Injection drug use brings a wide range of health risks, and cancer is one you might not consider right away. While issues like infections and overdoses generally get more attention, cancer is also a significant concern for people who inject drugs. If you’re looking to track down exactly how injection drug use and cancer are tied together, this guide breaks it down so you can stay in the know or help someone you care about.
Understanding the Links Between Injection Drug Use and Cancer
People who inject drugs face some unique cancer risks because of what they inject, how it’s injected, and what these habits do to the body in the long run. Not everyone realizes that injecting drugs exposes the body to substances that can kick-start cancer or create other health issues that make it easier for cancer cells to form and thrive.
Hepatitis C and HIV often get the spotlight as major risks tied to injection drug use. Both raise your odds for cancer—hepatitis C is a leading cause of liver cancer after years of infection, while HIV weakens your immune system, opening the door for cancers that would be rare otherwise. Reusing needles, sharing shot equipment, and using unclean drugs or surfaces can bring on infections and put you in contact with cancer-linked substances.
The very stuff that’s injected—whether street drugs or substances used to stretch the supply—might include toxic fillers or chemicals with a track record for triggering cancer. Even the location where drugs are injected, if not sterile, can let harmful bacteria or viruses get in and stick around, adding another layer of risk. The whole situation is complicated, but let’s check out what that looks like, part by part.
How Cancer Develops in People Who Inject Drugs
Cancer begins when cells grow and divide uncontrollably. In the case of people who inject drugs, this can be set off in a few major ways:
- Infections: Bloodborne viruses and other germs enter your bloodstream through reused or dirty needles. Viruses like hepatitis B, hepatitis C, and HIV lead directly to cancers—including those of the liver, lymph nodes, or even the cervix.
- Chronic inflammation: Ongoing use can cause recurring inflammation, where you shoot up, which in turn can create the conditions needed for cancer to develop in the long run.
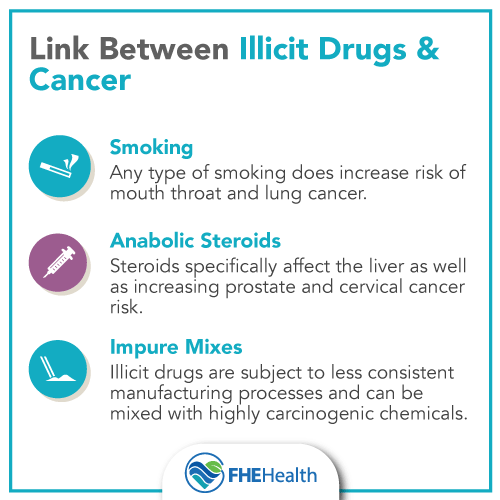
- Exposure to cancer-causing substances: Some illicit drugs, or the stuff mixed in with them, can mess with your DNA or your cells and start the process toward cancer.
- Lowered immune function: Drug use, particularly when infections set in, weakens your immune system, making it less effective at catching rogue cancer cells early or fighting infections that might let cancer grow unchecked.
This set of risks might not jump out at first, but these hidden triggers slowly build up in the background, increasing the chance for serious health scares in the future.
Common Cancers Linked to Injection Drug Use
Certain types of cancer are more likely among those who consistently inject drugs. Here’s what tends to pop up and why:
- Liver cancer: The big culprit here is long-term hepatitis B and C infection, which often happens because of shared needles. These viruses can quietly attack the liver for years, setting the stage for cancer way down the road.
- Lymphoma: Chronic HIV infection, far more likely in people who inject drugs, is strongly tied to certain lymphomas like non-Hodgkin lymphoma.
- Kaposi Sarcoma: This rare condition is tied to low immune function in HIV-positive folks, especially if the immune system has been badly weakened for a while.
- Cervical and anal cancers: HIV raises the risk here, and these can pop up in anyone exposed repeatedly. It’s also important to remember that virus-linked head and neck cancers show up more often in this group due to similar infections.
- Skin and soft tissue cancers: Whenever someone keeps injecting in the same area, wounds and sores can hang around, and in rare cases, they might turn cancerous if not properly taken care of.
