Intermittent fasting (IF) is being explored as a strategy to manage addiction. It could aid physical health, reduce cravings, and improve mental clarity. While IF offers benefits, it also comes with challenges, such as health risks, ethical concerns, and psychological effects. Self-management strategies, family support, and community resources are essential to ensure its effectiveness in addiction recovery. With proper discipline, encouragement, and professional guidance, IF can be a valuable tool when integrated safely into treatment plans.
Can Intermittent Fasting Aid in Addiction Recovery? Exploring the Potential Benefits
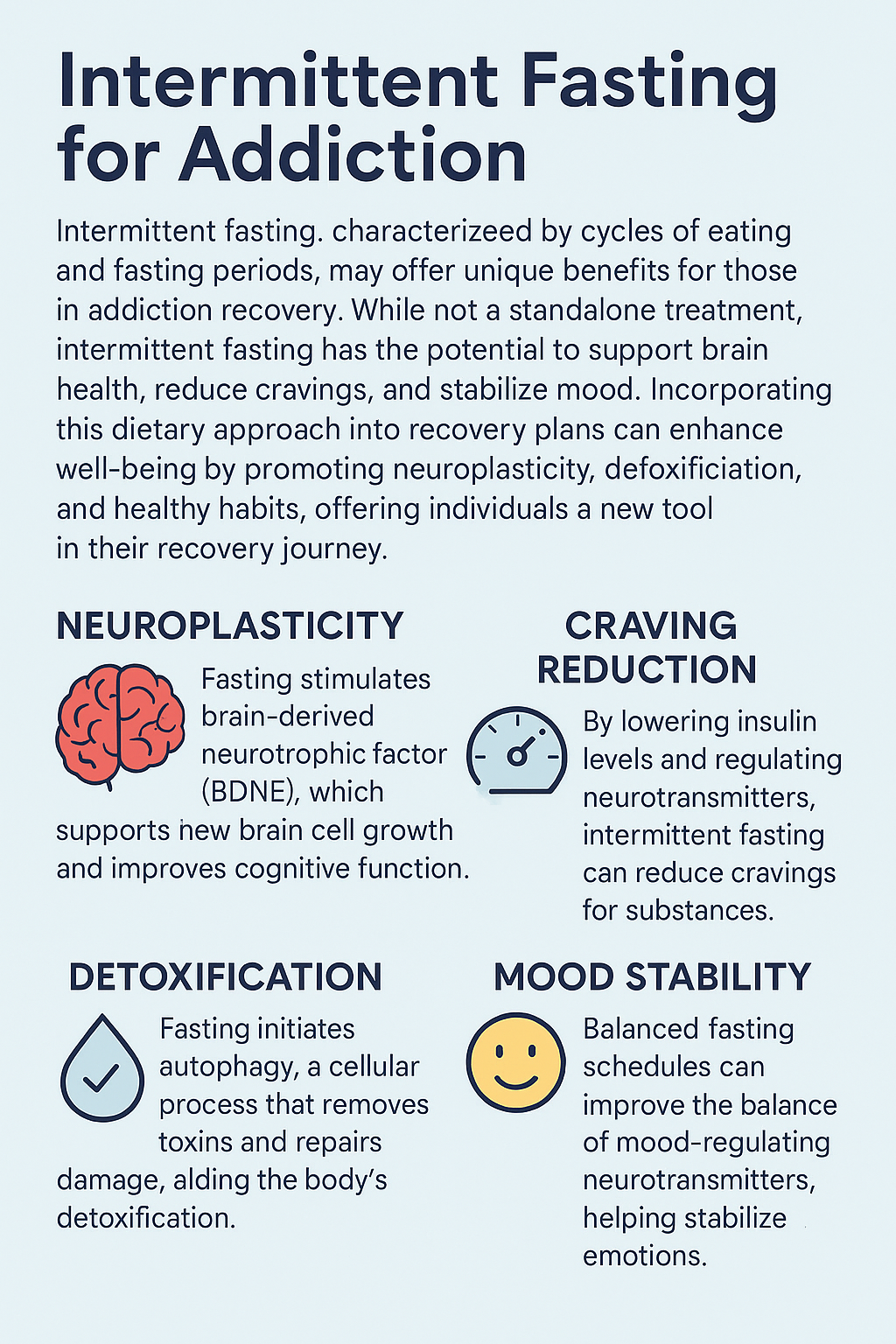
Intermittent fasting (IF)—a dietary approach that alternates between periods of eating and fasting—is gaining attention not only for its physical health benefits but also for its potential to support addiction recovery. Research suggests that intermittent fasting may positively impact brain chemistry, reduce cravings, and promote self-control, offering a complementary approach for individuals overcoming substance use disorders. Here’s a look at how intermittent fasting could aid in addiction treatment:
- Improving Brain Function and Neuroplasticity
- Brain resilience: Intermittent fasting has been shown to increase brain-derived neurotrophic factor (BDNF), a protein essential for neuroplasticity. Enhanced neuroplasticity helps the brain adapt and “rewire,” a crucial factor for individuals in recovery who need to break free from dependency patterns.
