Licensure policies are critical for ensuring access to opioid use disorder (OUD) medication in specialty addiction treatment, impacting provider practices and patient outcomes. Governed at the state level, these policies aim to broaden the pool of healthcare providers able to prescribe medications like buprenorphine and methadone. Effective implementation relies on government support and community engagement. Yet, barriers such as provider restrictions, regulatory complexities, stigma, and healthcare disparities hinder their execution. Addressing these challenges requires simplifying regulations, enhancing provider education, reducing stigma, and promoting integrated healthcare models. By doing so, states can improve access to essential OUD medications and enhance addiction treatment services for all.
The Impact of Licensure Policies on Access to Opioid Use Disorder Medications
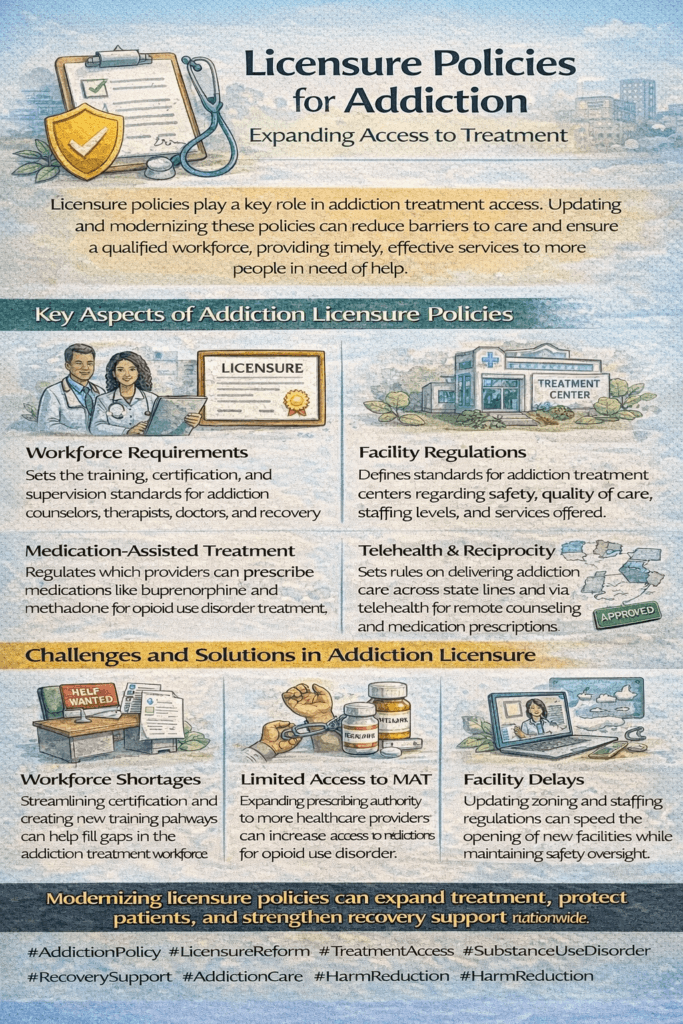
Licensure policies are critical components of the healthcare landscape, especially in the context of treating opioid use disorder (OUD). These regulations define who can provide treatment and influence how and where care is delivered. By understanding how licensure policies can facilitate access to OUD medications, we can identify opportunities to improve treatment for individuals affected by opioid addiction. Here are several key ways in which these policies play a pivotal role:
1. Provider Eligibility
Licensure policies determine which healthcare providers can prescribe and administer OUD medications, such as buprenorphine and methadone. Expanding eligibility to include a broader range of providers, such as nurse practitioners and physician assistants, can significantly increase the number of clinicians available to provide OUD treatment. This is particularly beneficial in underserved areas where addiction treatment services are scarce.
2. Telemedicine and Remote Prescribing
Many licensure policies now recognize the value of telemedicine and allow for remote prescribing of OUD medications. This is especially advantageous in rural or remote regions with limited access to specialty addiction treatment services. By enabling providers to assess and prescribe medications remotely, these policies expand access to OUD treatment beyond traditional clinic settings.
3. Integration of Services
Licensure policies that support the integration of OUD treatment into primary care settings and community health centers enhance access by minimizing barriers to care. Individuals can receive therapy in familiar healthcare environments, making it more convenient and less stigmatizing to seek help. This holistic approach encourages comprehensive care for patients, addressing both their addiction and overall health needs.
