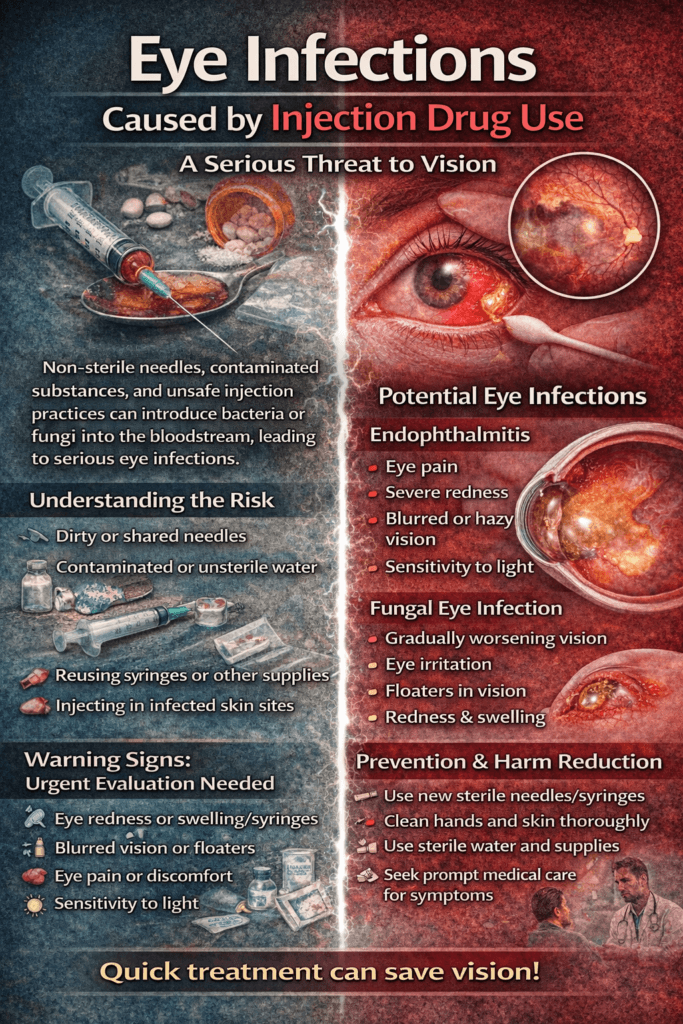
Eye infections caused by injection drug use are a serious yet often overlooked medical complication that can threaten vision and overall health. When non-sterile needles, contaminated substances, or unsafe injection practices introduce bacteria or fungi into the bloodstream, these microorganisms can travel to delicate eye structures, triggering infections such as endophthalmitis or retinal inflammation. Because early symptoms—like mild redness or blurred vision—may seem minor, individuals sometimes delay care, allowing infections to progress rapidly. Understanding how injection-related infections affect the eyes is essential for recognizing warning signs, seeking prompt treatment, and preventing permanent damage.
Illicit Injection Drug Use and Eye Infections: A Hidden Threat to Vision
Illicit injection drug use carries many well-known health dangers, but one of the lesser-recognized complications is the risk of serious eye infections that can threaten vision or even lead to permanent blindness. These infections often develop when bacteria or fungi enter the bloodstream through non-sterile needles, contaminated substances, or unsafe injection practices. Once pathogens circulate in the blood, they can travel to delicate structures of the eye, causing conditions that require urgent medical treatment.
One of the most severe complications is endophthalmitis, a rare but devastating infection inside the eye. This condition can occur when microorganisms spread hematogenously after injection drug use. Symptoms may include eye pain, blurred vision, light sensitivity, redness, or floaters. Without rapid treatment—often involving intravitreal antibiotics or antifungals—vision loss can occur within days. Because early symptoms may seem mild, individuals sometimes delay seeking care, which significantly worsens outcomes.
Another concern is fungal eye infection, especially from organisms such as Candida species that can enter the bloodstream through contaminated injection equipment. These infections may initially cause subtle visual disturbances but can progress to retinal damage. Injection drug use is also associated with septic emboli, where infected particles travel through blood vessels and lodge in retinal circulation, leading to inflammation, hemorrhage, or tissue damage.
Risk factors extend beyond needle sharing. Using non-sterile water, reusing syringes, injecting crushed pills, or injecting into infected skin sites all increase the likelihood of bloodstream infection. Coexisting conditions common among people who inject drugs—such as weakened immune systems, poor nutrition, or untreated systemic infections—further heighten susceptibility.
Prevention strategies focus on harm reduction and early medical care. Access to sterile injection supplies, education on safer practices, regular health screenings, and prompt treatment of systemic infections can reduce risk. Individuals who inject drugs should seek immediate medical evaluation if they experience any vision changes, eye pain, or redness, as early intervention dramatically improves the chance of preserving sight.
