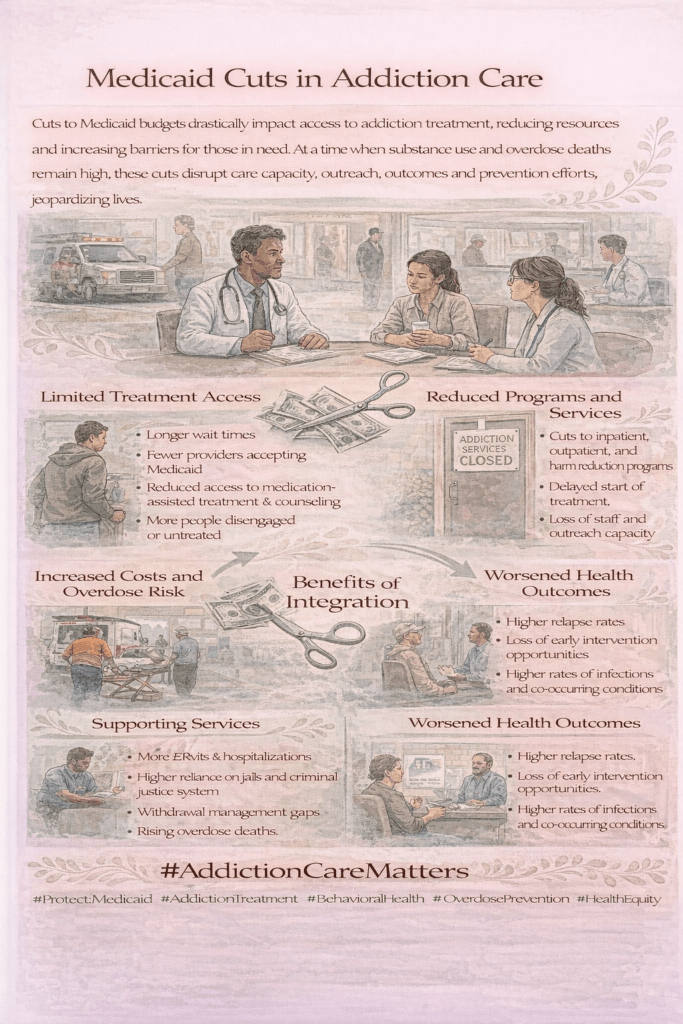
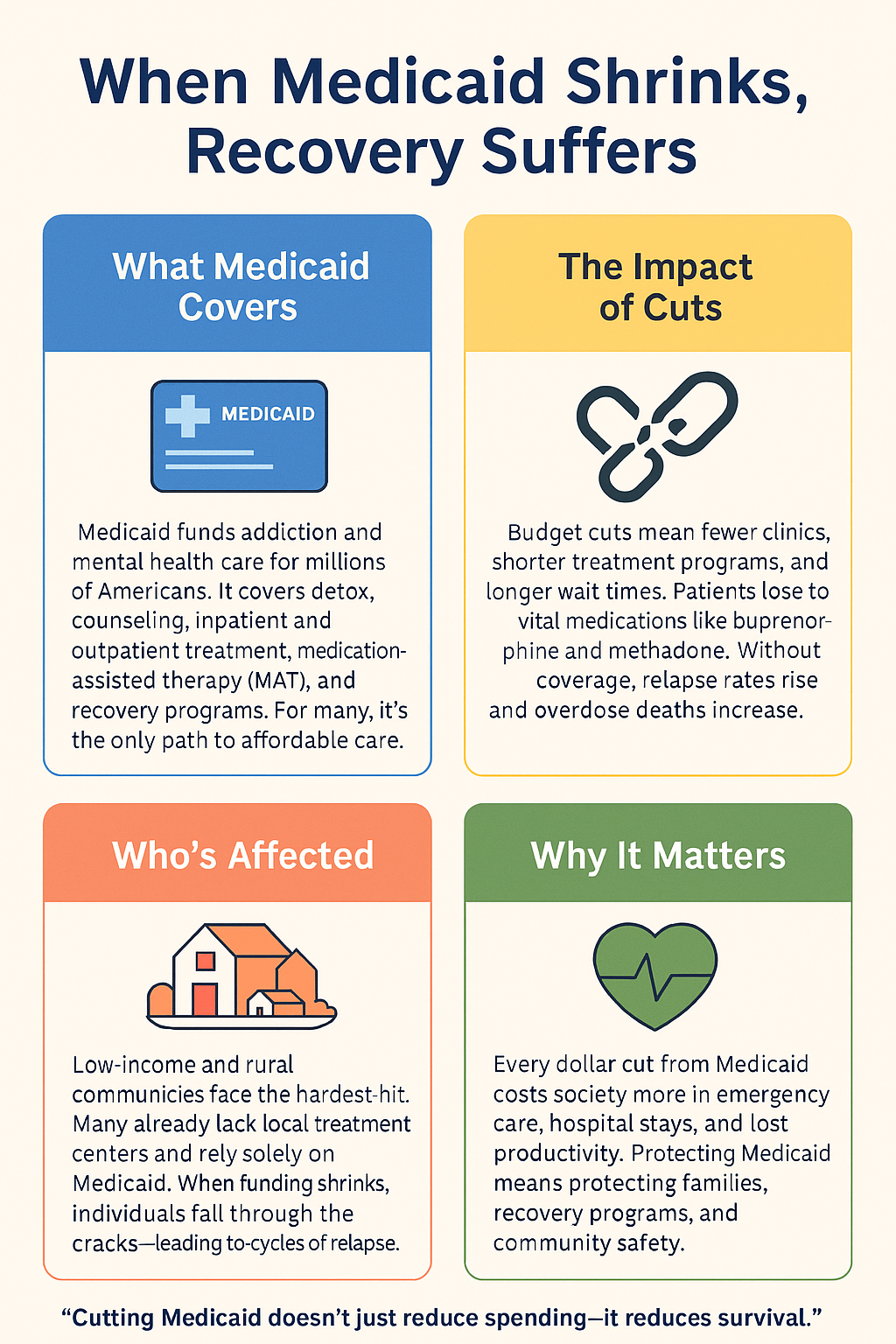
Medicaid cuts significantly reduce access to vital mental health and addiction services, placing some of the most vulnerable individuals at heightened risk for untreated illness, relapse, and overdose. Many people with substance use disorders and serious mental health conditions rely on Medicaid for medications, therapy, inpatient and outpatient treatment, and recovery supports. When funding is reduced, services are often limited through stricter eligibility rules, fewer covered treatments, provider shortages, and longer wait times. These gaps can interrupt continuity of care at critical moments, such as after hospitalization, incarceration, or during early recovery. Despite these challenges, access is not determined solely by policy. State-level decisions, individual self-management strategies, family advocacy, and community-based resources play an essential role in mitigating harm. By strengthening coordination across healthcare systems, empowering families to advocate for care, supporting patient self-navigation, and expanding community partnerships, it is possible to bridge treatment gaps and protect access to lifesaving mental health and addiction services even amid funding constraints.
How Medicaid Cuts Endanger Mental Health and Addiction Treatment
Medicaid cuts can have profound and far-reaching effects on mental health and addiction treatment, especially for low-income and vulnerable populations who depend on it for essential care. Here’s how these changes impact individuals and communities:
1. Reduced Access to Care
Cuts often lead to fewer covered services, stricter eligibility requirements, and longer wait times—making it harder for people to get therapy, medication, or inpatient treatment for mental health or substance use disorders.
2. Loss of Coverage for Vulnerable Groups
