Access to affordable opioid use disorder (OUD) treatment is crucial for addressing the public health challenges posed by opioid addiction. Government interventions are pivotal in shaping policies and initiatives to improve access to low-cost OUD treatment options. However, barriers such as financial constraints, regulatory complexities, stigma, and healthcare disparities hinder effective implementation. Community resource strategies, including peer support programs, harm reduction services, and community health centers, are essential in overcoming these challenges and enhancing treatment accessibility. These initiatives are instrumental in supporting individuals affected by opioid addiction on their path to recovery and promoting a more inclusive healthcare system.
Enhancing Access to Treatment: The Impact of Low-Cost Strategies for Opioid Use Disorder (OUD)
Low-cost opioid use disorder (OUD) treatment can significantly improve access and treatment outcomes through several key strategies. By addressing financial barriers and promoting innovative care approaches, these initiatives can pave the way for a healthier future for individuals struggling with OUD.
1. Affordability
One of the primary benefits of low-cost treatment options is the reduction or elimination of financial barriers. By making OUD medications and counseling more accessible, individuals from all economic backgrounds are encouraged to seek treatment and adhere to prescribed therapies. This affordability is crucial for increasing the number of people willing to enter recovery.
2. Expansion of Provider Network
Low-cost treatment initiatives can incentivize a broader range of healthcare providers to participate in OUD treatment. This includes primary care physicians, nurse practitioners, and physician assistants, who may not traditionally specialize in addiction treatment but can now provide effective care without imposing a heavy financial burden on patients. A diversified provider network enhances access and fosters a more supportive environment for recovery.
3. Integration into Primary Care
Integrating OUD treatment into primary care settings lowers costs and enhances patient convenience. Routine medical visits can be used to screen for, diagnose, and manage OUD alongside other chronic health conditions. This holistic approach promotes comprehensive care and improves treatment adherence, as patients can address multiple health issues in one visit.
4. Telemedicine and Remote Services
Leveraging telemedicine and remote services can reduce the overhead costs associated with in-person visits while extending treatment options to rural or underserved areas. Patients can access medication-assisted treatment (MAT), counseling, and monitoring remotely, enhancing convenience and significantly reducing barriers to regular care. This innovative approach is especially beneficial for individuals with transportation challenges or those living in remote locations.
5. Community-Based Support Programs
Low-cost initiatives can support community-based programs that offer peer counseling, group therapy, and harm reduction services. These programs complement medical treatment by providing emotional support, practical guidance, and resources for individuals in recovery from OUD. Community engagement fosters a sense of belonging and accountability, which can be crucial for long-term recovery.
6. Public Health Initiatives
Government-funded public health campaigns can raise awareness about OUD treatment options, reduce stigma, and encourage early intervention. These efforts promote a supportive environment for seeking treatment, thereby improving overall community health outcomes. By informing the public about the availability of low-cost treatment, more individuals may feel empowered to pursue recovery.
7. Streamlined Access and Navigation
Simplifying access to treatment is vital. Streamlined intake procedures and navigation services help individuals quickly connect with the care they need, reducing delays in treatment initiation. By improving the overall patient experience, these strategies enhance retention in care, ensuring individuals receive the support they need throughout their recovery journey.
8. Medication Accessibility
Ensuring consistent availability and affordability of OUD medications through government subsidies, negotiated pricing agreements, or generic alternatives is essential for improving treatment continuity and patient outcomes. When patients can reliably access the medicines they need, they are more likely to stay engaged in their recovery.
By implementing these strategies, low-cost OUD treatment initiatives can expand access to care, improve treatment retention rates, reduce overdose deaths, and support long-term recovery efforts for individuals affected by opioid use disorder. Collaborative efforts among healthcare providers, policymakers, and communities can create a more inclusive and supportive environment for those on the path to recovery. With a focus on affordability, accessibility, and comprehensive care, we can foster a brighter future for individuals battling OUD.
Strategies for Governments to Provide Low-Cost Treatment for Opioid Use Disorder (OUD)
Governments play a crucial role in combating the opioid epidemic and improving access to treatment for opioid use disorder (OUD). Implementing low-cost strategies can enhance treatment outcomes and facilitate recovery for individuals struggling with addiction. Here are several practical approaches that policymakers can consider:
1. Funding and Subsidies
Governments can allocate public funding or subsidies to reduce the cost of essential OUD medications such as buprenorphine, methadone, and naltrexone. This may involve providing direct financial support to treatment providers or negotiating pricing agreements with pharmaceutical companies. Individuals are more likely to seek and maintain treatment when medications are more affordable.