Ultimately, eye infections related to illicit injection drug use highlight how substance use can affect organs far beyond the injection site. Increasing awareness among healthcare providers, patients, and communities helps ensure earlier recognition, faster treatment, and better outcomes. Protecting vision is not only about eye care—it is about addressing systemic health, infection prevention, and compassionate access to addiction treatment and support.
Self-Management Strategies to Prevent Eye Infections From Injection Drug Use
Eye infections linked to injection drug use can develop quickly and lead to serious complications, including permanent vision loss. These infections often occur when bacteria or fungi enter the bloodstream through contaminated needles, unsafe preparation methods, or unclean injection practices and then travel to the eye. While treatment and recovery support are essential long-term solutions, self-management and harm-reduction strategies can significantly lower the immediate risk of infection and protect overall health.
One of the most important strategies is strict hygiene before injection. Washing hands thoroughly, cleaning the skin with alcohol swabs, and using sterile equipment each time reduces the risk of harmful microorganisms entering the bloodstream. Reusing or sharing needles dramatically increases infection risk, including infections that can spread to the eyes. Using new, sterile supplies whenever possible is one of the most effective preventive steps.
Safe preparation practices also matter. Using sterile water instead of tap water, avoiding saliva to dissolve substances, and preparing drugs on clean surfaces can reduce contamination. Many infections originate not from the substance itself but from bacteria introduced during preparation. Taking extra care during this stage can prevent systemic infections that may later affect vision.
Another key strategy is early symptom recognition. Individuals should monitor for warning signs such as eye redness, blurred vision, floaters, light sensitivity, swelling, or eye pain. Because bloodstream infections can quickly reach the eyes, any visual change should be treated as urgent. Seeking prompt medical care greatly increases the chance of preserving sight and preventing permanent damage.
General health maintenance also strengthens protection. Staying hydrated, maintaining a healthy diet, treating skin infections early, and managing chronic health conditions support immune function. A stronger immune system can better fight off bacteria or fungi before they spread to sensitive organs like the eyes.
Finally, connection to medical and harm-reduction services provides added protection. Clinics, syringe service programs, and outreach teams often offer sterile supplies, health screenings, wound care, and education about safer practices. These services are not about enabling drug use—they are about preventing life-threatening complications and creating pathways to treatment and recovery.
In summary, preventing eye infections related to injection drug use relies on practical daily actions: hygiene, sterile supplies, early symptom recognition, and access to supportive care. Even small protective steps can dramatically reduce infection risk and help safeguard vision. Empowering individuals with knowledge and realistic safety strategies supports both immediate health and long-term recovery possibilities.
Family Support Strategies to Help Prevent Eye Infections From Injection Drug Use
Injection drug use can lead to serious medical complications, including bloodstream infections that may spread to the eyes and threaten vision. These infections can develop when bacteria or fungi enter through non-sterile needles, contaminated preparation methods, or untreated skin wounds. While medical treatment and recovery services are critical, families play a powerful role in prevention. Supportive, informed family involvement can reduce infection risk, encourage safer behaviors, and help loved ones access timely care.
One of the most effective family strategies is nonjudgmental communication. Individuals who inject drugs often avoid discussing health concerns due to shame or fear of criticism. Families who approach conversations calmly and with empathy create a safe space for honesty. Phrases such as “I’m here to support you” or “I care about your health” can open dialogue and make it more likely the person will share symptoms early, including vision changes or signs of infection.
Families can also help by promoting harm-reduction awareness. Learning about sterile supplies, hygiene practices, and safer injection education allows relatives to share practical information without lecturing. When families understand that infection prevention strategies save lives—even if substance use has not stopped—they can reinforce safety rather than unintentionally increasing risk through stigma or confrontation.
Another important strategy is watching for early warning signs. Eye redness, swelling, sensitivity to light, blurred vision, or complaints of floaters may signal an infection that requires urgent care. Systemic symptoms such as fever, chills, or skin infections near injection sites can also indicate bacteria in the bloodstream that could spread to the eyes. Families who notice these signs can encourage immediate medical evaluation, which is often critical for preserving vision.
Supporting access to healthcare is equally protective. Offering transportation to appointments, helping schedule medical visits, or assisting with insurance or clinic navigation can remove barriers that delay treatment. Many people who inject drugs face logistical challenges, such as a lack of transportation or fear of judgment in healthcare settings. Family assistance can make care more accessible and less intimidating.
Finally, families should remember to care for themselves as well. Supporting someone with substance use challenges can be emotionally demanding. Seeking education, counseling, or peer support groups helps relatives stay informed, resilient, and effective in their role. When families maintain their own well-being, they are better equipped to provide steady, compassionate support.
In the end, preventing eye infections related to injection drug use is not solely a medical issue—it is also a relational one. Families who lead with empathy, awareness, and practical support can help reduce health risks, encourage early treatment, and strengthen the pathway toward recovery. Their presence can be a stabilizing force that protects both vision and overall health while reinforcing hope for long-term healing.
