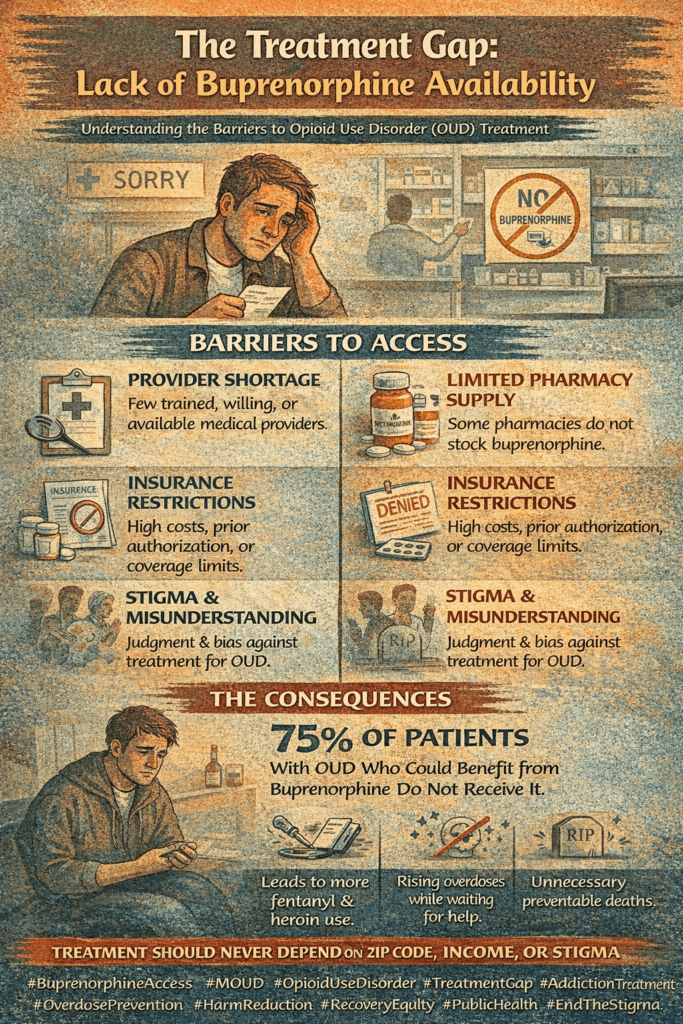
The lack of availability of buprenorphine, an essential medication for opioid use disorder (OUD), hinders effective treatment and recovery. Buprenorphine reduces cravings and withdrawal symptoms, improving health outcomes and supporting long-term recovery. Governments have addressed this issue through policy changes and financial incentives. Community strategies like expanding telemedicine, integrating treatment into primary care, and public education are crucial for increasing accessibility. These efforts aim to enhance the availability of buprenorphine, helping more individuals receive the treatment they need to combat the opioid crisis.
The Critical Importance of Buprenorphine in Drug Addiction Recovery
The availability of buprenorphine for treating opioid addiction is a crucial element in addressing the opioid crisis. Buprenorphine is a medication that provides significant benefits for individuals struggling with opioid use disorder (OUD), helping to stabilize their lives, support recovery, and improve overall health. Here’s why its availability is so important:
1. Effectiveness in Treating Opioid Use Disorder (OUD)
- Reduction in Opioid Use: Buprenorphine, as a partial opioid agonist, helps to reduce cravings and alleviate withdrawal symptoms, making it easier for individuals to stop using opioids. Research has shown that it significantly decreases illicit opioid use and increases retention in treatment programs, offering a more sustainable path to recovery.
- Improvement in Health Outcomes: Individuals treated with buprenorphine experience better health outcomes, including lower risks of infectious diseases like HIV and Hepatitis C. There is also a reduction in overdose incidents and improvements in mental health due to stabilized brain chemistry and reduced substance use.
2. Safety Profile
- Lower Risk of Overdose: Buprenorphine is safer than full opioid agonists, such as methadone, because it has a “ceiling effect” that limits respiratory depression. This makes it a safer treatment choice for many patients, reducing the risk of fatal overdose.
- Office-Based Treatment: Unlike methadone, which often requires daily visits to a specialized clinic, buprenorphine can be prescribed and administered in an office-based setting. This approach increases the convenience and accessibility of treatment, encouraging adherence and continuity of care.