- Mood and cognition: By boosting levels of norepinephrine and other mood-enhancing neurotransmitters, intermittent fasting can improve mood and focus. This can help individuals manage withdrawal symptoms and the psychological stress associated with addiction recovery.
- Reducing Cravings by Regulating Dopamine
- Dopamine sensitivity: Substances of abuse often disrupt the brain’s dopamine pathways, creating an exaggerated need for reward. Intermittent fasting may help restore dopamine sensitivity, making the brain less reliant on external substances for pleasure and reducing cravings.
- Curbing impulse control: The practice of fasting requires self-discipline and a delay in gratification, which can build the ability to resist impulsive behaviors—an invaluable skill in addiction recovery.
- Lowering Inflammation and Supporting Mental Health
- Reduced inflammation: Substance use often triggers systemic inflammation, linked to mood disorders and cognitive decline. Intermittent fasting has been shown to lower inflammatory markers, potentially easing both the physical and mental strain of addiction.
- Supporting mental health: Inflammation is closely tied to anxiety and depression—conditions often co-occurring with addiction. By reducing inflammation, intermittent fasting may indirectly improve mental health, aiding individuals as they work to rebuild a stable, healthy life.
- Enhancing Self-Control and Discipline
- Building a sense of agency: The structure of intermittent fasting requires planning and self-discipline, skills that can carry over into other areas of life, including addiction recovery. By practicing self-control, individuals may find it easier to manage cravings and avoid triggers.
- Mindful eating habits: Fasting can increase awareness of eating patterns, encouraging people to reflect on other behaviors, such as substance use. Developing mindfulness around actions and triggers is beneficial in recognizing habits that contribute to addiction.
- Improving Physical Health to Support Recovery
- Weight and metabolic health: Addiction can often negatively affect physical health. Intermittent fasting has been associated with better metabolism, weight loss, and improved blood sugar control. Enhancing physical health can provide a more stable foundation for recovery and improve motivation.
- Promoting better sleep: Studies suggest that intermittent fasting may improve sleep quality, which is essential for emotional regulation and reducing cravings. Better sleep quality is a critical element in addiction recovery, helping individuals manage stress and maintain mental resilience.
Potential Considerations and Challenges
- Individual differences: Intermittent fasting may not work equally well for everyone, and some individuals may experience fatigue or irritability, which could be counterproductive for those in recovery.
- Medical oversight: Given the complexities of addiction and possible health issues, individuals in recovery need to consult healthcare professionals before starting intermittent fasting.
- Avoiding additional stress: For some, restrictive eating can increase stress or anxiety, potentially exacerbating cravings or mental health symptoms. Adopting a flexible, balanced approach is critical to ensuring that fasting remains supportive rather than stressful.
While intermittent fasting is not a stand-alone solution for addiction recovery, it offers promising benefits that may complement traditional treatment approaches. It could be a valuable tool in a comprehensive recovery plan by supporting brain health, reducing cravings, enhancing mental well-being, and promoting physical resilience. As research continues, intermittent fasting may become an increasingly recognized and accessible strategy for individuals in recovery.
The Risks and Drawbacks of Intermittent Fasting in Addiction Recovery: Is It Right for You?
Intermittent fasting (IF) is often promoted for its potential health benefits, including possible support for addiction recovery. However, fasting isn’t without its challenges, particularly for those in recovery from substance use disorders. Here are some critical concerns associated with intermittent fasting in the context of addiction recovery:
- Potential for Increased Stress and Irritability
- Mood swings: IF can lead to fluctuations in blood sugar and energy levels, which may cause irritability, fatigue, or mood swings. Since stress and unstable moods are common relapse triggers, these effects could increase the risk of setbacks for those working on recovery.
- Physical stress: Fasting has been shown to increase cortisol, the body’s primary stress hormone, which may counteract some of the positive effects of addiction treatment. For those in the early stages of recovery, this additional stress may be particularly detrimental as both physical and mental stability are often fragile.
- Risk of Triggering Other Unhealthy Eating Patterns
- Disordered eating: Individuals in recovery may already be susceptible to developing disordered eating habits, and the restrictive nature of fasting could intensify these tendencies. In some cases, intermittent fasting could lead to cycles of binge eating and restriction, which can negatively impact mental and physical health.
- Loss of control: Maintaining a strict fasting schedule may encourage obsessive or unhealthy thoughts about food. This rigidity could cause stress or trigger compulsive behaviors in those with a history of eating disorders, creating additional challenges during recovery.
- Incompatibility with Physical Health Conditions
- Nutritional deficiencies: Fasting can limit the variety and balance of nutrients consumed, leading to potential deficiencies. For individuals in recovery, poor nutrition may weaken the immune system, impact mental health, and slow down the healing process.
