Intensive Outpatient Programs (IOPs) provide structured addiction treatment with flexibility for individuals to maintain daily routines. Offering more support than traditional outpatient therapy but less than inpatient care, IOPs include a range of therapies and peer support. However, challenges such as limited crisis support, varying program quality, and ethical issues related to autonomy can arise. By focusing on self-management and incorporating family and community resources, IOPs effectively support long-term sobriety and well-being.
The Structure and Benefits of Intensive Outpatient Programs (IOPs) for Addiction Recovery
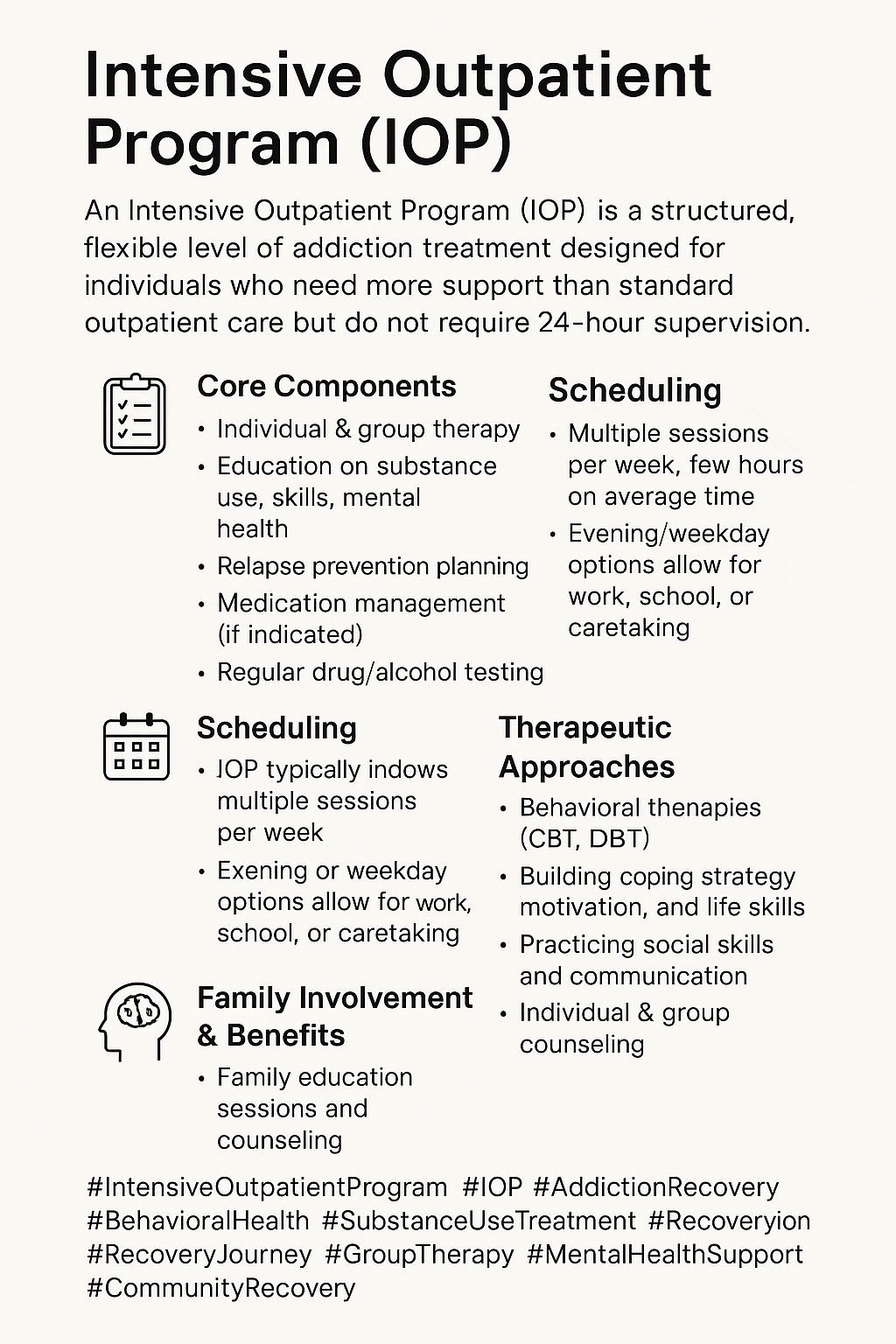
Intensive Outpatient Programs (IOPs) offer structured treatment for individuals struggling with addiction while allowing them to maintain a level of daily functioning. IOPs are ideal for those needing more support than traditional outpatient therapy but not the 24-hour care provided by inpatient facilities. Here’s a look at what IOPs typically offer:
Key Features of Intensive Outpatient Programs
1. Frequency and Duration
- Session Frequency: IOPs typically involve 3 to 5 weekly sessions, each lasting 2 to 4 hours, providing consistent support.