3. Supporting Long-term Recovery
- Stabilization: Buprenorphine helps stabilize patients by normalizing brain chemistry and reducing the highs and lows associated with opioid addiction. This stabilization allows individuals to focus on rebuilding their lives and engaging in meaningful activities that support long-term recovery.
- Integration with Psychosocial Support: Buprenorphine is commonly used in conjunction with counseling and behavioral therapies, forming a comprehensive approach known as medication-assisted treatment (MAT). This integrated method addresses the physical, psychological, and social aspects of addiction, enhancing the chances of sustained recovery.
4. Reducing Societal Impact
- Lowering Healthcare Costs: Effective treatment with buprenorphine can significantly reduce healthcare costs by reducing the need for emergency care, hospitalizations, and treatment for co-occurring conditions. It also helps lessen the economic burden associated with untreated addiction, including lost productivity and criminal justice expenses.
- Reducing Crime and Improving Public Safety: Individuals undergoing buprenorphine treatment are less likely to engage in criminal activities related to drug use. By reducing drug-related crime, buprenorphine contributes to safer communities and relieves some pressure on the criminal justice system.
5. Addressing Public Health Crises
- Response to the Opioid Epidemic: The opioid epidemic has caused a dramatic rise in opioid-related overdoses and deaths. Expanding access to buprenorphine is a critical component of the public health response to this crisis, as it provides a proven treatment that saves lives and supports recovery efforts.
- Harm Reduction: As an essential tool in harm reduction strategies, buprenorphine minimizes the adverse health and social consequences of drug use. It helps individuals reduce their reliance on illicit opioids, even if they do not immediately pursue complete abstinence, allowing for a more gradual and supportive path to recovery.
6. Equity and Accessibility
- Addressing Disparities: Expanding the availability of buprenorphine helps address disparities in access to addiction treatment. This is especially important for underserved populations, including those in rural areas, low-income communities, and minority groups disproportionately affected by the opioid crisis. Improving accessibility ensures that everyone can receive effective treatment regardless of background or location.
The availability of buprenorphine is essential for supporting drug addiction recovery due to its safety, effectiveness, and accessibility. It promotes long-term promotion, improves health outcomes, reduces societal costs, and plays a critical role in addressing the opioid epidemic. Expanding access to buprenorphine is a necessary step to enhance the healthcare system’s capacity to treat opioid use disorder and mitigate the broader impacts of the opioid crisis. Buprenorphine is not just a treatment option; it is a lifeline that can save lives and transform communities.
Critical Reasons Behind the Lack of Buprenorphine Availability
The government has taken various steps to increase the availability of buprenorphine and improve access to treatment for opioid use disorder (OUD). These measures address regulatory, economic, and access barriers while tackling stigma and expanding healthcare provider capabilities. Some key initiatives include:
1. Regulatory and Policy Changes
- Relaxing Prescribing Restrictions: The U.S. government has worked to ease prescribing restrictions on buprenorphine. In 2021, the Department of Health and Human Services (HHS) introduced new guidelines that eliminated the requirement for certain prescribers to complete a unique training and certification (known as the “X-waiver”) to prescribe buprenorphine for up to 30 patients. This change allows more healthcare providers, including primary care providers, to treat OUD with buprenorphine.
- Increasing Patient Limits: The government has increased the number of patients certified providers can treat. Initially, providers were limited to treating 30 patients in their first year of certification, but this can now be expanded to 100 patients in the first year and up to 275 thereafter.
- Telemedicine Flexibility: During the COVID-19 pandemic, federal agencies such as the Drug Enforcement Administration (DEA) allowed expanded telemedicine prescribing of buprenorphine without an in-person visit. This measure increased access to treatment, particularly for individuals in remote or underserved areas.
2. Expanding Access in Rural and Underserved Areas
- Grant Programs and Funding Initiatives: The government has allocated funding to support addiction treatment programs, including those that provide buprenorphine. The Substance Abuse and Mental Health Services Administration (SAMHSA) offers grants to increase access to medication-assisted treatment (MAT) in rural and underserved areas.
- Mobile Treatment Units and Community Health Centers: The government has promoted the establishment of mobile treatment units and the integration of MAT services into community health centers, increasing access to buprenorphine in areas with limited healthcare resources.
3. Reducing Cost Barriers
- Medicaid Expansion and Coverage Requirements: The Affordable Care Act (ACA) expanded Medicaid coverage to include substance use disorder (SUD) treatment, including buprenorphine. Some states have also passed legislation requiring insurance companies to cover MAT without prior authorization, making it easier for patients to access treatment.
- Increased Reimbursement for MAT Services: Efforts have been made to increase reimbursement rates for MAT services under Medicaid and Medicare, encouraging more providers to offer buprenorphine treatment.
4. Addressing Stigma and Misinformation
- Public Awareness Campaigns: The government has supported public health campaigns to reduce the stigma associated with OUD and MAT, aiming to educate the public on the effectiveness and safety of buprenorphine for addiction treatment.
- Provider Education and Training Programs: Federal agencies, such as SAMHSA, have launched initiatives to enhance education and training for healthcare providers on buprenorphine and other MAT options. These programs aim to increase the number of providers equipped to treat OUD.
5. Criminal Justice System Initiatives
- MAT in Correctional Facilities: The government is working to expand access to buprenorphine in jails and prisons, where OUD is prevalent. Some states have implemented pilot programs to provide MAT to incarcerated individuals, and federal funding is available to support these initiatives.
- Reentry Programs: Policies are being developed to ensure continuity of care for individuals transitioning out of the criminal justice system, helping them access buprenorphine treatment upon release to reduce the risk of overdose and relapse.
6. Legal and Policy Advocacy
- Support for the Mainstreaming Addiction Treatment (MAT) Act: This legislative proposal eliminates the special training and waiver requirements for buprenorphine prescribing altogether, making it as accessible as other medications. The act also addresses legal barriers and promotes the availability of buprenorphine across various healthcare settings.
These government efforts represent significant steps toward expanding access to buprenorphine for OUD treatment. However, ongoing challenges remain, including geographic disparities in access, persistent stigma, and the need for ongoing regulatory reforms. Addressing these issues will be crucial for further improving the reach and effectiveness of buprenorphine as part of the response to the opioid crisis.
Government Initiatives to Increase Buprenorphine Availability for Opioid Use Disorder Treatment
The U.S. government has implemented various measures to expand the availability of buprenorphine for treating opioid use disorder (OUD). These initiatives aim to remove barriers, increase provider capacity, and reduce the stigma associated with the treatment, helping to address the ongoing opioid crisis. Here are some key actions taken by the government to improve access to buprenorphine:
Legislative and Regulatory Changes
- Support Act (2018): The Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act was a landmark step toward expanding access to medication-assisted treatment (MAT). It allowed a broader range of healthcare professionals, such as nurse practitioners and physician assistants, to prescribe buprenorphine, thereby increasing the number of qualified prescribers. The Act also raised patient limits, enabling these providers to treat more individuals.
- Mainstreaming Addiction Treatment (MAT) Act (2021): The MAT Act eliminated the requirement for healthcare providers to obtain a separate waiver (the X-waiver) to prescribe buprenorphine for OUD. By reducing this regulatory burden, the Act aimed to make it easier for more clinicians to provide buprenorphine treatment.
Financial Incentives and Grants
- State Targeted Response (STR) and State Opioid Response (SOR) Grants: Administered by the Substance Abuse and Mental Health Services Administration (SAMHSA), these grants support state-level efforts to expand access to MAT, including buprenorphine. They provide funding for treatment programs, infrastructure, and training to increase availability in areas with high OUD rates.
- Medicaid Expansion: Expanding Medicaid under the Affordable Care Act (ACA) allowed more low-income individuals to access OUD treatment, including buprenorphine. Medicaid programs in many states cover the cost of medication, counseling, and other related services, significantly increasing access for vulnerable populations.
Increasing Provider Capacity
- Training and Education Programs: The federal government has funded initiatives to train healthcare providers in treating OUD, including the proper use of buprenorphine. SAMHSA, along with other federal agencies, provides training modules, continuing education credits, and technical assistance to clinicians to encourage the incorporation of MAT into their practices.
- Project ECHO (Extension for Community Healthcare Outcomes): This telemedicine-based model connects primary care providers with addiction specialists, enhancing their ability to manage OUD treatment. Project ECHO has been instrumental in expanding access to buprenorphine treatment in rural and underserved areas by training and supporting local healthcare providers.
Enhancing Access in Underserved Areas
- Telemedicine Expansion: During the COVID-19 pandemic, regulations were relaxed to allow providers to prescribe buprenorphine through telemedicine without requiring an in-person visit. This change increased access to treatment for individuals in rural and underserved areas, where addiction specialists may not be readily available.
- Federally Qualified Health Centers (FQHCs): FQHCs receive federal funding for primary and preventive care, including MAT services. Expanding MAT programs within these centers has improved access to buprenorphine in low-income and underserved communities, helping to bridge the treatment gap.
Criminal Justice System Reforms
- Support for MAT in Correctional Facilities: There has been a push to make MAT, including buprenorphine, available in jails and prisons. By providing treatment during incarceration and linking individuals to MAT services upon release, these programs aim to reduce relapse and overdose risk for formerly incarcerated individuals.
Public Awareness and Anti-Stigma Campaigns
- Public Health Campaigns: Agencies such as SAMHSA and the Centers for Disease Control and Prevention (CDC) have launched campaigns to reduce stigma surrounding OUD and MAT. These efforts focus on educating the public, healthcare professionals, and policymakers about the effectiveness of buprenorphine, aiming to increase acceptance and use of the medication.
Funding and Support for Research
- National Institutes of Health (NIH) HEAL Initiative: The Helping to End Addiction Long-term (HEAL) Initiative funds research to improve prevention and treatment of opioid addiction. The initiative supports the development and dissemination of effective MAT practices, including expanding access to buprenorphine.
Through legislative changes, financial support, training programs, telemedicine expansion, and public awareness efforts, the government has significantly increased the availability of buprenorphine for the treatment of OUD. These initiatives are helping to improve access, reduce overdose deaths, and address the public health crisis posed by the opioid epidemic. However, challenges such as geographic disparities and persistent stigma remain, requiring ongoing efforts to expand access further and ensure comprehensive support for individuals seeking recovery.
Community Strategies to Increase Buprenorphine Availability for Opioid Use Disorder Treatment
Expanding access to buprenorphine in communities requires coordinated efforts involving healthcare providers, local governments, and community organizations. Implementing the following strategies can effectively improve the availability of this critical medication-assisted treatment for opioid use disorder (OUD):
1. Training and Support for Healthcare Providers
- Expand Training Programs: Enhance training opportunities for healthcare providers, including physicians, nurse practitioners, and physician assistants, to obtain waivers for prescribing buprenorphine. Programs like those provided by the Substance Abuse and Mental Health Services Administration (SAMHSA) can be scaled up to reach more clinicians.
- Continuing Education: Offer ongoing education on best practices for treating OUD with buprenorphine. This can be achieved through webinars, workshops, and peer support networks that keep providers up to date on the latest evidence-based treatments and policy changes.
2. Integrated Care Models
- Primary Care Integration: Incorporate buprenorphine treatment into primary care settings to normalize OUD treatment and make it more accessible to patients seeking regular medical care. This approach helps reduce stigma and facilitates early intervention.
- Collaborative Care Teams: Establish multidisciplinary teams that include addiction specialists, mental health professionals, and social workers to support patients on buprenorphine. These teams can address co-occurring disorders and provide holistic care.
3. Telemedicine Expansion
- Telehealth Services: Expand the use of telemedicine to prescribe buprenorphine, particularly in rural and underserved areas where access to in-person care is limited. Telehealth can overcome geographic barriers and improve continuity of care for individuals who may face challenges attending regular appointments.
4. Community Health Centers and Clinics
- Increase Capacity at FQHCs: Federally Qualified Health Centers (FQHCs) and community clinics can expand capacity to provide buprenorphine by hiring additional trained staff and integrating medication-assisted treatment (MAT) into their services.
- Mobile Clinics: Mobile health clinics can reach remote or underserved areas, offering buprenorphine and other medical services. Mobile units can deliver care directly to communities with limited healthcare infrastructure.
5. Public Awareness and Education Campaigns
- Reduce Stigma: Launch public education campaigns to dispel myths about OUD and buprenorphine treatment. Sharing success stories and highlighting the effectiveness of MAT can help reduce stigma and encourage more individuals to seek treatment.
- Community Outreach: Partner with community leaders, local organizations, and faith-based groups to promote understanding of buprenorphine treatment and support individuals in recovery.
6. Supportive Services and Peer Support
- Peer Recovery Coaches: Employ peer recovery coaches with personal experience with OUD to support individuals in treatment. They can offer encouragement, share resources, and help navigate the healthcare system.
- Support Groups: Facilitate access to support groups tailored for individuals using buprenorphine, providing a safe space to share experiences, address challenges, and build a sense of community.