2. Insurance Coverage Expansion
Expanding Medicaid coverage or requiring private insurance plans to cover OUD treatment—including medications and counseling—can significantly improve access. Ensuring minimal out-of-pocket costs for patients allows individuals from various economic backgrounds to receive the treatment they need, regardless of their insurance status.
3. Telemedicine and Remote Services
Establishing policies that support telemedicine and remote services for OUD treatment can reduce travel costs and improve patient convenience, particularly in rural or underserved areas. Reimbursement frameworks should be developed to encourage healthcare providers to offer medication-assisted treatment (MAT), counseling, and monitoring remotely, making it easier for individuals to access care.
4. Provider Incentives and Training
Offering financial incentives or grants to healthcare providers who incorporate OUD treatment into their practices can expand access to care. These funds can support training in evidence-based addiction treatment practices, including the effective use of medications and behavioral therapies. A well-trained workforce can enhance treatment outcomes for individuals struggling with OUD.
5. Integration into Primary Care
Integrating OUD treatment services into primary care settings can lower costs associated with specialty addiction treatment centers. This holistic approach allows individuals with co-occurring medical conditions to receive comprehensive care in one location, leading to better health outcomes and improved treatment adherence.
6. Community-Based Initiatives
Government support for community-based initiatives—such as peer support groups, harm reduction programs, and outreach services—can provide vital social support and resources for individuals in recovery. Sustaining these programs through funding ensures they can continue to complement medical treatment and address the broader needs of those affected by OUD.
7. Public Health Campaigns
Launching public health campaigns aimed at raising awareness about OUD, reducing stigma, and promoting treatment-seeking behavior is essential. These campaigns can educate the public about low-cost treatment options and encourage individuals to seek help early, ultimately improving health outcomes.
8. Research and Evaluation
Investing in research to evaluate the effectiveness of low-cost OUD treatment strategies is crucial for continuous improvement. By identifying best practices and allocating resources efficiently, governments can improve treatment outcomes over time and adapt to their populations’ evolving needs.
By implementing these comprehensive strategies, governments can enhance access to affordable OUD treatment, reduce barriers to care, and support long-term recovery for individuals affected by opioid use disorder. Collaborative efforts among policymakers, healthcare providers, and community organizations can create a supportive environment that fosters recovery and saves lives. Addressing the opioid crisis requires innovative and sustainable solutions, and with the right strategies in place, we can make significant progress in overcoming this public health challenge.
Community Resource Strategies for Enhancing Access to Low-Cost Opioid Use Disorder Treatment
Access to affordable and effective treatment for opioid use disorder (OUD) is crucial for addressing the ongoing opioid crisis. Community resource strategies can significantly improve treatment access and outcomes for individuals seeking help. Here are several key strategies that communities can implement:
1. Peer Support Programs
Establishing peer support groups or recovery communities can create safe spaces for individuals in recovery to connect, share experiences, and provide mutual encouragement. Peer support complements formal treatment and fosters a sense of belonging and accountability, which can be instrumental in maintaining long-term recovery.
2. Harm Reduction Services
Harm reduction initiatives, such as needle exchange programs and naloxone distribution, play a critical role in minimizing the risks associated with opioid use. By providing overdose prevention education and safer practices, these services reach individuals who may not be ready or able to access formal treatment immediately, promoting health and safety within the community.
3. Community Health Centers
Strengthening community health centers to offer integrated OUD treatment services, including medication-assisted treatment (MAT), counseling, and primary care, makes treatment accessible. These centers serve as familiar and approachable points of care, allowing individuals to receive comprehensive support closer to home.
4. Mobile Outreach Services
Deploying mobile units or outreach teams can effectively reach underserved populations, particularly those in rural or remote areas. These teams can conduct on-site screenings and assessments and provide direct links to treatment resources, effectively overcoming transportation and geographic isolation barriers.
5. Telehealth and Virtual Care
Expanding telehealth services allows for the remote delivery of OUD treatment, including counseling and medication management. This accessibility reduces travel costs and facilitates continuity of care, making it easier for individuals to engage with their treatment plans from the comfort of their homes.
6. Community Education and Awareness Campaigns
Launching public education campaigns to raise awareness about OUD can reduce stigma and promote understanding of available treatment options. Hosting community workshops and informational sessions empowers individuals and families to seek early help, fostering a more informed community that is better equipped to tackle addiction.
7. Legal and Social Services Support
Collaborating with legal aid organizations and social services can address the social determinants of health that impact individuals with OUD. By providing assistance with housing stability, employment opportunities, and navigating legal issues related to addiction treatment, communities can create a more supportive environment for recovery.