Many living with mental illness or addiction are unemployed or earn low wages. Medicaid cuts can disqualify them from coverage, leaving them untreated and at higher risk for relapse, hospitalization, or incarceration.
3. Fewer Providers Accepting Medicaid
Lower reimbursement rates can discourage providers from taking Medicaid patients. This limits care options, especially in rural or underserved areas where provider shortages already exist.
4. Disruption of Ongoing Treatment
Treatment plans like therapy sessions, medication-assisted treatment (MAT), or recovery support rely on consistency. Cuts can interrupt these services, increasing the risk of relapse, overdose, or mental health crises.
5. Strain on Emergency and Public Health Systems
Without preventive and ongoing care, more individuals turn to emergency rooms, jails, or shelters—driving up public costs while worsening overall health outcomes.
6. Reduced Funding for Community Programs
Medicaid supports many community-based programs for mental health and addiction recovery. Cuts can lead to program closures, reducing access to crisis intervention, peer support, and outreach services.
In summary, Medicaid cuts weaken the foundation of mental health and addiction care by limiting access, disrupting continuity, and lowering quality. The result is increased suffering for individuals and families—and higher long-term costs for society as a whole.
8 State Policy Strategies to Protect Mental Health and Addiction Care Amid Medicaid Cuts
State governments can take action to reduce the harm of Medicaid cuts on mental health and addiction treatment. By using innovative policy tools, they can protect access, sustain service quality, and safeguard vulnerable populations—even during budget shortfalls.
1. Expand Medicaid Under the Affordable Care Act (ACA)
Expanding Medicaid eligibility allows states to access federal matching funds, increasing coverage while lowering the state’s financial burden.