Community Resource Strategies to Prevent Eye Infections From Injection Drug Use
Eye infections caused by injection drug use are a serious but often overlooked public health concern. When non-sterile needles, contaminated solutions, or unsafe preparation practices introduce bacteria or fungi into the bloodstream, these microorganisms can travel to the eyes and cause severe infections that threaten vision. Because these complications develop systemically, prevention requires more than individual action—it depends heavily on accessible community resources, public health infrastructure, and supportive outreach systems.
One of the most effective strategies is expanding harm-reduction services. Community syringe service programs provide sterile needles, alcohol swabs, sterile water, and safe disposal options, all of which significantly reduce infection risk. These programs also offer wound care, infection screening, and education about safer injection practices. Studies consistently show that access to sterile equipment lowers bloodstream infection rates, which in turn decreases the risk of eye infections and other organ complications.
Accessible healthcare services are equally critical. Community clinics, mobile health units, and outreach teams help individuals receive early evaluation for symptoms such as redness, blurred vision, or eye pain. Early treatment is essential because infections that spread to the eye can progress rapidly and cause permanent damage if left untreated. Clinics that provide nonjudgmental care environments increase the likelihood that individuals will seek help early rather than delaying treatment due to stigma or fear.
Another vital strategy is community education initiatives. Public health campaigns, peer-led workshops, and outreach events can teach individuals about infection risks, early warning signs, and when to seek care. Education also includes training community members, shelter staff, and outreach workers to recognize the symptoms of systemic infection and respond appropriately. When communities are informed, they become proactive partners in prevention rather than passive observers.
Integrated support services further strengthen prevention efforts. Programs that combine addiction treatment referrals, mental health counseling, housing assistance, and medical care address the underlying conditions that increase infection risk. Stable housing, for example, allows individuals to maintain hygiene and store supplies safely, while mental health support can reduce risky behaviors associated with substance use.
Finally, community partnerships—between healthcare providers, nonprofits, public health agencies, and local organizations—create a coordinated safety net. Collaboration ensures that individuals have access to sterile supplies, medical care, education, and treatment pathways within a single connected system. This integrated approach reduces fragmentation and improves outcomes.
In summary, preventing eye infections related to injection drug use is not solely a medical challenge; it is a community responsibility. When communities invest in harm reduction, accessible healthcare, education, and integrated social services, they reduce infection risk, protect vision, and create opportunities for recovery. Strong community resources transform prevention from an individual burden into a shared public health effort that promotes safety, dignity, and long-term well-being.
Frequently Asked Questions
Here are some common questions:
1. How can injection drug use cause eye infections?
Bacteria or fungi can enter the bloodstream through non-sterile needles, contaminated drugs, or unsafe injection practices. Once in the bloodstream, these microorganisms can travel to the eye and infect internal structures, potentially causing serious complications.
2. What is the most serious eye infection linked to injection drug use?
One of the most severe is endophthalmitis, an infection inside the eye that can lead to rapid vision loss if not treated immediately. It is considered a medical emergency.
3. What symptoms should someone watch for?
Warning signs include eye redness, swelling, pain, blurred vision, floaters, discharge, or sensitivity to light. Any sudden change in vision should be treated as urgent.
4. How quickly can these infections develop?
Some infections can progress within hours to days. Because the eye is delicate and infections can spread rapidly, early medical care is critical to prevent permanent damage.
5. Are these infections treatable?
Yes. Many eye infections can be treated with antibiotics or antifungal medications, and sometimes injections directly into the eye. However, treatment is most effective when started early.
6. What increases the risk of infection?
Risk factors include sharing needles, reusing syringes, using non-sterile water, injecting crushed pills, poor skin hygiene, and injecting into infected or damaged skin.
7. Can someone lose vision permanently?
Unfortunately, yes. Severe infections can damage the retina or other eye structures, leading to partial or complete vision loss if treatment is delayed.
8. How can infections be prevented?
Using sterile injection supplies, cleaning the skin before injection, washing hands, avoiding shared equipment, and seeking medical care for wounds or illness can significantly reduce risk.
9. When should someone seek medical help?
Immediate medical attention is needed if there is eye pain, redness, swelling, or vision changes. Waiting can allow infection to spread and worsen outcomes.
10. Why is early treatment so important?
Early treatment can prevent infection from damaging delicate eye tissues. Prompt care greatly improves the chance of preserving vision and preventing complications.
Conclusion
Although eye infections linked to injection drug use can be severe, they are often preventable and treatable when addressed early. Harm-reduction practices, access to sterile supplies, timely medical evaluation, and supportive healthcare environments all play vital roles in reducing risk. Increased awareness among individuals, families, clinicians, and communities helps ensure symptoms are recognized quickly and treated effectively. By promoting education, compassionate care, and accessible health services, it is possible to protect vision, reduce complications, and support safer health outcomes for those at risk.
Video: