Overdose deaths among women have risen sharply, driven by factors like opioid use, mental health struggles, trauma, and stigma. In response, governments have expanded naloxone access, funded gender-focused treatment, and promoted trauma-informed care. Women can reduce risk through self-management strategies such as safe medication use and relapse prevention. Families support recovery by fostering open communication and learning overdose response skills, while communities offer women-centered recovery programs, shelters, harm reduction, and peer support. Together, these efforts aim to lower overdose risks and strengthen recovery for women.
Why Are Drug Overdoses Increasing Among Women? A Deep Dive into Biological, Social, and Systemic Drivers
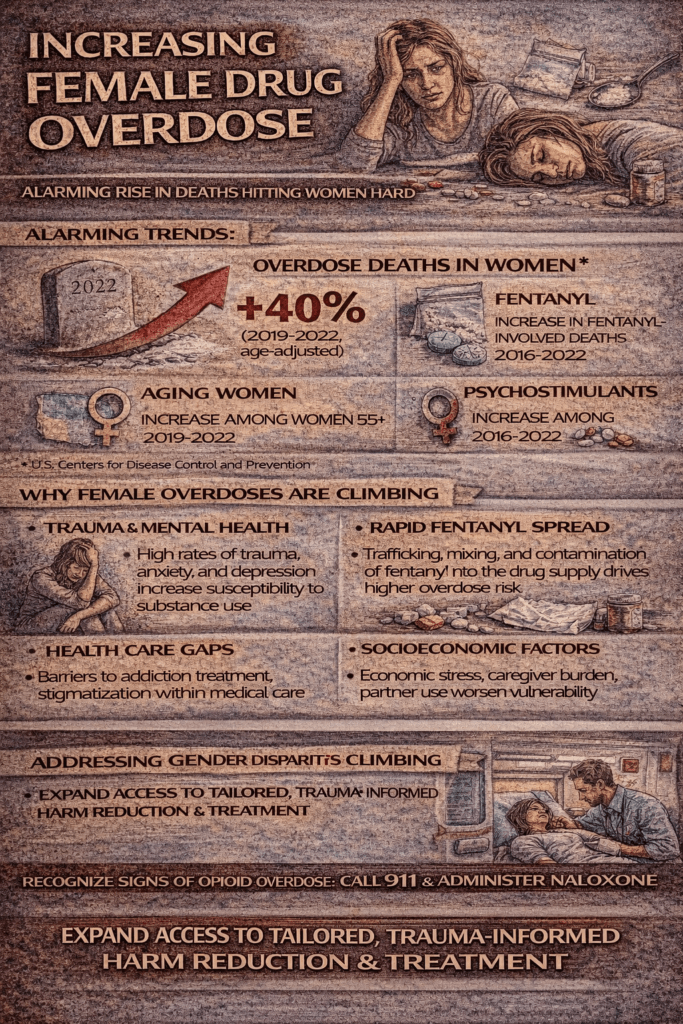
Over the past two decades, the United States has witnessed a troubling surge in overdose deaths among women. While the opioid epidemic often dominates headlines, this rise is not confined to opioids alone—it spans benzodiazepines, alcohol, and other substances. Understanding this crisis requires looking at overlapping biological, social, and systemic factors that place women at unique risk.
1. Biological Susceptibility and Faster Progression
Women often experience the “telescoping effect”—progressing more quickly than men from first use to addiction, and from addiction to health complications. Differences in metabolism play a key role: women have higher body fat, less body water, and lower levels of gastric alcohol dehydrogenase, all of which intensify toxic effects. These physiological factors make even moderate use riskier.
2. Prescription Practices and Health System Dynamics
Women are more likely than men to be prescribed medications for chronic pain, anxiety, and insomnia. Higher healthcare utilization means more exposure to opioids, benzodiazepines, and antidepressants. Between 1999 and 2016, prescription opioid overdose deaths among women rose nearly 600%, compared to just over 300% among men. Additionally, women are more frequently prescribed multiple medications at once—a dangerous combination that elevates overdose risk.