- Program Length: Generally, IOPs last several weeks to a few months, with the duration adjusted based on individual needs.
2. Comprehensive Treatment
- Therapeutic Approaches: Treatment includes individual, group, and family therapy, with evidence-based practices like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT).
- Focus on Co-Occurring Disorders: Many IOPs provide integrated treatment for addiction and co-occurring mental health disorders.
3. Personalized Treatment Plans
- Individualized Approach: Plans are tailored to each participant’s substance use history, goals, and underlying issues.
- Regular Assessments: Ongoing assessments allow for adjustments based on participant progress.
4. Supportive Environment
- Peer Support: Group therapy fosters community, offering a support network among peers.
- Family Involvement: Programs often encourage family participation to reinforce supportive home environments.
5. Life Skills Development
- Skill-Building Activities: IOPs teach coping skills, relapse prevention, and life skills to help participants navigate daily triggers.
- Focus on Re-Integration: Support is provided as participants reintegrate into daily life, including work and relationships.
6. Flexibility and Accessibility
- Part-Time Commitment: IOPs allow individuals to maintain other responsibilities, making them accessible for those with jobs, school, or family duties.
- Variety of Locations: Programs are available in diverse settings, including hospitals, mental health centers, and private practices.
Benefits of Intensive Outpatient Programs
IOPs offer effective treatment for moderate to severe substance use disorders and are often more affordable than inpatient options. The supportive group environment helps reduce feelings of isolation, fostering a sense of community essential to recovery.
In summary, intensive Outpatient Programs offer a flexible, supportive approach to addiction recovery. By combining structured treatment with the opportunity for community connection and skill-building, IOPs empower individuals to achieve and maintain recovery in their daily lives.
Disadvantages of Intensive Outpatient Programs (IOPs) in Addiction Treatment
While Intensive Outpatient Programs (IOPs) offer structured support for individuals in addiction recovery, they also present challenges that may impact their effectiveness and suitability for some individuals. Here are key disadvantages to consider:
1. Limited Structure Compared to Inpatient Care
- Less Supervision: IOPs lack 24-hour supervision, making them less suitable for those with severe addiction or high relapse risk.
- Need for Self-Motivation: Success in an IOP requires participants to manage their addiction outside treatment hours, which may be challenging for some.
2. Potential for Relapse
- Exposure to Triggers: Participants remain in their usual environments, facing familiar triggers and stressors, which can increase relapse risk, especially in unstable settings.
- Gradual Reintegration Challenges: Applying treatment skills in real-world situations can be difficult and may not provide the structured reintroduction some need.
3. Variable Treatment Quality
- Inconsistent Standards: Treatment quality varies by facility and staff expertise, affecting program effectiveness.
- Lack of Accreditation: IOPs may lack consistent standards without universal accreditation, raising concerns about treatment reliability.
4. Cost Considerations
- Insurance Limitations: Insurance may not always cover IOPs, leading to high out-of-pocket costs for some.
- Additional Expenses: Costs like transportation, childcare, or missed work can add up, creating barriers to consistent attendance.
5. Time Commitment
- Scheduling Challenges: Multiple weekly sessions can be challenging to fit into busy schedules, especially for those with work or family commitments.
- Inconvenience: Accessibility issues may arise for participants far from program locations.
6. Emotional Challenges
- Difficult Conversations: Group therapy can bring up personal or distressing topics that may be challenging to confront.
- Group Dynamics: Group therapy effectiveness can vary; some may feel uncomfortable sharing, which can impact their engagement.
7. Not Suitable for Everyone
- Severity of Addiction: IOPs may not be adequate for individuals with severe addiction or mental health issues that require more intensive care.