8. Funding and Grants
Securing funding and grants to support community-based organizations focusing on OUD treatment and recovery can sustain low-cost or free services for those in need. This financial backing is crucial for maintaining programs that support individuals seeking recovery.
9. Cultural Competency and Linguistic Accessibility
Ensuring that services are culturally competent and linguistically accessible is vital for reaching diverse populations. This includes translating materials into different languages, providing interpretation services, and being attuned to cultural factors that influence treatment-seeking behavior, thereby fostering inclusive access to treatment.
10. Collaboration with Stakeholders
Fostering partnerships among community organizations, healthcare providers, law enforcement, schools, and local government agencies enhances resource sharing and coordination. Collaborative efforts can leverage strengths across sectors to ensure a comprehensive approach to improving access to OUD treatment and outcomes.
By implementing these community resource strategies, communities can significantly enhance access to affordable, effective treatment for opioid use disorder. Supporting individuals in their recovery journey is essential for overcoming the challenges of addiction and building healthier, more resilient communities. Together, these strategies can create a robust support network that empowers individuals to achieve long-term recovery and well-being.
Overcoming Barriers to Low-Cost Opioid Use Disorder Treatment Initiatives
The opioid crisis continues to impact communities across the globe, highlighting the urgent need for effective and accessible treatment for opioid use disorder (OUD). While low-cost treatment initiatives aim to reduce barriers to care, several challenges can hinder their successful implementation and limit access and treatment outcomes. Understanding these barriers is crucial for developing effective strategies to improve access to OUD treatment. Here are some of the key obstacles:
1. Financial Constraints
Even with subsidized medications and treatment services, out-of-pocket costs can be a significant barrier for many patients. Individuals without insurance or those with high deductibles may find treatment unaffordable, deterring them from seeking or continuing care. Addressing financial constraints is essential to ensure all individuals can access the treatment they need.
2. Limited Provider Availability
A shortage of healthcare providers trained in addiction treatment can restrict access, particularly in rural or underserved areas. This workforce shortage means fewer options for individuals seeking care, leading to longer wait times and decreased likelihood of timely treatment.
3. Regulatory Barriers
Complex and often restrictive regulations surrounding the prescribing of OUD medications, such as buprenorphine and methadone, can discourage healthcare providers from offering these treatments. Mandatory training, certification, and oversight requirements can create administrative burdens that complicate the provision of care.
4. Stigma and Perception
The stigma associated with addiction and medication-assisted treatment (MAT) can significantly influence both patient and provider attitudes toward treatment. Misconceptions about the effectiveness and safety of OUD medications may result in a reluctance to prescribe these treatments or to seek help.
5. Lack of Integrated Care Models
Fragmented healthcare systems that fail to support the integration of OUD treatment into primary care can create barriers to effective care. Individuals may experience fragmented treatment without coordinated services, resulting in suboptimal outcomes.
6. Geographic and Transportation Challenges
Limited access to treatment facilities and transportation barriers, especially in rural or remote areas, can prevent individuals from obtaining regular care. Lack of reliable transportation options may make it difficult for individuals to attend appointments or access support services.
7. Insurance Coverage Gaps
Inconsistent insurance coverage and a lack of reimbursement for certain OUD medications can impede access to treatment. High copayments, restrictions on medication quantities, or prior authorization requirements can limit patients’ options and make treatment financially unfeasible.
8. Language and Cultural Barriers
The limited availability of culturally and linguistically appropriate services can pose significant obstacles for individuals from diverse backgrounds. Challenges in accessing information, understanding treatment options, and navigating the healthcare system can prevent individuals from seeking the care they need.
9. Data Privacy and Confidentiality Concerns
Concerns about privacy and confidentiality regarding addiction treatment can deter individuals from seeking care. In communities where stigma is prevalent, fears of disclosure and the potential legal or social consequences associated with seeking treatment can be significant barriers.
Addressing these barriers to low-cost OUD treatment requires a comprehensive approach that includes policy reforms, provider education, stigma-reduction initiatives, enhanced care integration, improved transportation access, and increased public awareness of available treatment options. By working collaboratively, policymakers, healthcare providers, and communities can overcome these challenges and improve access to affordable, effective treatment for opioid use disorder. Doing so will support long-term recovery and promote healthier communities for all.