3. Gender-Based Social and Economic Factors
Mental health burdens, including anxiety, depression, and trauma, often drive women toward substance use as a coping strategy. Adverse childhood experiences and intimate partner violence also play a role. On top of this, stigma and logistical barriers—such as childcare responsibilities, poverty, or fear of judgment—make it harder for women to seek treatment, leaving them more vulnerable.
4. Shifts in Illicit Drug Use
The drug supply itself has changed. Synthetic opioids like fentanyl, often mixed with heroin or counterfeit pills, are driving overdose deaths in women aged 30–64. Rates in this group rose by more than 260% between 1999 and 2017. Women are also more likely to engage in polysubstance use—mixing tranquilizers, sedatives, or alcohol—which compounds overdose risk.
5. Pregnancy and Postpartum Vulnerabilities
Overdose is now a leading cause of maternal mortality in the U.S. Among women ages 35–44, overdose deaths more than tripled between 2018 and 2021. Fear of custody loss, criminalization, and stigma keeps many pregnant and postpartum women from seeking care, despite increased vulnerability during these life stages.
6. COVID-19 and Broader Stressors
The pandemic magnified existing risks. Social isolation, economic hardship, and reduced access to healthcare and harm reduction programs hit women particularly hard. Marginalized groups—including sex workers and women with unstable housing—faced even greater risks when services closed or scaled back.
7. Alcohol’s Rising Toll
Beyond illicit drugs, alcohol-related deaths among women nearly tripled from 1999 to 2020. Physiological differences make women more vulnerable to liver disease, heart complications, and cancer at lower consumption levels. Cultural trends, including “wine culture” and targeted marketing, have normalized heavier drinking among women, particularly between the ages of 20 and 55.
Summary Table
| Rising deaths, cultural normalization, and marketing | Key Contributors |
|---|---|
| Biological | Faster addiction progression; metabolism differences |
| Healthcare | Higher prescribing rates; multiple medications |
| Social & Economic | Trauma, mental health, stigma, childcare barriers |
| Illicit Drugs | Fentanyl surge; polysubstance use |
| Maternal Health | Overdose risk in pregnancy/postpartum; treatment stigma |
| Pandemic Effects | Isolation, stress, disrupted supports |
| Alcohol Trends | Rising deaths, cultural normalization, marketing |
Key Takeaways
The rise in female overdose deaths is not the result of a single factor but a convergence of biological vulnerability, prescribing practices, trauma, stigma, shifting drug trends, and systemic barriers.
To reverse this trend, public health efforts must prioritize gender-responsive care:
- Better prescribing practices and safer pain management alternatives
- Expanded access to gender-specific addiction treatment programs
- Routine screening and supportive, non-punitive maternal healthcare
- Widespread naloxone distribution and education
- Policies that reduce stigma and increase accessibility for women juggling childcare and economic instability
This surge represents more than a statistical shift—it’s a public health crisis rooted in inequities. Addressing it requires coordinated action that acknowledges women’s unique biological, social, and systemic challenges.
How U.S. Government Policies Are Reducing Overdose Deaths—With Key Benefits for Women
The U.S. government, along with states and localities, has ramped up efforts to address the overdose crisis. While most initiatives are gender-neutral, many have had significant impacts on women, especially in maternal health, harm reduction, and access to life-saving medications like naloxone. Below is a breakdown of the major strategies shaping this response.
1. Expanding Access to Naloxone
One of the most visible steps has been making naloxone—the opioid overdose reversal drug—widely available.
- Over-the-counter approval: In March 2023, the FDA approved naloxone nasal spray (Narcan) for OTC purchase, enabling broader access without a prescription.
- Federal support: The Biden-Harris administration boosted State Opioid Response grants, distributing nearly 10 million naloxone kits and preventing more than 600,000 overdoses. Naloxone is now stocked in schools, federal facilities, and public housing.
- State and local impacts: Michigan’s statewide naloxone program led to a 25% drop in overdose deaths, while Indiana saw an 18% reduction after combining naloxone expansion with treatment programs. In Houston/Harris County, a comprehensive approach—including naloxone—helped drive one of the steepest local declines in overdose deaths.
For women, greater naloxone access is particularly critical during pregnancy and postpartum, when overdose is a leading cause of maternal death.
2. Harm Reduction and Real-Time Surveillance
Harm reduction policies have broadened safer use options and enhanced overdose prevention.
- Syringe services programs (SSPs): Now authorized in 41 states and D.C., these programs reduce the spread of infectious diseases, connect women to treatment, and provide naloxone.
- Fentanyl test strips: Federal funding allows community groups to distribute strips, giving users—especially women more likely to use prescription pills—an early warning about contaminated drugs.
- Overdose Data to Action (OD2A): A CDC program that funds states like Rhode Island and Illinois to collect real-time overdose data and deploy rapid, targeted interventions.
3. Continuity of Care and Treatment Access
Expanding treatment has been another major focus.
- Opioid Rapid Response Program (ORRP): Ensures care continuity when prescribers close unexpectedly, preventing treatment gaps that can lead to relapse or overdose.
- Medication-Assisted Treatment (MAT): Federal guidelines now make it easier for physicians and pharmacies to prescribe buprenorphine, a proven treatment for opioid use disorder.
- Maternal Opioid Misuse (MOM) Model: Integrates maternity care and substance-use treatment, addressing the unique risks faced by pregnant and postpartum women.
4. National Strategy, Public Awareness, and Advocacy
The White House has coordinated multi-sector responses, combining prevention, education, and community engagement.
- Real Deal on Fentanyl: A campaign targeting youth awareness of fentanyl risks.
- CDC Rx Awareness Campaign: Shares personal stories of women impacted by opioids to reduce stigma and encourage treatment-seeking.
- Community partnerships: The White House Challenge to Save Lives from Overdose brings local organizations together to scale up prevention and outreach efforts.
5. Settlement Funds and Local Deployment
Opioid lawsuit settlements are channeling nearly $50 billion to states and local governments. Yet the impact depends on how funds are spent. Communities that prioritize harm reduction, treatment, and the voices of people with lived experience—rather than solely policing—see more meaningful results, including improved support for women and mothers in recovery.
Summary: What the Government Is Doing to Help Women
| Gender-responsive pathways, such as the MOM model and expanded buprenorphine access. | Impact on Women |
|---|---|
| Naloxone Expansion | Greater survival chances during overdose events, especially critical for maternal health. |
| Harm Reduction | Safer use environments, fentanyl warnings, and easier entry points to treatment. |
| Treatment Access | Gender-responsive pathways like the MOM model and expanded buprenorphine access. |
| Data & Community Action | Tailored interventions where overdose risk is highest. |
| Awareness Campaigns | Stigma reduction and improved education for women seeking care. |
| Settlement Funding Oversight | Ensures money supports harm reduction and recovery programs that directly help women. |
Closing Note
While most overdose prevention policies are not explicitly designed for women, their benefits are substantial. Initiatives like naloxone expansion, syringe services, and the MOM model help address unique female vulnerabilities—including maternal overdose risks, stigma, and treatment barriers. Sustaining and expanding these efforts will be critical to turning the tide of overdose deaths for women and communities nationwide.
Self-Management Strategies to Prevent Overdoses Among Women: Practical, Gender-Responsive Approaches
Overdose prevention is often discussed in clinical or policy terms, but self-management plays a vital role—especially for women. Women face unique biological, psychological, and social risks that influence how substances affect them, how they cope with stress, and how they access care. While self-management is not a substitute for professional treatment or emergency response, it can reduce risks, build resilience, and empower women to protect themselves and their communities.
1. Substance Safety & Harm Reduction
- Avoid using alone: Overdoses are far more fatal when no one is present. Use with someone trusted or consider remote monitoring services like the Never Use Alone hotline.
- Test substances: Women are increasingly affected by fentanyl contamination in non-opioid drugs (such as cocaine or counterfeit pills). Fentanyl test strips offer a critical line of defense.
- Start low, go slow: Whether taking prescriptions or illicit substances, beginning with the smallest possible dose lowers the risk of accidental overdose.