- Need for a Support System: Those without a stable, supportive home environment may struggle in an IOP.
8. Potential Overlap with Other Treatments
- Conflicting Therapies: When participants engage in other treatments, such as medication management or outpatient therapy, they may face challenges coordinating these modalities.
While IOPs can be effective for many, understanding their limitations is crucial when considering them as a part of an addiction treatment plan. Evaluating both benefits and challenges helps ensure individuals receive the most appropriate level of care for their unique needs.
Ethical Dilemmas in Intensive Outpatient Programs (IOPs) for Addiction Treatment
Intensive Outpatient Programs (IOPs) provide a flexible approach to addiction treatment, yet they also come with ethical challenges that impact both treatment quality and participant well-being. Here are some critical ethical concerns to consider:
1. Equity and Access
- Barriers to Access: IOPs are not equally accessible to everyone, especially those in underserved communities without sufficient insurance. This raises ethical questions about fairness and equal treatment opportunity.
- Financial Constraints: Transportation costs, lost wages, and out-of-pocket fees can exclude low-income individuals, highlighting disparities in access to care.
2. Quality and Standards of Care
- Inconsistent Quality: Without standard accreditation, the quality of IOPs varies, raising ethical concerns if participants receive inadequate care.
- Use of Evidence-Based Practices: Ethical issues arise when programs don’t adhere to evidence-based methods, as this can reduce treatment effectiveness.
3. Pressure to Adhere to Treatment
- Participation Expectations: Participants may feel pressured to attend sessions or follow treatment activities rigidly, which can cause stress, particularly if they are struggling.
- Lack of Individualization: Standardized approaches may not meet each participant’s unique needs, raising ethical questions about informed consent and personalized care.
4. Confidentiality and Privacy
- Group Therapy Dynamics: Maintaining confidentiality in group settings can be challenging, as participants may feel uncomfortable discussing sensitive issues with peers.
- Sensitive Information Handling: Ethical concerns arise when staff fail to protect confidentiality, which could undermine trust and hinder effective treatment.
5. Conflict of Interest
- Financial Incentives: Ties to specific treatment products or methods can create conflicts of interest, potentially leading to treatment recommendations that are not in participants’ best interests.
- Trainer Bias: Trainers’ backgrounds may influence treatment approaches, raising ethical concerns if personal preferences overshadow participants’ well-being.
6. Relapse and Accountability
- Responsibility for Relapse: Ethical issues arise if relapse is framed as a personal failure, ignoring external factors that contribute. This can increase feelings of shame and reduce motivation.
- Support in Crisis: Inadequate support during crises poses ethical dilemmas, as participants may lack the assistance they need when they are most vulnerable.
7. Cultural Competence
- Ignoring Cultural Context: Programs that overlook cultural differences or diverse needs risk marginalizing participants and raising ethical concerns about inclusivity and effectiveness.
- Overgeneralized Approaches: Applying a one-size-fits-all model can perpetuate ethical issues, failing to recognize the unique social and economic backgrounds that influence recovery.
8. Outcome Measurement and Evaluation
- Measuring Success: Ethical questions arise from reliance on subjective self-reports to gauge program success, which may not fully reflect participants’ progress.
- Responsibility for Outcomes: When IOPs don’t yield positive results, ethical issues arise regarding accountability and staff responsibility for improving care quality.
Ethical dilemmas in IOPs for addiction treatment underscore the complexities of delivering effective, compassionate care. Recognizing and addressing these ethical issues can help improve IOPs, fostering a more moral, supportive environment for individuals on their recovery journey.
The Advantages of Intensive Outpatient Programs (IOPs) for Addiction Recovery
Intensive Outpatient Programs (IOPs) are a valuable treatment option for those seeking help for addiction while continuing to meet daily responsibilities. These programs offer flexibility, accessibility, and comprehensive care, making them an appealing option for individuals in recovery. Here’s a closer look at the primary benefits of IOPs:
1. Flexibility and Accessibility
- Part-Time Commitment: IOPs require fewer weekly hours than inpatient programs, enabling participants to balance treatment with work, school, and family obligations.
- Wide Availability: Offered in hospitals, community health centers, and private practices, IOPs are often accessible in various locations, allowing individuals to choose a setting that fits their needs.
