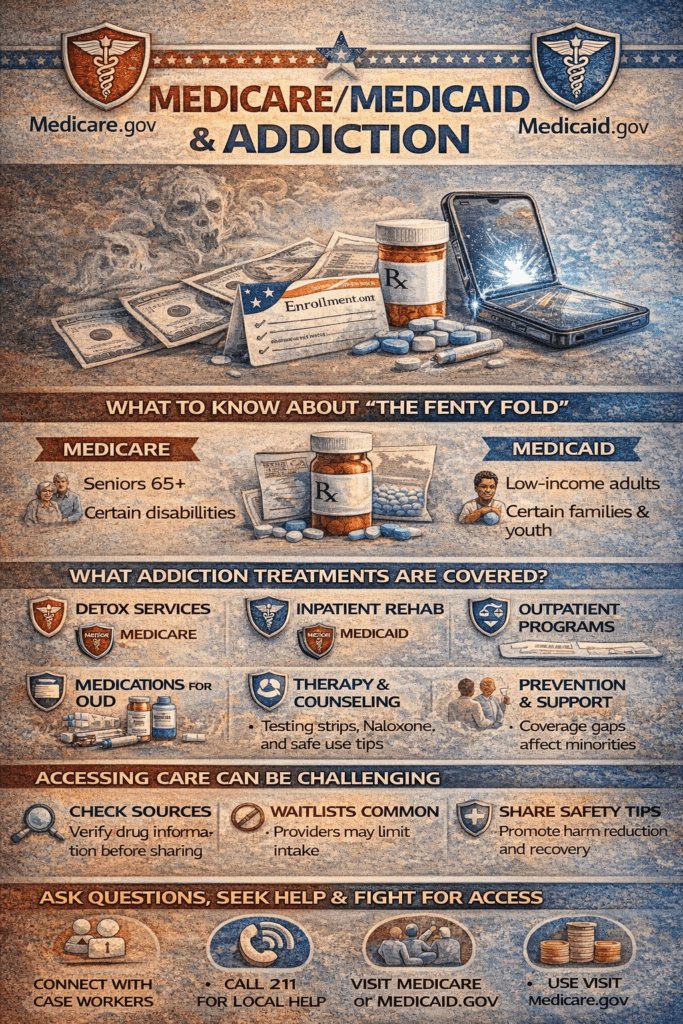
Medicare and Medicaid provide vital coverage for addiction treatment, including counseling, inpatient and outpatient care, and medication-assisted treatment. Still, barriers such as limited services, provider shortages, and administrative hurdles remain, along with ethical dilemmas regarding autonomy, confidentiality, and equitable access. When coverage falls short, alternatives such as state programs, nonprofits, sliding-scale clinics, telehealth, and peer support networks can help fill the gap.
Medicare vs. Medicaid: Addiction Treatment Coverage Explained
Both Medicare and Medicaid provide coverage for addiction treatment, though the specifics vary based on eligibility, plan type, and state regulations.
🏥 Medicare Coverage for Addiction Treatment
Medicare offers support for individuals aged 65 and older or those with qualifying disabilities:
- Inpatient Services (Part A): Covers detoxification and rehabilitation in hospitals.
- Outpatient Services (Part B): Includes therapy, counseling, and medication-assisted treatment (MAT) such as methadone, buprenorphine, and naltrexone.
- Opioid Treatment Programs (Part B): Covers services from OTPs, including medication administration and counseling.
- Medications (Part D): May cover addiction treatment medications, depending on the plan’s formulary.
⚠️ Medicare does not cover residential treatment facilities, which can limit access to some levels of care.
🏥 Medicaid Coverage for Addiction Treatment
Medicaid, a joint federal and state program, often provides broader coverage, especially in states that expanded Medicaid under the Affordable Care Act:
- Inpatient & Outpatient Services: Detoxification, rehab, therapy, and counseling.
- Residential Treatment: Some states offer waivers or programs that cover residential care.
- Medication-Assisted Treatment: Covers methadone, buprenorphine, and naltrexone, subject to state rules.
- Additional Services: May include peer support, case management, and recovery services.
📌 Coverage varies significantly by state, so check with your local Medicaid office for details.
📞 Getting Started
- Medicare Beneficiaries: Call 1-800-MEDICARE (1-800-633-4227) or visit medicare.gov.
- Medicaid Beneficiaries: Contact your state Medicaid office or visit medicaid.gov.
- National Helpline: Call SAMHSA’s Helpline at 1-800-662-HELP (4357) for free, confidential treatment referrals.
In summary, Medicare and Medicaid both cover essential addiction treatment services, but benefits vary. Understanding these differences—and checking your state’s rules—can help individuals access the proper care at the right time.
Barriers to Addiction Treatment Under Medicare and Medicaid
Medicare and Medicaid play a critical role in expanding access to addiction treatment, but many patients still face significant barriers. These challenges can be systemic, logistical, or patient-related, preventing individuals from fully benefiting from available coverage.
1. Limited Coverage for Certain Services
- Medicare: Does not typically cover long-term residential rehabilitation programs, which are often crucial for severe addiction. Outpatient therapy sessions may also be limited.
- Medicaid: Coverage varies by state, so services such as specific MAT options, peer support, or residential care may not be consistently available.
2. Provider Shortages
- Few providers accept Medicare or Medicaid because reimbursement rates are lower than those for private insurance.
- Specialized addiction treatment providers—especially for MAT—are scarce in rural or underserved areas.
3. Administrative Hurdles
- Many services require prior authorization or extensive paperwork, delaying care.
- These bureaucratic processes can discourage both providers and patients from pursuing treatment.
4. Stigma and Lack of Awareness
- Many patients do not realize that addiction treatment is covered under Medicare and Medicaid.
- Social stigma surrounding substance use often prevents individuals from seeking care even when coverage exists.
5. Limited Mental Health Integration
- Addiction frequently co-occurs with mental health disorders, yet integrated treatment is inconsistent.
- Patients may struggle to access coordinated care for both conditions simultaneously.
6. Geographic and Transportation Barriers
- Treatment facilities are often far from patients’ homes, especially in rural areas.
- Medicare and Medicaid may not cover transportation, further limiting access.
7. Restrictions on Medication-Assisted Treatment (MAT)
- Some plans require step therapy or restrict certain medications.
- Methadone is typically covered only through specialized OTPs, reducing treatment flexibility.
8. Gaps in Preventive and Recovery Support
- Essential long-term supports like peer counseling, case management, and recovery coaching may not be fully covered.
In summary, while Medicare and Medicaid provide vital coverage for addiction treatment, barriers such as limited services, provider shortages, administrative delays, geographic challenges, and stigma continue to block access. To make these programs truly effective, reforms are needed to improve coverage consistency, expand provider participation, and integrate recovery-focused services.
Ethical Dilemmas in Using Medicare and Medicaid for Addiction Treatment
Using Medicaid and Medicare for addiction treatment provides vital support, but it also raises complex ethical dilemmas. These often involve questions of access, fairness, patient autonomy, and systemic limitations.
1. Equity and Access
- Medicaid variation: Coverage differs by state, leading to unequal access to essential services.
- Provider shortages: Patients in rural or underserved areas may find few providers accepting Medicare or Medicaid, raising fairness concerns.
2. Resource Allocation
- Funding is limited, and prioritizing specific treatments or populations raises ethical questions about who receives care first.
- Balancing costly services—like long-term rehab—against broader population needs remains a challenge.
3. Autonomy vs. Oversight
- Prior authorization, mandatory documentation, and coverage rules may feel restrictive.
- Patients can feel their autonomy is compromised when insurance dictates available services or medications.
4. Confidentiality
- Coordinated care often requires sharing sensitive information among multiple providers and agencies.
- This raises privacy concerns, especially with billing and authorization processes.
5. Stigma and Discrimination
- Patients with public insurance may face stigma or bias, which can affect the quality of care they receive.
- Ethical dilemmas emerge when systemic disparities reinforce existing inequities.
6. Mandates and Incentives
- Some programs require treatment participation to maintain benefits.
- This creates tension between promoting recovery and respecting individual choice.
7. Access to Innovative or Experimental Treatments
- Medicare and Medicaid may not cover newer or less-established therapies.
- Patients may be denied promising options due to policy restrictions rather than medical need.
In summary, ethical dilemmas in Medicare and Medicaid addiction treatment reflect a balancing act: ensuring equity, respecting autonomy, protecting privacy, and managing limited resources, all while addressing stigma and systemic barriers. Recognizing these challenges is the first step toward designing policies that support both recovery and fairness.
Alternatives When Medicare and Medicaid Don’t Fully Cover Addiction Treatment
While Medicare and Medicaid provide essential coverage for addiction treatment, gaps remain. When these programs cannot fully meet needs, individuals can turn to alternative resources and strategies to access care.
1. State and Local Programs
- Many states fund substance use disorder (SUD) programs through state budgets or federal block grants.
- Local health departments may offer free or low-cost counseling, detox, or outpatient services.
2. Nonprofit and Community-Based Organizations
- Groups such as Salvation Army Adult Rehabilitation Centers, Catholic Charities, and local nonprofits provide free or sliding-scale treatment.
- Peer-led networks like SMART Recovery and 12-step groups offer no-cost guidance and community support.
3. Sliding-Scale or Low-Cost Clinics
- Some treatment centers adjust fees based on income.
- Federally Qualified Health Centers (FQHCs) often provide addiction counseling and behavioral health care at reduced rates.
4. Telehealth and Online Programs
- Virtual counseling platforms and telemedicine services can lower costs for therapy, support groups, and MAT consultations.
- Some online programs offer scholarships or self-pay discounts for those without coverage.
5. Employer Assistance Programs (EAPs)
- Many workplaces provide confidential support, counseling, and treatment referrals to employees dealing with substance use.
6. Scholarships, Grants, or Charitable Funds
- Nonprofit foundations and treatment programs sometimes offer financial assistance for residential or outpatient care.
7. Harm Reduction and Community Health Resources
- Needle exchange programs, naloxone distribution sites, and harm reduction clinics provide safety, education, and treatment referrals.
- Community mental health centers often support individuals with co-occurring mental health and substance use disorders.
8. Peer and Family Support Networks
- Groups like Al-Anon, Nar-Anon, and recovery coaching programs help both individuals and families manage the challenges of addiction.
In summary, even if Medicare or Medicaid cannot fully cover addiction treatment, individuals are not without options. State programs, nonprofits, sliding-scale clinics, telehealth, employer assistance, charitable funds, harm reduction services, and peer networks together create a broad safety net. These alternatives can help bridge coverage gaps and ensure access to essential recovery services.
Frequently Asked Questions
Here are some common questions:
Question: Provide a table of Medicare vs. Medicaid barriers for addiction treatment.
Answer: A concise table of Medicare vs. Medicaid barriers for addiction treatment:
| Coverage depends on the state; it may be limited or not fully funded | Medicare | Medicaid |
|---|---|---|
| Limited Coverage | Long-term residential rehab usually not covered; outpatient limits on therapy sessions | Coverage varies by state; some MAT, residential, or peer support services may be limited |
| Provider Shortages | Fewer providers accept Medicare; limited specialized addiction providers | Lower reimbursement rates; scarcity of MAT providers, especially in rural areas |
| Prior Authorization / Administrative Hurdles | Requires documentation and approvals for many services | State-specific rules and approvals can delay care |
| Stigma / Awareness | Patients may not know treatment is covered | Patients may avoid treatment due to stigma despite coverage |
| Mental Health Integration | Co-occurring mental health care often fragmented | Coordination of addiction and mental health services varies by state |
| Geographic / Transportation Barriers | Access limited in rural areas; transportation not covered | Rural and underserved areas may lack facilities; transportation coverage varies |
| MAT Restrictions | Some medications require prior authorization; methadone limited to OTPs | State-specific restrictions; step therapy or limits on certain MAT medications |
| Limited Recovery Support Services | Peer support, case management often not covered | Coverage depends on state; may be limited or not fully funded |
This table provides a clear comparison of the key barriers patients face under each program, useful for educational materials, policy discussions, or planning treatment access.