4. Continuing Education Requirements
Many licensure policies include ongoing education requirements on addiction treatment and OUD management. These requirements ensure that healthcare providers remain informed about the latest evidence-based practices and treatment guidelines. By promoting continuous learning, these policies help improve the quality of care delivered to patients and ultimately enhance treatment outcomes.
5. Reducing Stigma and Barriers
Licensure policies that advocate for comprehensive, patient-centered care can help mitigate the stigma often associated with addiction treatment. These policies promote compassionate and effective care delivery by establishing clear guidelines and expectations for providers. A supportive environment fosters trust, encouraging individuals to seek treatment without fear of judgment.
6. Monitoring and Oversight
Effective licensure policies typically include provisions for monitoring and oversight of OUD treatment practices. This ensures adherence to clinical guidelines and regulatory standards, maintaining the safety and efficacy of treatment services. Furthermore, robust oversight safeguards against potential misuse or diversion of medications, enhancing the integrity of the treatment process.
Overall, licensure policies play a vital role in shaping the landscape of OUD treatment. By expanding provider eligibility, supporting telemedicine initiatives, promoting integrated services, and ensuring ongoing education, these policies enhance access to effective OUD medications. Additionally, they contribute to reducing stigma and ensuring quality oversight, which are essential for improving outcomes for individuals affected by opioid addiction. Policymakers must continue to evaluate and adapt licensure regulations to foster an environment that supports accessible, effective treatment for all needy individuals.
Enhancing Access to Opioid Use Disorder Medications Through Effective Licensure Policies
Governments play a critical role in addressing the opioid crisis, particularly in ensuring access to effective treatment for opioid use disorder (OUD). One essential avenue for improving access is through effective licensure policies that facilitate the availability of OUD medications in specialty addiction treatment. Here are several strategies governments can implement to achieve this goal:
1. Expand Provider Eligibility
One of the most impactful steps is to revise licensure policies to include a broader range of healthcare providers eligible to prescribe OUD medications. This could involve allowing nurse practitioners, physician assistants, and potentially pharmacists to take on this role. By increasing the pool of accessible providers, especially in urban and rural areas where addiction specialists may be scarce, we can ensure that more individuals can access the care they need.
2. Telemedicine and Remote Prescribing
Governments can establish regulations allowing telemedicine and remote prescribing of OUD medications. This flexibility is precious in reaching patients in remote or underserved areas where traditional treatment facilities are unavailable. By enabling healthcare providers to conduct assessments and prescribe medications remotely, barriers to treatment access can be significantly reduced.
3. Integration of Services
Another effective strategy is encouraging the integration of OUD treatment into primary care settings and community health centers. Governments can incentivize or mandate collaboration between addiction specialists and primary care providers to create seamless patient care transitions. This approach not only enhances accessibility but also reduces the stigma often associated with seeking addiction treatment, as individuals can receive care in familiar healthcare environments.
4. Education and Training Requirements
To ensure that healthcare providers are well-equipped to offer effective OUD treatment, implementing continuing education requirements focused on addiction treatment and OUD management is essential. We can promote high-quality care and improve patient treatment outcomes by requiring providers seeking licensure or renewal to stay up to date on the latest evidence-based practices.
5. Quality Standards and Oversight
Establishing clear licensure standards and regulatory oversight is crucial for maintaining high-quality care delivery in OUD treatment. Governments should regularly monitor and evaluate treatment programs to ensure adherence to evidence-based practices. This oversight helps safeguard patient safety and ensure effective treatment.
6. Public Awareness and Support
Governments can support public awareness campaigns to educate communities about the importance of OUD treatment. These campaigns can play a significant role in destigmatizing addiction and encouraging individuals to seek help. Governments can foster a supportive environment for recovery by raising awareness of available treatment options.
7. Collaboration with Stakeholders
Finally, fostering collaboration between government agencies, healthcare providers, addiction treatment organizations, and community stakeholders is vital for developing comprehensive strategies to improve access to OUD treatment. This collaborative approach ensures that policies are effective and responsive to the unique needs of diverse communities.
By implementing these strategies, governments can leverage licensure policies to enhance access to OUD medications and improve outcomes for individuals affected by opioid addiction. A comprehensive approach that expands provider eligibility, supports telemedicine, integrates services, and promotes education can create a more accessible and effective treatment landscape. Together, these efforts can contribute to mitigating the impact of the opioid crisis and supporting the recovery journey for countless individuals in need.
Strengthening Access to Opioid Use Disorder Medications Through Community Resource Strategies
Community resource strategies are essential in supporting the implementation of licensure policies designed to ensure access to opioid use disorder (OUD) medications in specialty addiction treatment. By leveraging community resources effectively, stakeholders can enhance the treatment landscape and improve outcomes for individuals affected by opioid addiction. Here are several impactful strategies:
1. Support Groups and Peer Networks
Community-based support groups and peer networks provide invaluable emotional support and encouragement for individuals recovering from OUD. These groups can complement formal treatment by fostering a sense of belonging, sharing resources, and promoting adherence to treatment plans. Peer support enhances motivation and creates a safe space for individuals to share their experiences and challenges.
2. Education and Awareness Programs
Educational initiatives conducted by community organizations play a crucial role in raising awareness about OUD, available treatment options, and the importance of licensed healthcare providers. These programs help to demystify addiction, reduce stigma, and empower individuals with knowledge about the resources available to them, ultimately encouraging more people to seek help.
3. Access to Transportation
For individuals living in rural or underserved areas, a lack of transportation can be a significant barrier to accessing treatment. Community resources can include transportation services or partnerships with local transit authorities to facilitate travel to treatment facilities. Ensuring reliable transportation options is vital for enabling consistent access to care.
4. Crisis Intervention and Counseling Services
Community-based crisis intervention teams and counseling services provide immediate support for individuals experiencing substance use crises. These services can help stabilize individuals in need and connect them with appropriate treatment resources, including licensed providers. By addressing crises promptly, communities can prevent further deterioration of individuals’ health and facilitate smoother transitions into treatment.
5. Community Health Centers and Clinics
Enhancing the capacity of community health centers and clinics to provide integrated care for OUD, including medication-assisted treatment (MAT), is crucial. These centers serve as accessible points of care, offering comprehensive services closer to home. By integrating addiction treatment into primary care settings, individuals can receive holistic care that addresses both their physical and mental health needs.
6. Collaboration with Law Enforcement and Justice Systems
Establishing collaborations between healthcare providers, law enforcement, and justice systems can facilitate diverting individuals with OUD into treatment rather than incarceration. This approach promotes holistic care and reduces recidivism rates, ensuring that individuals receive the support they need while addressing the underlying issues related to their substance use.
7. Harm Reduction Services
Community organizations can provide harm reduction services, including needle exchange programs, naloxone distribution, and overdose prevention education. These services help to mitigate the negative consequences of opioid misuse while individuals engage in treatment, promoting safer practices and reducing the overall harm associated with drug use.
8. Employment and Housing Assistance
Stable employment and housing are vital components of recovery for individuals with OUD. Community resources can include job training programs, supportive housing options, and partnerships with employers willing to hire individuals in recovery. By addressing these social determinants of health, communities can create supportive environments that facilitate long-term recovery.
By implementing these community resource strategies, stakeholders can effectively strengthen the implementation of licensure policies to expand access to OUD medications and improve treatment outcomes. Collaborative efforts can build resilient communities that support recovery and enhance overall well-being. Through comprehensive and coordinated approaches, we can ensure that individuals affected by opioid addiction receive the care, support, and resources they need to embark on their recovery journeys.
Overcoming Barriers to Accessing Opioid Use Disorder Medications: A Call to Action
The practical implementation of licensure policies aimed at ensuring access to opioid use disorder (OUD) medications in specialty addiction treatment settings faces several significant barriers. Understanding these challenges is crucial for policymakers and healthcare stakeholders looking to improve access to care and enhance treatment outcomes for individuals affected by opioid addiction. Here are some of the primary barriers that hinder access to OUD medications:
1. Provider Eligibility Restrictions
Licensure policies often limit the types of healthcare providers eligible to prescribe OUD medications like buprenorphine and methadone. The exclusion of nurse practitioners, physician assistants, and pharmacists from prescribing these medications reduces the number of accessible providers, particularly in rural or underserved areas where specialty addiction treatment is scarce.
2. Training and Education Requirements
Stringent and complex training and education requirements for providers seeking authorization to prescribe OUD medications can pose significant barriers. These requirements can be time-consuming, costly, or difficult to access, especially for healthcare providers in smaller practices or community health settings. Simplifying these processes is essential to encourage more providers to become certified.