2. Comprehensive Treatment
- Holistic Approach: IOPs address multiple facets of recovery by providing individual counseling, group therapy, family involvement, and psychoeducation, helping participants tackle addiction from all angles.
- Treatment for Co-Occurring Disorders: Many IOPs are structured to support mental health needs alongside addiction, providing integrated care for those dealing with both.
3. Supportive Environment
- Peer Connections: Group therapy fosters a community where participants share experiences, offering mutual support and motivation in a judgment-free setting.
- Family Engagement: Many IOPs recognize the importance of family and invite family participation, creating a supportive home environment that enhances recovery.
4. Skill Development
- Life Skills Training: IOPs often incorporate life skills, coping mechanisms, and relapse prevention strategies to help participants manage everyday stressors.
- Trigger Management: Participants learn to identify and manage triggers, thereby reducing the risk of relapse over time.
5. Cost-Effectiveness
- Affordable Alternative: Compared to inpatient programs, IOPs are generally cheaper. They provide structured support without the high costs of residential treatment.
- Insurance Coverage: Many insurance providers cover IOPs, making treatment accessible for those seeking affordable recovery options.
6. Emphasis on Personal Responsibility
- Self-Management Skills: IOPs encourage self-reliance by promoting self-management and accountability, empowering participants to maintain sobriety independently.
- Gradual Reintegration: By being flexible and practicing skills in real-life situations, participants can gradually reintegrate into daily life, reinforcing their recovery skills.
7. Reduced Stigma
- Less Intensive Setting: IOPs are seen as a less stigmatizing alternative to inpatient care, making them a more approachable option for individuals who may be hesitant to seek help.
8. Continuous Support
- Frequent Check-Ins: Regular interaction with counselors and peers provides ongoing support and helps address any emerging challenges.
- Crisis Intervention: Many IOPs offer emergency support services, ensuring participants can access assistance when needed.
9. Tailored Treatment Plans
- Personalized Care: IOPs develop individualized treatment plans based on each participant’s needs, making the program more relevant and effective.
Intensive Outpatient Programs are an adaptable, supportive, and effective treatment option for individuals facing addiction. By combining comprehensive care with the ability to maintain daily responsibilities, IOPs offer a valuable pathway to recovery, equipping participants with the skills and confidence to achieve long-term sobriety.
Self-Management Strategies in Intensive Outpatient Programs: Empowering Individuals for Lasting Recovery
Self-management is a critical component in Intensive Outpatient Programs (IOPs) for addiction recovery, empowering individuals to take control of their healing journey actively. By focusing on personal goal-setting, coping techniques, and life skills, these strategies are designed to build resilience and equip participants with practical tools to manage triggers and maintain long-term sobriety. Here are some essential self-management strategies emphasized in IOPs:
1. Goal Setting
- SMART Goals: IOPs encourage participants to set SMART (Specific, Measurable, Achievable, Relevant, and Time-bound) goals, which provide direction and a clear path for progress.
- Personalized Goals: Tailoring goals to each individual’s unique challenges keeps them motivated and accountable.
2. Coping Strategies
- Developing Coping Skills: IOPs offer techniques like mindfulness, deep breathing, and grounding exercises to help individuals manage cravings and stress effectively.
- Relapse Prevention Plans: By identifying personal triggers and crafting prevention plans, participants gain confidence in navigating high-risk situations.
3. Self-monitoring and Reflection
- Journaling: Tracking thoughts, emotions, and experiences fosters self-awareness and encourages reflection on progress.
- Regular Check-Ins: Tools like mood charts or self-assessments can reveal emotional patterns, offering early insight into potential triggers or relapse risks.
4. Healthy Lifestyle Choices
- Nutrition and Exercise: A balanced diet and regular physical activity can reduce stress, improve mood, and boost overall well-being.
- Sleep Hygiene: Understanding the importance of quality sleep helps participants improve mental and physical health.
5. Building a Support Network
- Identifying Supportive Relationships: Participants are encouraged to surround themselves with friends, family, or mentors who support their recovery journey.
- Engaging in Support Groups: Programs like AA or NA provide a network of peers who understand the challenges of recovery and offer empathy and guidance.