Keep in mind that not every person who injects will get cancer. But anyone with untreated infections or ignored wounds sees a higher risk, particularly if they don’t keep up with routine healthcare visits or preventive steps.
Protecting Yourself: Reducing Cancer Risks with Safer Practices
Deciding to leave injection drug use behind is the safest route, but it’s understandable that this can be tough for many reasons. If stopping isn’t possible, here are steps you can take to make things safer and bring the risk down:
- Use only clean needles and gear. Look into local needle exchange services; these programs don’t just lower the odds for infection but also make it less likely you’ll come into contact with cancer-linked contaminants.
- Stay up to date on tests for hepatitis, HIV, and other transmitted infections. The sooner you know if something’s wrong, the quicker you can get ahead of bigger dangers—like cancer later on.
- Get vaccinated when you can. Vaccines for hepatitis B are widely available and drastically lower the risk.
- Don’t ignore wounds and sores. If an injection site remains red or swollen, or develops into an open sore, see a healthcare provider immediately. Quick fixes make a difference, and early action is best.
- Schedule regular health checkups. Even if you worry about being judged, more clinics are opening every year with harm reduction and no-judgment policies. Checkups help spot potential cancer warning signs before things get serious.
Making these steps part of your routine can help keep you safer, even if giving up drugs completely isn’t realistic right now.
Barriers That Make It Tougher to Spot and Treat Cancer Early
If you inject drugs, plenty of outside factors pile on and make it a challenge to catch cancer early or follow through with treatment. Stigma and fear, unstable living situations, and sometimes a lack of health insurance or negative experiences with healthcare push people away from the system. That means early cancer signs can get mistaken for side effects of drug use or missed entirely.
Getting to a provider you trust, or a supportive clinic, makes a huge difference. Where possible, build a relationship with a team that regularly works with people who use drugs—they can guide you on what to watch for and keep things welcoming and confidential.
Advanced Tips and Support Options
If you or someone you care about is interested in improving health options, here are some eye-catching tips and support avenues to check out:
- Join a support or harm reduction group. These groups don’t just tackle drug use; they offer solid advice for safe practices, help untangle the healthcare system, and share coping tricks for stress or cravings.
- Talk with a healthcare provider about screenings. If you’ve had infections or lasting sores, it’s smart to get advice about what screening for cancer makes sense.
- Explore medication-assisted treatment (MAT) if you’re thinking about cutting back or quitting. Medicines like methadone and buprenorphine, partnered with counseling, help manage cravings and make it easier to focus on overall wellness.
- Push for “one-stop shop” care programs. Integrated clinics can connect you with physical, mental, and substance use services under one roof—this is becoming a more popular model across healthcare systems.
Taking even small steps to connect with resources can pave the way to safer habits and better health outcomes.
Frequently Asked Questions
If you’re curious about how injection drug use and cancer overlap, you’re not alone. Here are some common questions, answered:
Question: Does every injection drug user develop cancer?
Answer: No. The risk depends on having certain long-lasting infections and on how often or long drugs have been injected, but many people never experience any cancer. Staying on top of regular checkups and screenings is key.
Question: Is hepatitis C treatable?
Answer: Yes. Almost all hepatitis C infections can now be cured with oral medication, bringing down liver cancer risks and also improving your overall health prospects.
Question: Can you reverse cancer risk if you stop injecting drugs?
Answer: Quitting improves your overall wellness, but if you already have certain viruses or long-term issues, some risk remains. Still, a healthier immune system and screening can catch problems earlier, making a big difference.
Wrapping up: What to Remember About Injection Drug Use and Cancer
The connection between cancer and injection drug use flies under the radar, yet it’s a real concern. Taking practical steps—like using sterile equipment, getting vaccines and tests, noticing changes early, and building ties with caring healthcare teams—can really lower your risks. The landscape for people who inject drugs is getting a bit more welcoming and supportive each year, with more resources designed to help without judgment. Don’t hesitate to ask for help or reach out for advice if you’re worried or need support. Even minor actions can set you on a path toward better, safer health.
Video: INJECTION DRUG USE AND CANCER