2. Use Medicaid Waivers (e.g., 1115 or 1915(c))
Waivers give states flexibility to redesign Medicaid programs and fund addiction treatment, mental health services, housing supports, and peer recovery programs in more targeted ways.
3. Increase Reimbursement Rates for Behavioral Health Providers
Fair payment encourages providers to accept Medicaid patients and sustain services despite budget pressures.
4. Integrate Behavioral and Physical Health Services
Coordinating care between mental health, addiction, and primary care providers—primarily through value-based care models—improves outcomes and reduces costs.
5. Invest in Community-Based and Preventive Services
Shifting toward early intervention, telehealth, crisis stabilization, and harm reduction is cost-effective and can prevent more expensive emergency care down the road.
6. Leverage Federal Grants and Partnerships
Applying for funds from SAMHSA, HRSA, and CDC can help fill Medicaid funding gaps and support targeted treatment and recovery programs.
7. Protect Essential Health Benefits in State Law
States can require insurers—including Medicaid-managed care—to cover mental health and addiction services as essential benefits, regardless of federal policy changes.
8. Enhance Data Tracking and Accountability
Using state data to monitor service gaps, health outcomes, and spending efficiency ensures limited funds are directed where they’re most needed.
In summary, even when Medicaid budgets are cut, states have the power to maintain—and even strengthen—mental health and addiction care. By combining expansion, innovation, and legislative protection, they can support recovery, improve public health, and avoid the long-term costs of untreated illness.
10 Self-Management Strategies for Addiction Treatment During Medicaid Cuts
Even with Medicaid cuts, individuals can take proactive steps to navigate the healthcare system and continue accessing addiction treatment. By exploring alternative coverage, using community resources, and advocating for themselves, people can maintain essential care and recovery support.
1. Explore All Eligibility Options
- Reapply or update Medicaid information—you may still qualify under different criteria (e.g., disability, pregnancy, low income).
- Check for Medicaid expansion in your state or marketplace subsidies through the ACA.
2. Apply for Sliding Scale or Charity Care Programs
- Many clinics and treatment centers provide income-based fees, payment plans, or free services supported by grants or donations.
3. Use Federally Qualified Health Centers (FQHCs)
- FQHCs often deliver low-cost or free addiction and mental health services regardless of insurance status.
4. Seek Support From Recovery Peer Networks
- Peer recovery coaches and groups can help you navigate applications, find free programs, and connect with local resources.
5. Contact Local Health Departments
- They may provide publicly funded treatment, referrals, or vouchers for detox, MAT, or outpatient programs.
6. Utilize Telehealth and Online Services
- Many virtual providers offer lower-cost treatment and financial assistance for uninsured individuals.
7. Apply for Emergency Medicaid or Short-Term Coverage
- In crises, you may qualify for emergency Medicaid if hospitalized or in urgent need of care.
8. Advocate for Yourself
- Be persistent with providers, case managers, and social workers. Ask about alternative funding sources, nonprofit help, or state-specific programs.
9. Keep Medical Documentation Organized
- Maintain a record of your health history, treatment needs, and authorizations to strengthen your case when applying for aid.
10. Connect With Legal Aid or Health Navigators
- These professionals can appeal coverage denials, assist with applications, and identify alternative care programs.
In summary, while Medicaid cuts create obstacles, individuals can still take charge of their recovery. Through education, resourcefulness, and strong support networks, these self-management strategies can help maintain access to critical addiction treatment services—even in uncertain policy environments.
10 Ways Families Can Support Loved Ones in Addiction Treatment During Medicaid Cuts
Families play a vital role in helping their loved ones access addiction treatment, especially during times of Medicaid cuts. By becoming informed advocates and resource navigators, families can help secure therapy through a variety of strategies:
1. Assist With Applications and Renewals
- Help complete Medicaid or health marketplace applications. Even minor paperwork errors can cause delays or denials.
2. Explore Alternative Coverage Options Together
- Check if your loved one qualifies under other Medicaid categories (disability, pregnancy, youth), ACA subsidies, or veterans’ benefits.
3. Research Low-Cost or Free Treatment Programs
- Look into state-funded, nonprofit, or faith-based programs that offer sliding-scale or free care.
- Contact local health departments for referrals or block-grant-funded services.
4. Advocate With Providers and Case Managers
- Attend treatment planning meetings, ask about financial assistance, and push for access to care despite coverage gaps.
5. Help With Transportation and Scheduling
- Assist with travel and appointment coordination, which can be crucial for meeting intake and application requirements.