- Avoid mixing: Combining opioids, alcohol, benzodiazepines, or sedatives magnifies overdose danger.
- Carry naloxone: Learn how to use naloxone (Narcan) and teach family or friends. Many states now provide it free or over the counter.
2. Mental Health & Emotional Resilience
- Build coping strategies: Replace self-medication with healthier outlets such as journaling, mindfulness, exercise, or creative activities.
- Recognize trauma triggers: Women with histories of trauma are more likely to use substances as coping tools. Identifying triggers early helps reduce relapse and risky use.
- Seek peer support: Online and in-person women’s recovery groups provide stigma-free spaces to share experiences and access encouragement.
3. Physical Health & Medication Awareness
- Track prescriptions: Logging medications reduces the chance of double-dosing or dangerous interactions.
- Communicate with doctors: Be transparent about prescriptions, supplements, and alcohol use so providers can spot risks.
- Know biological differences: Women metabolize alcohol and drugs differently, meaning smaller amounts can cause stronger and more toxic effects.
4. Social & Family Safety Nets
- Create an overdose safety plan: Identify emergency contacts, naloxone sources, and crisis steps.
- Address childcare needs: For mothers, planning safe childcare during stressful times reduces the risk of using in isolation.
- Find accountability partners: Trusted friends or family who check in regularly can spot warning signs early.
5. Lifestyle & Stress Management
- Maintain daily routines: Adequate sleep, hydration, and balanced nutrition stabilize mood and reduce cravings.
- Practice stress reduction: Tools like yoga, meditation, or even short daily walks can improve emotional resilience.
- Limit alcohol and stimulants: Since alcohol-related deaths among women are rising quickly, moderation and self-monitoring can be lifesaving.
6. Reproductive & Maternal Considerations
- Pregnancy and postpartum vigilance: Overdose risk peaks during these stages. Women should seek specialized maternal substance use programs when struggling.
- Avoid isolation: Stigma often prevents mothers from seeking help. Women-centered groups offer safe connections and reduce hidden risks.
7. Education & Community Empowerment
- Stay informed: Local harm reduction networks share drug supply alerts, including fentanyl spikes.
- Normalize overdose conversations: Discussing overdose risks with partners, family, and even children (in age-appropriate ways) builds protective networks.
- Advocate for resources: Women involved in advocacy—such as naloxone distribution or community education—often find empowerment in helping others.
Key Takeaway
Preventing overdoses among women requires a holistic approach. Practical harm reduction strategies (like naloxone use and safer consumption), emotional resilience (mental health support and peer networks), and attention to unique vulnerabilities (trauma, maternal health, and polysubstance risks) work together to protect lives. By tailoring self-management strategies to women’s realities, individuals and communities can take meaningful steps toward safety and recovery.
How Families Can Help Prevent Overdoses Among Women: Support Strategies That Save Lives
When it comes to preventing overdoses among women, families play a powerful role. Women often face unique challenges—including trauma, stigma, and caregiving responsibilities—that make overdose risks higher. Supportive family environments can reduce these risks by fostering trust, strengthening resilience, and ensuring safety. Below are practical family strategies to help protect women and promote recovery.
1. Open Communication & Emotional Support
- Listen without judgment: Create a safe space for women to share struggles with stress, trauma, or substance use. Avoid shaming language, which often drives secrecy.
- Check in regularly: Even brief daily conversations can uncover warning signs before a crisis.
- Normalize mental health care: Encourage therapy or counseling as part of family wellness, not just an individual burden.
2. Education & Overdose Preparedness
- Learn the signs of overdose: Slow or irregular breathing, pinpoint pupils, and unresponsiveness are urgent red flags.
- Keep naloxone at home: All family members should know how to use it and keep it within reach.
- Know emergency steps: Call 911 immediately, administer naloxone if available, and stay until medical help arrives.
3. Reducing Stigma & Isolation
- Avoid blame: Shaming women for substance use increases secrecy and risk.
- Promote belonging: Invite women into family routines and events, even if they are struggling.
- Encourage peer support: Connect them to women-centered recovery or harm reduction groups where stigma is lower.
4. Practical Daily Support
- Assist with childcare or household duties: Relieving these stressors reduces the likelihood of turning to substances for relief.
- Provide safe transportation: Offer rides to treatment, counseling, or recovery meetings.
- Create structured routines: Consistency in meals, sleep, and schedules fosters stability and lowers the risk of relapse.
5. Crisis & Safety Planning
- Develop a family safety plan: Decide who will call 911, who will administer naloxone, and who will care for children during emergencies.
- Identify triggers together: Work as a family to avoid high-risk environments or stressful dynamics.
- Build a trusted support network: Involve extended relatives, close friends, or community allies to ensure no one faces crises alone.
6. Long-Term Empowerment
- Support recovery goals: Celebrate progress, no matter how small, to reinforce motivation.
- Encourage healthy coping strategies: Promote exercise, hobbies, mindfulness, or spiritual practices as alternatives to substance use.
- Advocate together: Families who participate in awareness campaigns or local support groups not only reduce stigma but also strengthen their own bonds.
Key Takeaway
Families are a frontline defense against overdose. By combining compassion, education, overdose preparedness, and practical support, families can help women feel safer, reduce isolation, and foster healthier choices. Strong family networks are not just sources of love—they are protective factors that save lives.
Community Resources That Help Prevent Overdose Among Women
Women face unique challenges when it comes to overdose risk—balancing childcare, navigating trauma, and facing stigma often make treatment harder to access. While self-management and family support are important, community resources provide a critical layer of protection. By reducing barriers, creating safer environments, and addressing women’s social realities, communities can save lives.
1. Accessible Healthcare & Harm Reduction Services
- Women-focused clinics: Offer gender-responsive care, including childcare and reproductive health support.
- Syringe Services Programs (SSPs): Provide sterile supplies, naloxone, and links to care.
- Mobile outreach vans: Deliver naloxone, test strips, and wound care directly to neighborhoods.
2. Overdose Education & Naloxone Distribution
- Community trainings: Teach overdose recognition and naloxone use.
- Naloxone in public spaces: Distribute free kits through pharmacies, libraries, and women’s centers.
- Awareness campaigns: Share women’s stories to reduce stigma and encourage help-seeking.
3. Integrated Mental Health & Trauma Support
- Domestic violence shelters: Pair safety with substance use and trauma services.
- Peer recovery specialists: Women with lived experience guiding others toward recovery.
- Community mental health groups: Safe spaces to process anxiety, depression, and trauma.
4. Social & Economic Supports
- Childcare and housing assistance: Address two of the biggest barriers to recovery.
- Job training programs: Build long-term stability and independence.
- Transportation vouchers: Ensure women can reach treatment and recovery services.
5. Partnerships & Community Mobilization
- Faith-based organizations: Offer support circles and recovery events.
- Schools & colleges: Provide gender-aware prevention education.
- Cross-sector collaboration: Public health, law enforcement, and advocacy groups aligning around harm reduction.
6. Maternal & Postpartum Focused Resources
- Pregnancy & postpartum treatment programs: Integrate prenatal care with addiction support.
- Mother-and-child housing: Allow mothers to access treatment without fear of losing custody.
Key Takeaway:
Community-based strategies are most effective when they are holistic and gender-responsive. By addressing both medical risks (like fentanyl contamination) and social realities (trauma, stigma, childcare, and poverty), communities can play a decisive role in preventing overdose deaths among women.