7. Collaboration with Law Enforcement and the Criminal Justice System
- MAT in Correctional Facilities: Implement programs to provide buprenorphine in jails and prisons, ensuring continuity of care during incarceration and upon release. This approach can reduce relapse and overdose risk for formerly incarcerated individuals.
- Diversion Programs: Work with law enforcement to develop programs that divert individuals with OUD to treatment instead of incarceration, offering buprenorphine as part of a comprehensive recovery plan.
8. Policy Advocacy and Funding
- Advocate for Policy Changes: Push for regulatory reforms at the local and state levels to eliminate barriers, such as waivers and patient caps, that limit buprenorphine prescribing. Policies that support MAT expansion in primary care settings can make a significant difference.
- Secure Funding: Apply for federal and state grants to support buprenorphine programs. Use these funds to train healthcare providers, build telemedicine infrastructure, and cover patient care costs.
9. Pharmacy Engagement
- Pharmacy Partnerships: Partner with local pharmacies to ensure they stock buprenorphine and educate pharmacists on the medication’s role in OUD treatment. Pharmacists can be critical in supporting patients by providing information and guidance.
- Pharmacy-Based MAT: Explore collaborative practice agreements that allow pharmacists to initiate and manage buprenorphine treatment, thereby increasing access in areas with scarce healthcare providers.
10. Data Collection and Evaluation
- Track Outcomes: Establish systems to monitor outcomes of buprenorphine treatment programs, including patient retention, health improvements, and reductions in opioid use. Use this data to improve programs and continuously advocate for more resources.
- Community Needs Assessment: Conduct regular assessments to identify gaps in treatment availability and target resources to areas with the greatest need.
Implementing these community resource strategies can significantly increase the availability of buprenorphine, making effective treatment more accessible for individuals struggling with OUD. A collaborative approach that integrates healthcare providers, local governments, and community organizations is essential to ensuring that more people can benefit from this life-saving medication.
Frequently Asked Questions
Here are some common questions:
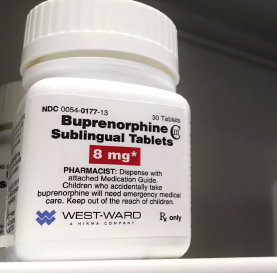
What is buprenorphine used for?
Buprenorphine is a medication used to treat Opioid Use Disorder by reducing cravings and withdrawal while lowering overdose risk.
Why is buprenorphine hard to access in some areas?
Many regions lack trained prescribers, participating pharmacies, or supportive healthcare systems, especially in rural or underserved communities.
Do all doctors prescribe buprenorphine?
No. Some providers lack training in addiction medicine, fear stigma, or are unfamiliar with updated prescribing regulations.
Can pharmacies refuse to stock buprenorphine?
Yes. Some pharmacies do not carry it due to corporate policies, misconceptions about misuse, or low local demand.
Do insurance companies create barriers to access?
Yes. Prior authorizations, coverage limitations, or high copays can delay or prevent treatment.
Does stigma affect buprenorphine availability?
Yes. Misunderstanding medication-assisted treatment discourages providers from prescribing and patients from seeking it.
What happens when treatment is delayed?
Individuals may return to illicit opioid use while waiting, increasing withdrawal suffering and overdose risk.
Is buprenorphine safer than illicit opioids?
Yes. It is a regulated, medically supervised treatment proven to reduce deaths and stabilize recovery.
Are efforts being made to improve access?
Yes. Expanding provider education, changing pharmacy policies, and reducing insurance barriers are ongoing initiatives.
How can someone find buprenorphine treatment?
Contacting local health departments, addiction clinics, or national treatment locators is the best first step.
Conclusion
Addressing the lack of availability of buprenorphine is essential for effectively combating the opioid crisis. Buprenorphine’s ability to reduce cravings and withdrawal symptoms makes it a critical component of opioid use disorder treatment, supporting better health outcomes and long-term recovery. Government interventions, such as policy reforms and financial incentives, alongside community resource strategies, such as expanding telemedicine, integrating buprenorphine into primary care, and enhancing public education, are vital to improving accessibility. These combined efforts are crucial for ensuring that more individuals can access the treatment they need, ultimately leading to a more comprehensive and effective response to the opioid epidemic.
Video: Why the Opioid Crisis Gets Worse Every Year #TreatmentGap #Buprenorphine #MOUD