6. Time Management and Structure
- Creating Routines: A consistent routine adds stability, helping participants focus on their recovery goals.
- Prioritizing Activities: Emphasizing recovery-related activities, such as therapy sessions and support meetings, reinforces a commitment to sobriety.
7. Crisis Management Skills
- Developing Emergency Plans: Participants are equipped with strategies for handling crises and managing unexpected triggers that could jeopardize recovery.
- Knowing When to Seek Help: Recognizing when additional support is needed empowers individuals to reach out and access resources in difficult moments.
8. Mindfulness and Stress Reduction Techniques
- Mindfulness Practices: Meditation and yoga reduce cravings and enhance self-awareness, helping participants manage stress effectively.
- Relaxation Techniques: Techniques like progressive muscle relaxation and visualization support individuals in managing anxiety and emotional distress.
9. Educational Workshops
- Learning About Addiction: Educational sessions on addiction and the brain’s response to substances deepen participants’ understanding of their condition and empower their recovery journey.
- Skill-Building Workshops: Workshops on communication, problem-solving, and conflict resolution improve personal and interpersonal dynamics.
Self-management strategies within Intensive Outpatient Programs empower participants to actively engage in their recovery process. IOPs equip individuals with the tools to overcome challenges, manage triggers, and build a strong foundation for long-term sobriety by fostering essential skills such as goal-setting, coping mechanisms, healthy lifestyle choices, and support networks. These strategies are critical to fostering resilience and promoting personal growth throughout recovery.
The Importance of Family Support in Intensive Outpatient Programs for Addiction Recovery
Family support is a powerful asset in the success of Intensive Outpatient Programs (IOPs) for addiction treatment. When family members actively engage in recovery, they contribute to a more robust support network, fostering a more positive and stable environment for their loved ones. Here are several key family support strategies that enhance the recovery process within IOPs:
1. Family Therapy Sessions
- Structured Communication: Family therapy improves communication and helps family members address issues that may contribute to addiction.
- Conflict Resolution: Through therapy, families learn conflict resolution techniques, creating a healthier, more supportive home environment.
2. Education and Awareness
- Understanding Addiction: Family members gain insight into addiction and the recovery process, reducing stigma and fostering empathy.
- Learning Coping Strategies: Education equips families with skills to effectively support their loved ones while managing their own mental health.
3. Involvement in Treatment Planning
- Collaborative Goals: Including family in treatment planning helps shape realistic goals that support positive changes.
- Encouragement of Growth: Family involvement in goal-setting reinforces the individual in recovery’s motivation and accountability.
4. Support Groups for Families
- Peer Support: Family support groups connect with others who understand the challenges of addiction recovery, offering comfort and advice.
- Resource Sharing: Groups often share valuable resources and coping techniques to help families manage stress and support their loved ones.
5. Open Communication Channels
- Regular Check-Ins: Maintaining consistent communication strengthens family bonds, addressing concerns, and celebrating progress.
- Encouraging Honesty: Fostering honest communication builds trust and enhances the recovery experience.
6. Creating a Supportive Home Environment
- Substance-Free Space: A home free from drugs and alcohol supports recovery and reduces potential triggers.
- Routine and Stability: Establishing daily routines can provide a sense of normalcy and support for individuals in recovery.
7. Encouraging Active Participation
- Engagement in Treatment: Family members participating in treatment sessions or educational workshops contribute positively to recovery.
- Attendance at Family Days: Family days allow families to learn more about addiction, reinforcing their role as allies in recovery.
8. Addressing Family Dynamics
- Identifying Patterns: Understanding dysfunctional roles or patterns within the family can promote healthier interactions.
- Setting Boundaries: Learning to set boundaries prevents enabling behaviors and encourages accountability.
9. Crisis Management Strategies
- Preparedness: Educating families on crisis management helps them handle challenging situations, which reduces relapse risk.
- Access to Resources: Knowing how to contact emergency support (counselors or hotlines) provides security during crises.
Family support strategies are vital in enhancing the recovery experience in Intensive Outpatient Programs. By creating an environment grounded in open communication, education, and active engagement, families can provide the necessary support for lasting recovery. Embracing these strategies within IOP strengthens the family bond, equipping everyone involved with the tools needed for long-term success.