- Blood sugar concerns: Fasting can be risky for those with conditions like diabetes or hypoglycemia, as extended fasting periods can lead to dangerously low blood sugar. For individuals in recovery, consistent energy and focus are essential, and blood sugar instability could make recovery efforts harder to maintain.
- Interference with Sleep and Energy Levels
- Sleep disruption: Fasting may disrupt some people’s sleep patterns, as the timing of meals can affect circadian rhythms. Sleep deprivation can affect impulse control, mood, and concentration—all essential for recovery success.
- Reduced energy for recovery activities: Fasting may lower energy levels, affecting participation in physical exercise, therapy sessions, or social interactions—all crucial aspects of a balanced recovery routine. Low energy could lead to decreased motivation and compromise commitment to recovery.
- Impact on Medication Efficacy and Side Effects
- Medication absorption: Some medications, including those for mental health, require food for proper absorption. Fasting may alter the effectiveness of these medications or increase the risk of side effects, potentially complicating recovery.
- Increased side effects: For individuals taking medications for addiction or co-occurring disorders, fasting can increase gastrointestinal discomfort, nausea, or other side effects if medication is taken on an empty stomach.
- Lack of Long-Term Research for Addiction Recovery
- Limited evidence in addiction contexts: While intermittent fasting has been studied in general health contexts, research on its effects on addiction recovery remains limited. The risks and benefits of IF in this setting are poorly understood, making it challenging to establish safe and practical guidelines.
- Potential for relapse triggers: Without extensive research, there’s a risk that fasting could unintentionally trigger cravings or lead to compensatory behaviors that increase relapse risk. Dietary changes can be particularly challenging for individuals sensitive to lifestyle alterations.
- Added Complexity to Recovery Routines
- Overcomplicating recovery: Recovery requires a focus on establishing stability and healing, and fasting adds an extra layer of complexity that may feel overwhelming. Managing a fasting routine alongside recovery activities could increase stress or detract from recovery goals.
- Conflicting focus: Fasting may shift attention toward diet and meal planning rather than recovery, potentially creating stress if the routine becomes rigid or challenging.
While intermittent fasting may offer benefits as a complementary tool for addiction treatment, it carries potential risks that should be carefully considered. Increased stress, nutritional deficiencies, disordered eating patterns, and possible interference with medication all highlight the need for caution. Intermittent fasting may be more suitable as a supplementary approach rather than a core component of addiction treatment, and it should always be tailored to each individual’s needs under professional supervision.
The Risks and Challenges of Using Intermittent Fasting in Addiction Treatment
Intermittent fasting (IF) has gained attention as a potential supportive tool in addiction recovery, with claims that it could help reset the brain, improve mood, and reduce cravings. While IF holds promise, it’s essential to recognize its potential disadvantages and risks, particularly for individuals in recovery. Here are some key concerns to consider before incorporating intermittent fasting into an addiction treatment plan:
1. Potential for Increased Stress and Irritability
- Mood Swings: IF can cause fluctuations in blood sugar and energy levels, potentially leading to mood swings, irritability, and fatigue. These effects can be particularly challenging for individuals in addiction recovery, as stress and unstable emotions are common relapse triggers.
- Physical Stress: Fasting can increase cortisol, the body’s stress hormone, leading to physical stress. This may counteract the benefits of addiction treatment, especially in the early stages of recovery, when individuals are still stabilizing both physically and mentally.
2. Risk of Triggering Unhealthy Eating Patterns
- Disordered Eating: Those in addiction recovery may already be at risk for developing disordered eating habits. Restricting food intake through fasting could exacerbate this issue, possibly leading to cycles of binge eating and restriction that undermine both physical and mental health.
- Loss of Control: A strict fasting schedule might lead to an unhealthy preoccupation with food. This rigidity can lead to obsessive thoughts or compulsive behaviors, particularly for those with a history of co-occurring eating disorders, adding unnecessary stress to the recovery process.
3. Incompatibility with Physical Health Conditions
- Nutritional Deficiencies: Fasting could lead to nutrient deficiencies if meals during eating windows lack variety and balance. This can weaken the immune system, slow recovery, and negatively impact physical and mental health.
- Blood Sugar Concerns: Fasting might be risky for individuals with conditions like diabetes or hypoglycemia, as extended periods without food can lead to dangerously low blood sugar levels. For people in addiction recovery, stable energy levels are crucial for maintaining focus and managing triggers.
4. Interference with Sleep and Energy Levels
- Sleep Disruption: While IF may improve sleep for some, it can disrupt sleep patterns for others. Those who fast too late or too early in the day may struggle to fall asleep, which could negatively impact mood, concentration, and impulse control—critical components of successful addiction recovery.