Frequently Asked Questions
Here are some common questions:
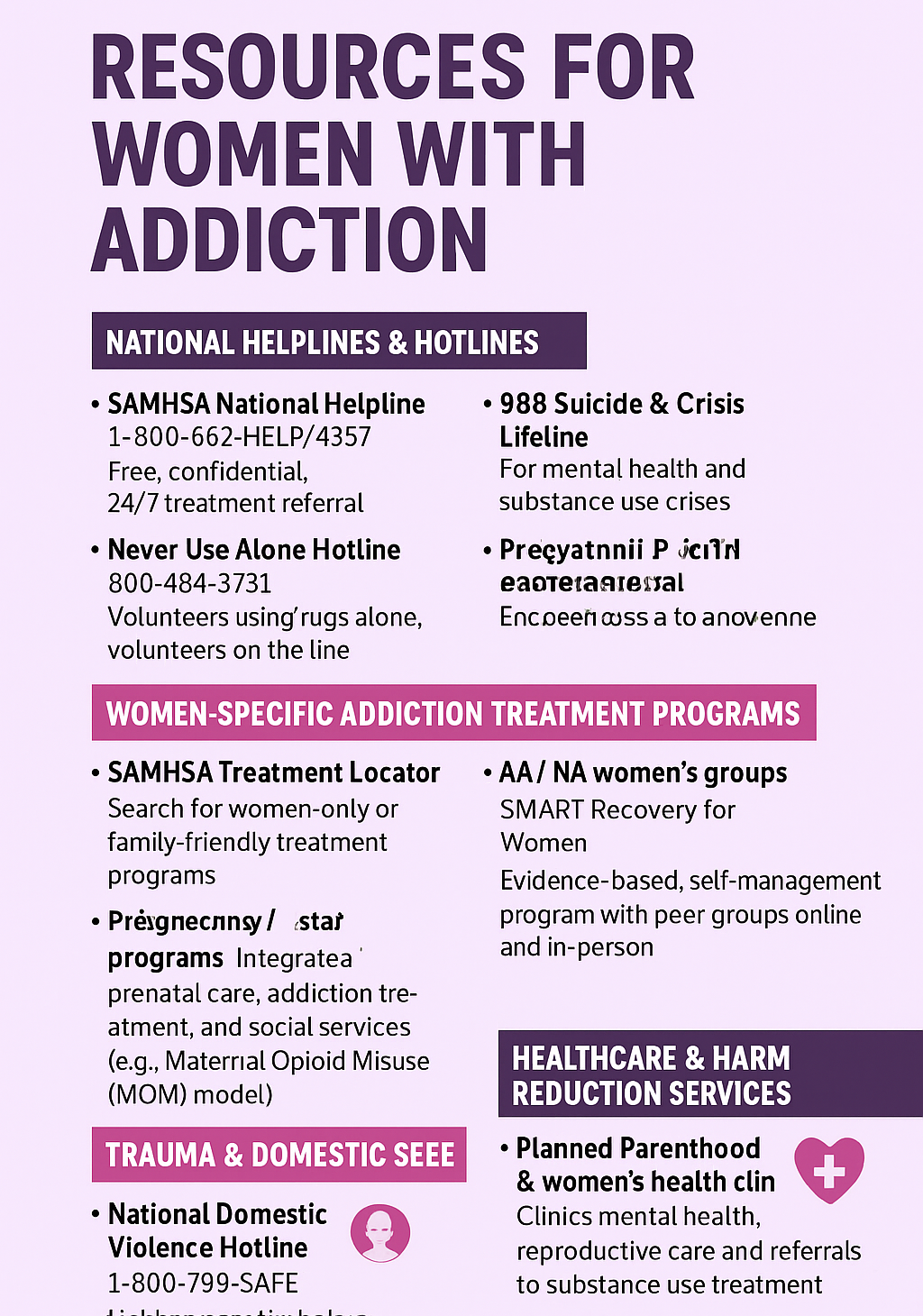
Question: What resources are available for women with addiction?
Answer: Women with addiction often face unique barriers—like childcare responsibilities, stigma, histories of trauma, or fear of losing custody—that make traditional services harder to access. Fortunately, there are many resources specifically designed for women, ranging from national hotlines to gender-responsive treatment programs.
Here’s a structured overview:
🔹 1. National Helplines & Hotlines
- SAMHSA National Helpline (1-800-662-HELP / 4357)
- Free, confidential, 24/7 treatment referral and information.
- Can connect women to local programs that accept Medicaid, uninsured patients, or sliding scale.
- 988 Suicide & Crisis Lifeline
- For mental health and substance use crises.
- Never Use Alone Hotline (800-484-3731)
- For individuals using drugs alone, volunteers stay on the line and call EMS if needed.
🔹 2. Women-Specific Addiction Treatment Programs
- Substance Abuse and Mental Health Services Administration (SAMHSA) Treatment Locator
- Search for programs with women-only or family-friendly treatment.
- Residential programs for women and mothers
- Many states fund treatment centers that allow women to bring their children with them (reducing custody fears).
- Pregnancy/Postpartum programs
- Specialized programs integrate prenatal care, addiction treatment, and social services (e.g., the Maternal Opioid Misuse [MOM] model).
🔹 3. Peer & Community Support
- Women for Sobriety (WFS)
- Peer support program designed by and for women, focusing on self-empowerment.
- AA / NA women’s groups
- Many communities offer women-only meetings to reduce stigma and increase comfort.
- SMART Recovery for Women
- Evidence-based, self-management program with peer groups online and in-person.
🔹 4. Trauma & Domestic Violence Resources
- National Domestic Violence Hotline (1-800-799-SAFE)
- Links women to shelters and trauma-informed services that often integrate addiction care.
- Rape, Abuse & Incest National Network (RAINN) (1-800-656-HOPE)
- For women whose substance use is connected to sexual assault or trauma.
🔹 5. Healthcare & Harm Reduction Services
- Planned Parenthood & women’s health clinics
- Offer mental health, reproductive care, and referrals to substance use treatment.
- Harm reduction programs
- Syringe exchange, naloxone distribution, and fentanyl test strips.
- Many have women-focused outreach (e.g., services for pregnant women, sex workers, or homeless women).
🔹 6. Social Support Resources
- Housing assistance (e.g., Oxford House for Women, recovery housing programs that allow children).
- Childcare services during treatment (offered in some state-funded women’s rehab programs).
- Job training & workforce programs for women in recovery, to reduce economic instability.
🔹 7. Online & Virtual Resources
- In the Rooms (free virtual support groups, many women-only).
- SheRecovers Foundation (women’s recovery network offering online meetings and retreats).
- Facebook/Reddit recovery communities (e.g., r/stopdrinking, women’s recovery groups).
✨ Key Takeaway:
Resources for women with addiction exist at multiple levels—from national hotlines and harm reduction services to women-only peer groups and maternal programs. The most effective supports are gender-responsive, addressing childcare, trauma, and stigma alongside treatment.
Question: What are some examples of social situations that would make women with addiction overdose more often?
Answer: Social situations and contexts that increase vulnerability for women. Research shows women face unique pressures and risks that can make overdoses more likely. Here are some examples of social situations:
🔹 1. Relationship Dynamics & Intimate Partner Violence
- Using drugs with a controlling or abusive partner who encourages higher doses.
- Partners are pressuring women into injecting drugs or combining substances.
- Fear of calling 911 during an overdose due to partner threats, legal fears, or custody issues.
🔹 2. Motherhood & Family Stressors
- Women use alone in secret due to stigma about being a mother with addiction.
- Fear of child protective services intervention leading to hidden or rushed use.
- Overdose risk postpartum, when relapse risk is especially high.
🔹 3. Stigma & Social Isolation
- Using drugs in isolation to avoid judgment, which increases fatal overdose risk (no one to administer naloxone).
- Double stigma (being a woman + being a person who uses drugs), reducing willingness to seek help.
🔹 4. Economic & Survival Pressures
- Trading sex for drugs or money leads to unsafe environments with high overdose risk.
- Homelessness or unstable housing, where women may be in unsafe or rushed conditions.
- Working in informal/unstable jobs with high stress and little support.
🔹 5. Peer Group & Social Use Situations
- Being introduced to new or stronger substances by peers or partners (e.g., fentanyl-laced drugs).
- Sharing drugs or syringes in group settings without knowing the potency.
- Social pressure to “keep up” with others’ tolerance levels.
🔹 6. Mental Health & Trauma Contexts
- Self-medicating after traumatic experiences (e.g., domestic violence, sexual assault).