Frequently Asked Questions
Here are some common questions:
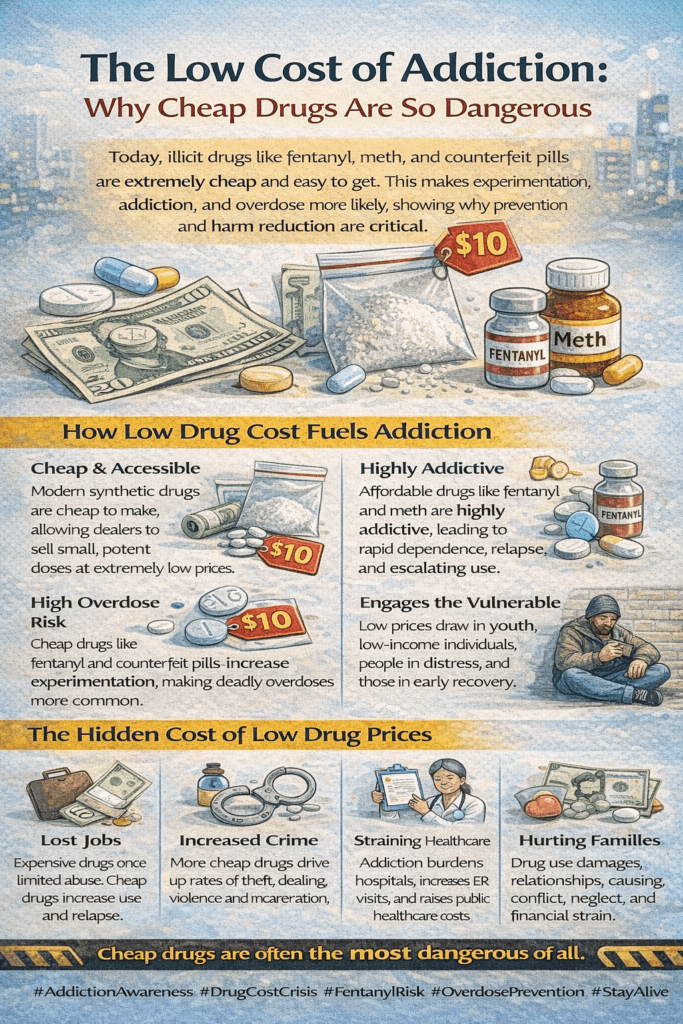
1. What does “low cost of addiction” mean?
It refers to how modern illicit drugs are cheaper and more accessible than ever, increasing the risk of frequent use and addiction.
2. Why are drugs like fentanyl so inexpensive?
Fentanyl is extremely potent, so tiny amounts produce strong effects. This makes it cheap to manufacture, transport, and sell.
3. Does a cheaper drug cost increase addiction risk?
Yes. When drugs are affordable and easy to obtain, experimentation increases, and dependence can develop more quickly.
4. Are low-cost drugs more dangerous?
Often yes. Cheap synthetic drugs like fentanyl and methamphetamine are highly potent and unpredictable, raising overdose risk.
5. How do counterfeit pills relate to low drug costs?
Fake pills are cheaply manufactured and sold as real prescriptions, often containing fentanyl, leading to accidental overdoses.
6. Does low cost affect relapse risk?
Yes. Easy and affordable access to drugs increases temptation and relapse risk for individuals in recovery.
7. Are there hidden costs of cheap drugs?
Absolutely. Addiction leads to healthcare expenses, job loss, legal issues, and family strain — far exceeding the price of the drug itself.
8. Why has the cost of drugs dropped in recent years?
Synthetic drug production requires fewer raw materials and can be manufactured quickly, lowering market prices.
9. Can education reduce the impact of low-cost drugs?
Yes. Awareness helps people understand that cheap drugs are not safer and carry a high addiction and overdose risk.
10. What helps protect communities from low-cost addiction dangers?
Prevention education, accessible treatment, harm-reduction tools, naloxone availability, and community support.
Conclusion
Enhancing access to low-cost opioid use disorder (OUD) treatment is paramount in addressing the complex challenges posed by opioid addiction. Government intervention is critical through policy reforms and funding initiatives to expand access to affordable treatment options. Despite these efforts, barriers such as financial constraints, regulatory hurdles, stigma, and disparities in healthcare access persist, limiting the effectiveness of interventions. However, community resource strategies offer promising avenues to overcome these barriers, including peer support programs, harm reduction services, and community health centers. By fostering collaboration between government agencies, healthcare providers, and community organizations, we can create a more comprehensive and accessible care system for individuals affected by OUD. These efforts are essential not only in improving treatment outcomes but also in supporting long-term recovery and reducing the devastating impact of opioid addiction on individuals and communities alike.
Video: How Affordability Made Addiction Worse #AddictionTruth #PublicHealth