3. Stigma and Misconceptions
The stigma surrounding OUD and medication-assisted treatment (MAT) can affect both providers’ willingness to prescribe and patients’ readiness to seek treatment. Misconceptions about the effectiveness and safety of OUD medications often lead healthcare providers to be reluctant to incorporate these treatments into their practice, ultimately limiting patient access to necessary care.
4. Regulatory Burden and Administrative Processes
Cumbersome administrative processes, including prior authorization requirements and complex reporting obligations, can deter providers from offering OUD medications. These regulatory burdens complicate the prescribing process and can delay patients’ access to vital treatments, worsening health outcomes.
5. Reimbursement and Financial Barriers
Inadequate reimbursement rates and limited insurance coverage for OUD medications and associated services can discourage providers from offering these treatments. Patients often face high out-of-pocket costs, which can deter them from seeking necessary medications. Improving reimbursement policies is essential to making treatment more affordable.
6. Geographic and Accessibility Challenges
The limited availability of specialty addiction treatment facilities and OUD medication providers in rural or remote areas restricts access for individuals living in these regions. Transportation barriers complicate access to care, especially for individuals who lack reliable transportation. Addressing these challenges requires innovative solutions such as mobile clinics and telehealth services.
7. Workforce Shortages
There is a notable shortage of healthcare providers trained in addiction treatment and OUD management. This workforce shortage is particularly acute in areas with high service demand, resulting in inadequate access to specialized care. Strategies to recruit and train more addiction specialists are vital for addressing this issue.
8. Lack of Integrated Care Models
Fragmented healthcare systems that fail to support the integration of OUD treatment into primary care settings or community health centers create significant barriers. Lack of coordination among healthcare providers and services can lead to disjointed care, ultimately reducing treatment effectiveness.
Addressing barriers to OUD medication access requires comprehensive strategies that include policy reforms, enhanced provider education, stigma-reduction efforts, improved reimbursement policies, and increased geographic access to care. By overcoming these challenges, states can strengthen access to OUD medications, ultimately improving outcomes for individuals affected by opioid addiction. Collaborative efforts among policymakers, healthcare providers, and community organizations are essential for fostering a supportive environment that prioritizes effective treatment and recovery for those in need.
Frequently Asked Questions
Here are some common questions:
1. What are licensure policies in addiction treatment?
They are laws and regulations that determine who is qualified and legally allowed to provide substance use disorder treatment services.
2. Why do licensure policies matter in addiction care?
They protect patient safety, ensure provider competency, and set quality standards for treatment programs.
3. Can licensure rules limit access to treatment?
Yes. Overly strict or outdated licensing requirements can delay provider certification and reduce the number of available treatment professionals.
4. How do licensure policies affect rural communities?
Rural areas often face provider shortages because fewer professionals meet licensing requirements or are available to practice locally.
5. What is reciprocity in licensing?
Reciprocity allows licensed addiction professionals to practice across state lines without having to repeat the entire credentialing process, thereby improving workforce mobility.
6. Do licensure policies affect medication-assisted treatment (MAT)?
Yes. Some states restrict which providers can prescribe medications like buprenorphine or methadone, limiting treatment availability.
7. How does telehealth relate to licensure policies?
Telehealth expansion allows licensed providers to deliver addiction care remotely, but cross-state licensing rules can still create barriers.
8. Why are facility licensing rules important?
They ensure treatment centers meet safety, staffing, and ethical standards, protecting clients from poor-quality or fraudulent programs.
9. What happens when licensure policies are too relaxed?
Without proper oversight, unsafe or unethical treatment practices can occur. A balance between access and quality is essential.
10. How can licensure policies be improved?
Through faster credentialing, cross-state reciprocity, expanded training pathways, and updated telehealth regulations to increase access while maintaining safety.
Conclusion
Licensure policies are pivotal tools for enhancing access to opioid use disorder (OUD) medication within specialty addiction treatment. With government support and active community involvement, these policies aim to expand the cadre of healthcare providers authorized to prescribe critical medicines like buprenorphine and methadone. However, barriers such as restrictive provider eligibility criteria, regulatory complexities, stigma surrounding addiction, and disparities in healthcare access pose significant challenges. Overcoming these hurdles demands collaborative efforts to streamline regulations, increase provider education, combat stigma, and foster integrated healthcare systems. By addressing these issues comprehensively, states can effectively improve access to essential OUD medications and elevate the quality of addiction treatment services across diverse populations.
Video: The Hidden Rule Blocking People from Getting Help #AddictionCare #LicensureReform