- Reduced Energy for Recovery Activities: Low energy levels due to fasting could interfere with an individual’s ability to engage in physical exercise, therapy, or social activities—crucial parts of a balanced recovery. This energy reduction could hinder motivation and progress in the treatment process.
5. Impact on Medication Efficacy and Side Effects
- Medication Absorption: Some medications, particularly those for mental health conditions, require food for proper absorption. Fasting may alter the timing and effectiveness of these medications, reducing their therapeutic benefits or increasing the likelihood of side effects.
- Increased Side Effects: For individuals taking medications for addiction or co-occurring disorders, fasting may increase the risk of gastrointestinal discomfort, nausea, or other unpleasant side effects when taken on an empty stomach.
6. Lack of Long-Term Research for Addiction Recovery
- Limited Evidence in Addiction Contexts: While IF has been studied in the context of general health and metabolic conditions, there is limited research on its impact on addiction recovery. The long-term benefits and risks of IF in addiction treatment remain unclear, making it difficult to predict outcomes or establish clear, safe guidelines.
- Potential for Relapse Triggers: Without extensive research, there’s a risk that intermittent fasting could inadvertently trigger cravings or lead to compensatory behaviors that increase the risk of relapse, especially in individuals sensitive to dietary changes.
7. Added Complexity to Recovery Routines
- Overcomplicating Recovery: Addiction recovery often involves significant lifestyle changes, including therapy, support groups, and daily stress management. Introducing fasting into the mix may create additional complexity, overwhelming individuals already adjusting to new routines.
- Conflicting Focus: Addiction recovery focuses on healing, stability, and well-being. Intermittent fasting may shift the focus toward dieting and meal planning, potentially adding stress and detracting from more essential recovery activities, especially if fasting routines become challenging.
While intermittent fasting holds some potential as a complementary tool in addiction treatment, it carries several risks, especially when practiced without professional guidance. The possible increase in stress, risk of nutritional deficiencies, potential disruption of eating habits, and interference with medication and sleep should not be overlooked. IF may be better suited as a supplementary strategy, tailored to individual needs and implemented with careful monitoring by healthcare professionals. As with any recovery approach, it is essential to prioritize overall well-being and stability above all else.
Ethical Concerns of Using Intermittent Fasting in Addiction Treatment
While intermittent fasting (IF) has shown promise in various health contexts, its application in addiction treatment raises several ethical concerns that cannot be ignored. These issues revolve around patient autonomy, health equity, potential harm, and experimental approaches. Here are some of the primary ethical dilemmas that emerge when considering IF as part of addiction recovery:
1. Autonomy and Informed Consent
- Lack of Established Evidence: One of the central ethical concerns is the limited research explicitly addressing the impact of IF on addiction recovery. Patients cannot make fully informed decisions regarding IF’s potential benefits and risks without sufficient evidence. This lack of comprehensive information makes it difficult to obtain valid, informed consent, as patients may not understand it.
- Pressure to Comply: In some structured treatment environments, patients may feel pressured to adopt IF as a treatment method, especially if it is presented as an integral or recommended part of their recovery program. This creates an ethical dilemma, infringing on the patient’s autonomy and right to choose their preferred treatment options.
2. Health Equity and Accessibility
- Socioeconomic Disparities: The practice of IF might be more accessible to individuals with reliable access to nutritious food, which is often a privilege in higher socioeconomic groups. For individuals facing food insecurity, lacking access to healthy food during eating windows could lead to nutritional deficiencies, potentially exacerbating health risks. Promoting IF could unintentionally widen health disparities, favoring those with more resources.
- Cultural and Religious Considerations: Eating patterns are deeply influenced by cultural and religious beliefs, which may directly conflict with fasting practices. They are forcing or recommending IF without considering an individual’s cultural or religious background, which can be regarded as ethically questionable, as it does not respect the person’s values and practices.
3. Potential for Physical and Psychological Harm
- Exacerbation of Health Conditions: Many individuals in addiction recovery have co-occurring physical or mental health conditions such as malnutrition, diabetes, or mood disorders. Fasting could worsen these pre-existing conditions, creating a tension between the potential benefits of fasting for addiction and the risks posed to overall health.
- Risk of Triggering Disordered Eating: Many people recovering from addiction may also have a history of disordered eating behaviors. Intermittent fasting could exacerbate these tendencies, potentially leading to an unhealthy preoccupation with food or triggering eating disorders. Without addressing these risks, IF could cause harm to the mental health of individuals in recovery.
4. Balance of Benefit and Harm
- Insufficient Evidence for Addiction Recovery: While IF has been studied for various health benefits, there is still inadequate research supporting its use specifically for addiction recovery, and recommending or implementing IF without clear evidence of its efficacy and safety in addiction treatment raises ethical concerns about exposing patients to unproven and potentially harmful interventions.