6. Connect With Peer and Parent Support Groups
- Join family recovery or advocacy groups that share information, resources, and strategies for navigating treatment access.
7. Contact Legal Aid or Health Navigators
- Reach out to professionals who can appeal Medicaid denials or guide families toward alternative funding sources.
8. Encourage Self-Advocacy
- Support your loved one in tracking medical documentation, voicing their needs, and asking for help from case managers or providers.
9. Fundraise or Apply for Temporary Assistance
- Explore local charities, crowdfunding platforms, or short-term aid programs to help cover urgent treatment needs.
10. Monitor Policy Changes and Opportunities
- Stay updated on Medicaid expansions, new waivers, or emergency state funding that may restore access to treatment.
In summary, families can be powerful advocates during Medicaid cuts by helping with applications, finding alternative resources, and collaborating with providers. With persistence and creativity, families can play a critical role in ensuring their loved ones continue receiving the addiction treatment they need.
10 Community Resource Strategies to Support Addiction Treatment During Medicaid Cuts
Community resource strategies are essential in helping individuals access addiction treatment when Medicaid cuts threaten care. Local organizations, nonprofits, and government-supported services can bridge the gap by providing funding, support, and advocacy. Here are ten key strategies:
1. Federally Qualified Health Centers (FQHCs)
These centers offer low-cost or free addiction and mental health services regardless of insurance status, including medication-assisted treatment (MAT).
2. State and Local Health Departments
States often use block grant funding (e.g., SAMHSA funds) to support treatment programs for the uninsured or underinsured. They can provide referrals, vouchers, or sliding-scale detox and recovery programs.
3. Nonprofit and Faith-Based Treatment Providers
Organizations such as the Salvation Army, Catholic Charities, and local recovery missions frequently provide free or subsidized treatment, housing, and support services.
4. Recovery Community Organizations (RCOs)
These peer-led groups guide individuals through treatment navigation, applications, and recovery coaching. They also collaborate with local providers to expand support networks.
5. Health Insurance Navigators and Legal Aid Services
Navigators help people apply for coverage, appeal Medicaid denials, or transition to marketplace plans. Legal aid services assist with eligibility disputes and access to care.
6. Community Mental Health Centers
Funded by states and grants, many centers provide substance use disorder treatment for those who are uninsured or underinsured.
7. Educational and Job Training Programs
Some community centers combine addiction recovery with employment or housing support, often covered through alternative public funding streams.
8. Community Coalitions and Advocacy Groups
These groups advocate for funding, organize resource fairs, and raise awareness of available services during budget cuts or policy transitions.
9. Harm Reduction Organizations
Though not a substitute for complete treatment, harm reduction groups provide naloxone, counseling referrals, and bridge services while individuals pursue comprehensive care.
10. Telehealth and Virtual Care Networks
Community-funded telehealth programs offer affordable virtual counseling and MAT services, reducing barriers tied to cost and geography.
In summary, community-based organizations are a lifeline when Medicaid cuts occur. Through flexible funding, outreach, and coordinated care, they help ensure that individuals don’t fall through the cracks and can continue their recovery journey.
Frequently Asked Questions
Here are some common questions:
Question: How do the Medicaid cuts affect drug prices?
Answer: Medicaid cuts don’t directly set or change the price of drugs on the market (pharmaceutical companies set list prices), but they can affect how much patients and states pay for them and how accessible they are. Here’s how:
1. Reduced Negotiating Power
- Medicaid is one of the largest purchasers of prescription drugs in the U.S.
- With fewer enrollees (because of cuts), the state may lose some bargaining leverage with pharmaceutical companies, making it harder to secure deep discounts.
2. Changes to the Medicaid Drug Rebate Program
- By law, drug manufacturers must give rebates to Medicaid for covered medications, lowering the cost for states.
- If Medicaid enrollment shrinks, fewer prescriptions qualify for these rebates, which can drive up per-patient costs.
3. More Out-of-Pocket Spending for Patients
- When individuals lose Medicaid coverage, they may have to pay retail prices for addiction medications (like buprenorphine, methadone, or naltrexone) or psychiatric meds, which are often very expensive.
- Some may shift to cheaper, less effective medications—or skip treatment entirely.
4. Shifts to State or Local Budgets
- Without Medicaid covering much of the cost, states and local governments may need to rely on block grants or emergency funds to provide addiction-related medications.
- This can limit supply and force rationing of treatment programs.
5. Indirect Pressure on Market Prices
- While Medicaid cuts don’t usually raise drug list prices, they can reduce the number of people receiving discounted coverage.
- That means more people pay higher retail or insurance-based costs, and manufacturers face less pressure to offer rebates to keep net prices lower.