Question: Provide a guide to alternative resources for addiction treatment when Medicare or Medicaid cannot fully cover care:
Answer: A practical guide to alternative resources for addiction treatment when Medicare or Medicaid cannot fully cover care:
Alternative Resources for Addiction Treatment
1. State and Local Programs
- What they offer: Detox, outpatient therapy, case management, and prevention programs.
- How to access: Contact your state health department or local behavioral health agency.
2. Nonprofit and Community-Based Organizations
- Examples: Salvation Army Adult Rehabilitation Centers, Catholic Charities, and local recovery nonprofits.
- Services: Free or low-cost residential treatment, counseling, and peer support.
3. Sliding-Scale or Low-Cost Clinics
- Federally Qualified Health Centers (FQHCs) provide behavioral health and addiction services based on income.
- Ask local clinics about sliding-scale fees for counseling or MAT.
4. Telehealth and Online Programs
- What they offer: Virtual therapy, support groups, and MAT consultations at a lower cost.
- How to access: Search for licensed online counseling platforms or telemedicine addiction services.
5. Employer Assistance Programs (EAPs)
- Services: Confidential counseling, short-term therapy, and treatment referrals.
- How to access: Contact your human resources department to learn about available EAP benefits.
6. Scholarships, Grants, or Charitable Funds
- Some treatment centers and nonprofit foundations provide financial assistance for residential or outpatient care.
- Check with local rehab centers or online databases for addiction treatment scholarships.
7. Harm Reduction and Community Health Resources
- Services: Needle exchanges, naloxone distribution, overdose prevention, and support for safe recovery practices.
- Often provide referrals to treatment programs and counseling.
8. Peer and Family Support Networks
- Examples: AA, NA, SMART Recovery, Al-Anon, Nar-Anon.
- Benefits: Emotional support, recovery guidance, and community accountability.
Tips for Accessing These Resources:
Keep track of appointments, referrals, and contacts in a recovery notebook or app.
Make a list of available local and online programs.
Contact organizations directly to ask about cost, services, and eligibility.
Combine multiple resources (e.g., peer support + sliding-scale clinic) to cover all aspects of care.
Question: Where do Medicare and Medicaid get resources to provide addiction care?
Answer: Medicare and Medicaid fund addiction care from several sources, but the pathways differ:
Medicare
- Payroll Taxes & Premiums: Medicare Part A (hospital insurance) is mainly funded by payroll taxes from workers and employers. Parts B and D (outpatient and prescription drug coverage) are financed through enrollee premiums and federal revenues.
- Federal General Revenues: A large share of Medicare’s funding comes directly from the U.S. Treasury.
- These resources are then used to reimburse providers for addiction-related services such as hospital stays, outpatient visits, and medication-assisted treatment.
Medicaid
- Joint Federal–State Funding: Medicaid is financed through both federal and state tax dollars. The federal government matches state spending at a rate (FMAP) that ranges from ~50% to over 70%, depending on the state’s income level.
- State Contributions: States raise funds through their own tax systems (income, sales, or other taxes).
- States then allocate this funding toward approved services, which can include detox, counseling, rehab, and recovery support.
In summary, Medicare’s resources come from federal payroll taxes, premiums, and Treasury revenues, while Medicaid’s come from a federal-state partnership of tax dollars.
Conclusion
Medicare and Medicaid play a critical role in making addiction treatment accessible, but challenges such as service limitations, provider shortages, administrative hurdles, and ethical dilemmas can hinder care. Awareness of these barriers is essential for patients and providers to navigate the system effectively. When coverage is insufficient, alternative resources—including state programs, nonprofits, sliding-scale clinics, telehealth, and peer support networks—offer valuable options to ensure individuals receive the treatment and support necessary for recovery.
Video: 5 SHOCKING Truths About Medicare Medicaid Addiction Treatment