- Complexity and Recovery Focus: Addiction recovery is already a complex process involving therapy, support groups, and significant psychological and lifestyle adjustments. Introducing a strict dietary regimen like IF might increase the emotional and mental burden on individuals, making a recovery more complex. From an ethical standpoint, presenting additional challenges that could complicate the recovery process may be problematic.
5. Ethical Concerns in Research and Experimentation
- Experimental Nature of Treatment: Since IF’s role in addiction treatment has not been well-established through rigorous research, implementing it as part of a treatment plan without long-term evidence raises ethical concerns. Using patients as subjects in experimental treatments without clear evidence of benefits can be ethically questionable.
- Vulnerability in Addiction Recovery: Individuals in addiction recovery are often in a vulnerable state, which makes them more susceptible to trying new treatments without fully understanding the risks involved. There is a responsibility to protect this population from interventions that may not have well-defined benefits or could exacerbate their condition.
6. Resource Allocation and Fairness
- Potential Diversion of Resources: Incorporating IF into addiction treatment could divert valuable resources away from more proven and essential treatment options, such as therapy, medications, and social support. In settings with limited resources, this could limit access to necessary services and undermine the overall efficacy of addiction care.
- Equitable Access to Support for IF: If IF is to be integrated into addiction treatment, adequate resources like nutrition counseling and meal planning must be provided to ensure that all patients can safely and effectively follow the regimen. Lack of access to these services could lead to inequalities and health disparities, further complicating treatment outcomes.
The integration of intermittent fasting into addiction treatment presents complex ethical challenges, primarily due to the lack of conclusive research, potential physical and psychological harms, and concerns about health equity. Issues surrounding patient autonomy, informed consent, and the accessibility of necessary support make it crucial for treatment providers to approach IF cautiously. Ensuring that patients are fully informed, considering their unique health situations, and receiving appropriate resources is necessary for any intervention, particularly one that is still largely experimental. It may hold promise as a complementary tool in addiction recovery, but it should be used judiciously, with full ethical consideration, to avoid potential harm.
Effective Self-Management Strategies for Incorporating Intermittent Fasting into Addiction Treatment
Incorporating intermittent fasting (IF) into addiction recovery can offer significant benefits, but it requires careful self-management to be both effective and safe. Self-discipline, mindful eating, and maintaining physical and mental health are crucial for success. Here are key strategies that can help individuals manage intermittent fasting while supporting their recovery journey:
1. Start Gradually and Customize the Fasting Window
- Ease into Fasting: To minimize side effects like fatigue or irritability, it’s essential to start fasting gradually. Beginning with a 12-hour fast (e.g., 8 PM to 8 AM) and gradually increasing it to 14 or 16 hours allows the body to adjust more easily.
- Choose a Suitable Fasting Schedule: Different IF schedules (e.g., 16:8, 18:6, or 5:2) offer flexibility. The key is to choose one that aligns with your daily routine and addiction recovery plan. Flexibility in fasting schedules reduces stress, ensuring IF complements recovery rather than disrupting it.
2. Focus on Nutrient-Dense Foods During Eating Windows
- Prioritize Balanced Nutrition: Ensure meals contain proteins, healthy fats, fiber, and complex carbohydrates. These nutrients stabilize blood sugar, improve mood, and reduce cravings — all essential for those recovering from addiction.
- Avoid Sugary Foods and Stimulants: Minimize processed foods and excess caffeine, which can cause blood sugar fluctuations and increase cravings. Whole foods like vegetables, fruits, lean proteins, and whole grains help maintain steady energy and emotional balance.
3. Practice Mindful Eating and Drinking
- Avoid Binge Eating: Mindful eating helps prevent overeating during eating windows, which can lead to digestive discomfort, energy crashes, and feelings of guilt. Focus on eating slowly and savoring each meal.
- Hydrate Consistently: Proper hydration is critical during critical periods. Drinking water, herbal teas, or other non-caloric beverages can reduce hunger pangs, keep you hydrated, help maintain mental clarity, and reduce impulsive cravings.
4. Set Clear Goals and Monitor Progress
- Track Fasting and Recovery Goals: Logging fasting hours, meal quality, cravings, and moods in a journal or app can help identify patterns. Tracking progress boosts motivation and highlights the positive effects of IF on addiction recovery and overall health.
- Be Mindful of Mental Health: Regular self-check-ins are essential to ensure that IF is not leading to irritability, mood swings, or heightened cravings. Staying in tune with emotional and mental well-being allows for adjustments to the fasting regimen when necessary.
5. Prioritize Sleep and Rest
- Maintain Consistent Sleep Patterns: Good sleep is crucial for addiction recovery and successful fasting. Poor sleep can increase cravings, impair impulse control, and make fasting harder to manage. Aim for a consistent bedtime routine and prioritize restful sleep.
- Listen to Your Body: If fasting leads to excessive fatigue or stress, consider shortening the fasting window or taking a break from fasting. The focus should always be on long-term recovery, and fasting should not compromise physical or mental health.
6. Incorporate Stress-Relief Practices
- Practice Mindfulness and Stress Management: Techniques like meditation, deep breathing, and yoga can help lower stress levels, making it easier to maintain fasting and recovery routines. Reduced stress can also lessen the risk of triggering cravings.
- Engage in Supportive Activities: Spend time with family, friends, or support groups. These relationships provide emotional support, promote self-discipline, and offer a healthy distraction from cravings and fasting challenges.
7. Cultivate Positive Self-Discipline and Flexibility
- View fasting as Part of a Holistic Recovery Plan: Approach fasting as a complementary tool for recovery rather than a rigid rule. Flexibility is key. This mindset allows for adjustments to the fasting schedule, helping individuals remain relaxed and focused on overall well-being.
- Reward Self-Control: Celebrating small victories, like completing a fast or choosing a healthy meal, can reinforce positive behaviors and boost confidence. Acknowledging these achievements fosters a sense of accomplishment and control.
8. Seek Support and Accountability
- Share Goals with a Support Network: Tell friends, family, or a support group about your decision to incorporate IF into your recovery. Having a support system provides accountability and encouragement, especially during challenging moments.
- Consider Professional Guidance: Consulting with healthcare providers, nutritionists, or addiction counselors ensures your IF plan is tailored to your needs. Professional support helps ensure that the fasting approach is beneficial and safe for your mental and physical health.
9. Practice Self-Compassion and Adjust as Needed
- Accept Setbacks as Part of the Process: Recovery is a gradual journey, and occasional setbacks are normal. Practice self-compassion by learning from setbacks rather than criticizing yourself. Resilience grows from understanding that progress is not always linear.
- Adjust Fasting as Needed: If intermittent fasting becomes overwhelming or negatively affects your recovery, don’t hesitate to modify or take a break from fasting. Prioritize mental health and well-being, as they are essential for long-term recovery.
Self-management strategies are essential for effectively incorporating intermittent fasting into addiction treatment. By gradually adopting a personalized fasting schedule, prioritizing nutrition, managing stress, and seeking support, individuals can use IF to support their recovery journey. Flexibility, mindfulness, and self-compassion make fasting a sustainable and empowering tool, helping individuals build self-discipline, reduce cravings, and enhance both physical and mental health as they progress through addiction recovery.
The Vital Role of Family Support in Implementing Intermittent Fasting in Addiction Treatment
Family support is a cornerstone of successful addiction recovery, and it plays a crucial role when integrating intermittent fasting (IF) as a complementary treatment. Intermittent fasting can be a powerful tool for those in recovery, but it requires the right kind of support to be effective and sustainable. Family members can provide emotional, practical, and motivational support, helping ensure that fasting is practiced in a balanced, manageable way. Here are several strategies for family members to support their loved ones as they integrate IF into their addiction treatment:
1. Encouragement and Emotional Support
- Positive Reinforcement: Family members can help by offering consistent encouragement and celebrating small milestones, such as completing a fasting window or making healthy food choices. Recognizing progress boosts self-esteem and motivation, which is essential for fasting and recovery efforts.
- Emotional Reassurance: Addiction recovery is emotionally taxing, and fasting might add additional stress. By being empathetic and patient, family members can create a supportive environment where the individual feels understood and not judged, strengthening their commitment to their recovery and fasting goals.
2. Creating a Supportive Environment at Home
- Meal Planning and Preparation: An essential support strategy is helping to plan and prepare nutritious, balanced meals during eating windows. This allows the individual to focus on recovery without the added pressure of meal planning, ensuring they can maintain a healthy eating routine that aligns with their fasting schedule.
- Avoiding Triggers: Family members should work to create a home environment free of addiction-related triggers, such as substances or behaviors that could undermine both the fasting and recovery process. A calm, supportive environment makes it easier for individuals to stick to their fasting schedule and focus on their recovery goals.
3. Promoting Healthy Habits and Routines
- Establishing a Routine: Encouraging a structured daily routine that includes designated times for fasting, meals, exercise, and rest can help reinforce both the fasting regimen and addiction recovery. Consistency in daily habits supports long-term success in both areas.
- Encouraging Balanced Nutrition: Ensuring that meals are nutrient-dense, with proteins, healthy fats, fiber, and complex carbohydrates, helps stabilize blood sugar, support mental health, and reduce cravings. Family members can provide valuable support in ensuring meals are balanced and aligned with health goals.
4. Stress Management and Coping Skills
- Supporting Stress Relief Practices: Both addiction recovery and fasting can be stressful, so it’s essential to engage in stress-relief activities. Family members can encourage mindfulness, relaxation techniques, exercise, or hobbies to reduce stress. Participating in these activities together can strengthen family bonds and help alleviate anxiety related to fasting or recovery.
- Being a Sounding Board: Having someone to talk to can help individuals process frustrations and challenges related to fasting or recovery. Family members can offer a listening ear, providing emotional relief and keeping the individual focused on their goals.
5. Accountability and Motivation
- Setting Joint Goals: Working together as a family to set mutual health and wellness goals, such as adopting healthier eating habits or exercising together, fosters a sense of shared accountability. This can make it easier for the individual to stick to their fasting plan while strengthening family connections.
- Monitoring progress together: Regular check-ins about fasting schedules and recovery progress help to keep everyone on track. Gentle reminders or encouragement from family members can offer much-needed motivation while also making necessary adjustments to ensure success.
6. Respecting Boundaries and Autonomy
- Encouraging Without Pressuring: Family members should offer support and encouragement, but must respect the individual’s autonomy in their recovery and fasting journey. Pressuring or forcing fasting could lead to resistance or feelings of failure, so it’s crucial to allow the individual to make decisions about fasting within a supportive framework.
- Flexibility and Understanding: If fasting becomes overwhelming, family members should remain flexible and understanding, offering to adjust the fasting plan or temporarily pause it. Being adaptable ensures the individual feels supported rather than forced and helps avoid burnout.
7. Providing Practical Help During Fasting Periods
- Managing Fasting-Related Difficulties: Fasting can be challenging, especially in the early stages. Family members can help by taking on additional responsibilities or reducing the individual’s workload during fasting periods. This alleviates stress and helps them focus on maintaining their fasting schedule.
- Ensuring Hydration: Encouraging consistent hydration during fasting periods can help manage hunger and stabilize energy levels. Family members can remind the individual to drink water, herbal teas, or other non-caloric beverages to ease fasting discomfort and maintain mental clarity.
8. Facilitating Open Communication
- Encouraging Open Dialogue: Open communication ensures the individual feels supported and understood. Family members should create a space where the person can talk about challenges, cravings, or frustrations related to fasting or addiction recovery. This allows for real-time adjustments to the fasting plan and ensures that the individual doesn’t feel alone.
- Providing Constructive Feedback: Offering positive reinforcement alongside thoughtful feedback helps the individual feel supported rather than criticized. Celebrating successes and constructively discussing areas for improvement can boost the individual’s confidence and keep them on track with fasting and recovery goals.
9. Creating a Support Network
- Engaging in Recovery Programs Together: Families can join addiction recovery programs (such as group therapy or support groups), creating a robust support system that strengthens recovery and fasting goals. Shared participation reinforces healthy lifestyle choices and helps the individual feel supported.
- Seeking Professional Guidance: Sometimes, professional input from a healthcare provider or addiction counselor is necessary to ensure that intermittent fasting suits the individual’s health needs. Family members can assist in ensuring that the fasting plan aligns with professional advice to ensure safety and effectiveness.
Family support is essential when integrating intermittent fasting into addiction treatment. By providing encouragement, practical help, emotional reassurance, and maintaining a structured environment, family members can ensure that fasting is a sustainable and valuable part of the recovery process. With a solid support system in place, individuals can better navigate the challenges of addiction recovery and intermittent fasting, fostering long-term success and well-being.
Leveraging Community Resources to Integrate Intermittent Fasting into Addiction Treatment
Incorporating intermittent fasting (IF) into addiction treatment can provide a holistic approach to recovery, fostering both physical and emotional health. However, successfully adopting fasting as a recovery tool requires access to appropriate guidance and emotional support. Community resources play a vital role in ensuring individuals have these tools at their disposal, helping to create a supportive environment that promotes sustainable health practices, including fasting. Below are several vital community essential sources that can aid in the integration of intermittent fasting into addiction treatment:
1. Support Groups and Peer Networks
- Addiction Recovery Support Groups: Community-based support groups such as Narcotics Anonymous (NA), Alcoholics Anonymous (AA), and other recovery-focused programs provide invaluable peer support. These groups offer shared experiences, encouragement, and emotional reinforcement, strengthening the individual’s commitment to fasting and sobriety.
- Fasting-Focused Support Groups: Specialized groups focused on intermittent fasting may also be available in some communities. These groups connect individuals who are using IF to support their overall well-being. Sharing experiences, challenges, and success stories can help participants stay motivated and informed about combining fasting with recovery.
2. Healthcare and Wellness Services
- Nutrition Counseling and Dietitian Services: Many communities offer access to nutritionists or dietitians who can help individuals integrate intermittent fasting with a balanced, nutrient-dense diet. These professionals can create personalized meal plans that ensure nutritional balance while mitigating the risks associated with fasting, especially for individuals in recovery from addiction.
- Addiction Treatment Centers: Some addiction treatment centers offer integrated programs that include intermittent fasting as a complementary therapy. These centers provide medical supervision, counseling, and mental health care, ensuring that fasting is done safely and effectively as part of the recovery process.
- Mental Health Services: Mental health counseling can be essential for those struggling with the emotional challenges of addiction recovery and fasting. Community-based mental health services can provide the necessary psychological support to help individuals cope with stress, cravings, and the emotional side effects of fasting.
3. Educational Programs and Workshops
- Public Health Education: Community centers, health departments, or nonprofit organizations may offer workshops or seminars on the benefits and risks of intermittent fasting, particularly in addiction treatment. These programs provide essential information to help individuals make informed decisions about incorporating fasting into their recovery plan.
- Addiction Recovery and Lifestyle Workshops: Local organizations often host workshops focusing on addiction recovery and lifestyle changes, including nutrition, exercise, and fasting. These educational resources provide a comprehensive, holistic approach to health, empowering individuals to take control of their well-being.
4. Fitness and Wellness Programs
- Community Fitness Programs: Physical exercise is an essential component of addiction recovery, and it complements intermittent fasting by enhancing both physical and mental well-being. Many communities offer group exercise classes, yoga, or walking groups that provide social support while promoting overall health, thereby reinforcing fasting practices.
- Wellness Centers: Wellness centers offer various services, such as fitness training, meditation, and mindfulness practices, all of which support the goals of intermittent fasting. These services reduce stress, manage cravings, and help individuals balance fasting and recovery.
5. Access to Professional Supervision
- Collaborative Care with Addiction Specialists: Addiction specialists can collaborate with healthcare providers to monitor individuals practicing intermittent fasting. These specialists ensure that fasting does not interfere with recovery or exacerbate mental health issues, guiding the integration of fasting safely and beneficially.
- Medical Support for Co-occurring Conditions: Many individuals in recovery may also have co-occurring physical or mental health conditions. Community health centers can provide medical care for these conditions, ensuring that fasting complements other treatments and does not worsen health concerns.
6. Access to Food and Nutritional Support
- Food Assistance Programs: Some communities have food banks or government-sponsored programs that provide access to healthy food. These resources help individuals in addiction recovery maintain a balanced diet during eating windows, ensuring they have the nutrition to support fasting and recovery.
- Community Nutrition Programs: Meal programs or food vouchers can assist individuals who may not have the resources to purchase nutritious food during fasting periods. These programs support the long-term success of fasting by ensuring individuals stay nourished and avoid the risks of undernutrition.
7. Public Policy and Advocacy
- Advocacy for Better Health Services: Community organizations can advocate for improved access to addiction treatment and holistic health services, including those integrating fasting and nutrition. This advocacy helps ensure that individuals in recovery have the resources they need to succeed in both addiction recovery and overall health.
- Creating Supportive Community Policies: Local governments and organizations can implement policies that promote access to health services, including wellness programs, mental health care, and addiction treatment, which support practices like intermittent fasting as part of addiction recovery.
8. Access to Online Resources and Digital Tools
- Online Education and Support Groups: Many communities provide online platforms that offer educational resources, virtual meetings, and peer support groups for individuals incorporating intermittent fasting into their addiction treatment. These platforms make it easier for individuals to connect with others and access valuable resources, especially in areas where in-person support may be limited.
- Mobile Apps for Fasting and Addiction Recovery: Some community programs promote mobile apps to track fasting schedules, meal plans, and recovery goals. These apps offer motivational support, reminders, and guidance to help individuals stay on track and successfully integrate intermittent fasting into their recovery journey.
9. Spiritual and Religious Support
- Faith-Based Recovery Programs: Some communities offer faith-based addiction recovery programs that may include fasting as part of a spiritual healing process. These programs offer individuals a sense of purpose and connection, providing additional support in their fasting and recovery journey.
- Spiritual Counseling: Community churches or religious organizations may offer counseling, group sessions, and spiritual practices for individuals seeking spiritual guidance. These services can provide emotional support and complement the goals of intermittent fasting in addiction treatment.
Community resources are essential for supporting the integration of intermittent fasting into addiction treatment. By providing educational programs, healthcare services, peer support, and fitness opportunities, these resources create a comprehensive support system that helps individuals successfully combine fasting with their recovery efforts. Access to these community-based services ensures that individuals in recovery have the tools, knowledge, and support needed to achieve long-term health and wellness. By leveraging the support of the community, individuals can integrate intermittent fasting into their addiction recovery journey safely and effectively.
Conclusion
While intermittent fasting can offer benefits in managing addiction by improving physical health, reducing cravings, and enhancing mental clarity, it also presents challenges, such as health risks and ethical dilemmas around autonomy and psychological well-being. For IF to be effective in addiction recovery, self-management strategies, family support, and community resources are crucial. Through careful monitoring, emotional encouragement, and access to professional guidance, individuals can navigate these challenges, making IF a viable complement to traditional addiction treatment when approached responsibly and holistically.
Video: 5 Secrets of Successful Recovering Addicts Who Use Intermittent Fasting