✅ In short: Medicaid cuts don’t usually change drug list prices, but they reduce discounts, weaken negotiating power, and shift more costs to patients and states. For people needing addiction treatment, that often means higher out-of-pocket costs and reduced access to life-saving medications.
Question: How do Medicaid cuts affect accessibility for addiction treatment?
Answer: Medicaid cuts can seriously reduce accessibility to addiction treatment because Medicaid is the single largest payer for substance use disorder (SUD) services in the U.S. Here’s how:
1. Loss of Coverage
- Many people with addiction are low-income and rely on Medicaid. Cuts may make them ineligible or cause certain benefits to be dropped, leaving them uninsured.
- Without coverage, the cost of detox, residential care, or medication-assisted treatment (MAT) becomes unaffordable.
2. Fewer Treatment Options
- If Medicaid stops covering certain services (such as residential treatment beyond a set number of days or specific medications), patients lose access to the full continuum of care.
- Essential services like counseling, recovery housing, or peer support may be cut back.
3. Reduced Provider Participation
- Cuts often come with lower reimbursement rates for providers.
- Many treatment centers and clinics may stop accepting Medicaid, especially in rural or underserved areas, shrinking the treatment network.
4. Longer Wait Times
- With fewer funded treatment slots available, people often face weeks or months-long delays for detox beds, therapy, or MAT.
- This delay increases the risk of relapse, overdose, or dropping out of treatment.
5. Disruption of Ongoing Care
- Cuts can interrupt people already in treatment if programs lose funding.
- Stopping MAT or counseling abruptly can cause withdrawal, relapse, or even fatal overdoses.
6. Greater Reliance on Emergency Systems
- Instead of receiving steady, preventive treatment, people may only access care in crisis—through ERs, jails, or shelters—where outcomes are worse, and costs are higher.
✅ In summary: Medicaid cuts reduce who can get care, what services are covered, which providers are available, and how quickly people can enter treatment. The result is fewer people able to access or sustain life-saving addiction care, and more strain on families and public systems.
Question: How do Medicaid cuts affect accessibility to hospital services due to addiction?
Answer: Hospital services are often the safety net for people with addiction when outpatient or community treatment isn’t accessible. Medicaid cuts affect hospital-based care in several ways:
1. Higher Uncompensated Care Burden
- Many individuals with addiction rely on Medicaid for emergency visits, detox, or psychiatric stabilization.
- If they lose coverage, hospitals must absorb costs for uninsured patients.
- This financial strain can lead hospitals to cut back addiction-specific services like detox units or psychiatric beds.
2. Reduced Access to Emergency Detox and Stabilization
- Medicaid often covers emergency department (ED) visits, detox protocols, and short inpatient stays for withdrawal or overdose.
- Cuts may limit coverage for repeat ED visits or specialized addiction services, reducing accessibility for patients in crisis.
3. Fewer Hospital-Based Addiction Programs
- Many hospitals run medication-assisted treatment (MAT) initiation programs (e.g., starting buprenorphine in the ED).
- With less Medicaid reimbursement, hospitals may downsize or eliminate these programs, leaving patients without a “warm handoff” into recovery care.
4. Staffing and Resource Reductions
- Cuts lower reimbursement rates, making it difficult for hospitals to fund addiction-trained staff (psychiatrists, social workers, peer recovery coaches).
- This reduces the quality and availability of inpatient and consult services for patients with SUD.
5. Increased ER Overcrowding
- When outpatient and community programs shrink due to Medicaid cuts, more people turn to hospitals as their only option.
- This leads to longer wait times, overcrowding, and rushed care for both addiction-related and general emergencies.
6. Worse Continuity of Care
- Medicaid usually covers post-discharge services like outpatient follow-up, medication, or counseling.
- Without it, patients discharged after overdose or detox may have no affordable next step—raising the chance of relapse and readmission.
✅ In summary: Medicaid cuts reduce hospitals’ ability to provide detox, inpatient stabilization, and recovery support services. They also push more uninsured patients into emergency care without covering costs, which can force hospitals to scale back or eliminate addiction programs. The result is reduced accessibility, higher strain on ERs, and more treatment gaps for people with substance use disorders.
Conclusion
Medicaid cuts to mental health and addiction services can profoundly impact access to care, but strategic responses can help reduce harm. State governments play a key role by enacting supportive policies and funding alternatives. Individuals can manage their care through informed choices, while families provide vital advocacy and emotional support. Community organizations also help bridge service gaps with affordable, accessible programs. Together, these efforts work to protect recovery pathways despite financial challenges.
Video: The SHOCKING Truth About Medicaid Cuts and Addiction Care