- Using substances during depressive or anxious episodes without support.
- Higher risk of polysubstance use (mixing opioids, alcohol, benzodiazepines) to cope with trauma.
✨ In short: Women often overdose more in situations shaped by relationships, stigma, childcare fears, trauma, and economic survival pressures. Unlike men, their overdose risk is often tied to hidden or socially constrained drug use rather than open social use.
Question: Create a scenario-based guide (like role-play situations) that families or providers could use to spot these high-risk contexts for women before they escalate to overdoses?
Answer: High-Risk Situations for Women & Overdose: A Role-Play Guide
Scenario 1: Using Secrecy as a Mother
- Context: Maria, a single mother, hides her drug use because she fears Child Protective Services (CPS) will take her kids. She uses it alone at night after her children are asleep.
- Risk: No one is present to administer naloxone or call for help if she overdoses.
- Family Response Strategy:
- Create a safety plan with trusted family/friends who can check in.
- Reassure her that support ≠ judgment; encourage open communication.
- Provide naloxone training for supportive relatives.
Scenario 2: Intimate Partner Pressure
- Context: Jasmine’s boyfriend injects her with drugs, often mixing substances. He discourages her from seeking treatment and threatens her if she refuses.
- Risk: Coerced use, polysubstance overdose, fear of calling 911 during emergencies.
- Family/Provider Response Strategy:
- Screen for domestic violence and link to women’s shelters.
- Provide harm reduction tools (naloxone, fentanyl test strips).
- Empower her to access confidential women-only recovery programs.
Scenario 3: Social Pressure in Peer Settings
- Context: Leah, who has a lower tolerance, uses at a party with friends who are used to high-potency fentanyl pills. She feels pressured to match their use.
- Risk: Accidental overdose from taking more than her body can handle.
- Family/Community Response Strategy:
- Teach women to test substances (fentanyl test strips).
- Normalize setting boundaries and refusing unsafe use.
- Connect with peer recovery groups that reinforce safer norms.
Scenario 4: Trauma-Triggered Use
- Context: After a sexual assault, Tasha relapses and mixes opioids with benzodiazepines to numb pain. She isolates herself from her family.
- Risk: High risk of fatal overdose due to polysubstance use + secrecy.
- Family/Provider Response Strategy:
- Encourage trauma-informed therapy resources (e.g., RAINN).
- Normalize mental health support alongside recovery.
- Provide crisis numbers (988, domestic violence hotlines).
Scenario 5: Economic & Survival Pressures
- Context: Danielle, experiencing homelessness, exchanges sex for drugs. She often uses in unfamiliar, unsafe spaces with strangers.
- Risk: Increased likelihood of exposure to adulterated drugs and unsafe overdose environments.
- Family/Community Response Strategy:
- Link to housing-first programs and women’s shelters.
- Encourage harm reduction practices (don’t use alone, naloxone kits).
- Connect with outreach programs that provide safer spaces for women.
✨ Key Takeaway:
Overdose prevention for women requires understanding the social context—hidden use, relationship pressures, trauma, and survival needs. Families and providers can intervene by offering nonjudgmental support, safety planning, harm reduction tools, and gender-specific resources.
Conclusion
The rising rates of overdoses among women with addiction highlight a critical public health concern that demands comprehensive attention. Data indicate that women are increasingly affected by both prescription and illicit substances, often facing unique physiological, social, and psychological risk factors. Government interventions, including expanded access to treatment programs and harm reduction services, play a key role in addressing this crisis. Alongside these efforts, self-management strategies—such as developing coping skills, recognizing triggers, and practicing safe medication use—empower women to reduce personal risk. Family support and community resources further strengthen protective networks, offering emotional guidance, peer support, and connections to treatment services. Together, these strategies form a multi-layered approach that can help mitigate overdose risks and promote recovery among women struggling with addiction.
Video: The SHOCKING Truth About Women’s Drug Overdose Rates
What’s REALLY Holding Women Back in Recovery?
Expert Warns: Women’s Addiction Treatment Barriers Can Be DEADLY