Leveraging Community Resources in Intensive Outpatient Programs for Comprehensive Addiction Recovery Support
Community resource strategies in Intensive Outpatient Programs (IOPs) play a critical role in supporting individuals through addiction recovery. By connecting participants with local services and support networks, IOPs help build a comprehensive foundation for treatment and promote long-term recovery. Here are some key community resource strategies commonly integrated within IOPs:
1. Collaboration with Local Organizations
- Partnerships with Nonprofits: Many IOPs collaborate with nonprofit organizations specializing in addiction recovery, mental health, housing assistance, and employment support, giving participants access to a broader range of services.
- Referral Networks: IOPs often establish networks that connect participants with specialized services, such as detox programs, rehab centers, and counseling, for additional, tailored support.
2. Access to Support Groups
- Local Support Meetings: IOPs provide participants with information on community groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), encouraging peer-led support beyond structured treatment.
- Family Support Groups: Connecting families with local support groups offers a platform for shared experiences, insights, and encouragement as they support their loved ones in recovery.
3. Educational Resources
- Workshops and Seminars: IOPs can host community-led workshops on addiction, recovery skills, and coping techniques, often bringing in local experts to enhance learning.
- Information Dissemination: IOPs help participants deepen their understanding of addiction and develop recovery strategies by providing pamphlets, online resources, and reading materials.
4. Employment and Vocational Services
- Job Training Programs: Partnerships with local training programs enable participants to acquire job skills essential for achieving independence and stability.
- Career Counseling: Access to career counseling assists participants in job searching, resume building, and interview preparation, helping them rebuild their professional lives.
5. Mental Health and Counseling Services
- Integrated Care Models: Collaborating with mental health agencies allows IOPs to offer integrated treatment for co-occurring disorders, recognizing the importance of comprehensive care for substance use recovery.
- Access to Psychiatrists: Ensuring participants have access to psychiatric services for medication management can significantly improve treatment outcomes for those with underlying mental health needs.
6. Housing Assistance
- Transitional Housing Programs: Partnering with transitional housing programs offers participants a safe, supportive living environment essential for recovery and stability.
- Permanent Housing Resources: IOPs can guide participants to resources that help secure stable, permanent housing, a crucial factor in maintaining recovery progress.
7. Health and Wellness Programs
- Physical Health Resources: Access to medical services, wellness programs, and substance use screenings supports participants’ physical health, which is vital for overall recovery.
- Fitness Programs: Partnerships with local gyms or fitness centers encourage participants to adopt healthier lifestyles, thereby improving physical and mental well-being.
8. Crisis Intervention Services
- Emergency Hotlines: Providing contact information for crisis hotlines ensures participants can receive immediate assistance in case of an emergency or relapse.
- On-Site Support Services: Collaborating with local professionals for on-site crisis intervention enhances support availability and reassures participants during critical moments.
9. Volunteer and Community Engagement Opportunities
- Community Service Projects: Engaging in volunteer opportunities helps participants build social connections, foster a sense of purpose, and strengthen their commitment to recovery.
- Social Activities: IOP-organized community events enable participants to practice social skills and build supportive relationships, reinforcing recovery in a real-world context.
Community resource strategies within Intensive Outpatient Programs provide vital support beyond clinical treatment. By connecting participants with local resources in areas such as employment, housing, wellness, and crisis management, IOPs enhance treatment outcomes, promote resilience, and empower participants to sustain their recovery journey long-term. These strategies create a strong community framework that complements therapy, fostering a robust support system for ongoing success in recovery.
Conclusion
Intensive Outpatient Programs (IOPs) serve as a valuable treatment option for individuals facing addiction, striking a balance between the structured support of inpatient care and the flexibility of traditional outpatient therapy. By providing comprehensive resources, IOPs empower participants to develop self-management skills, actively involve their families, and utilize community resources to foster a supportive recovery environment. Despite the advantages of flexibility and diverse treatment modalities, challenges such as potential inadequacies in crisis support and ethical dilemmas surrounding patient autonomy must be addressed. Ultimately, the effectiveness of IOPs lies in their ability to adapt to individual needs, helping participants navigate the complexities of recovery and achieve long-term sobriety and well-being.
Video: 5 CRUCIAL Benefits of Intensive Outpatient Programs for Addiction