Addiction treatment during hospitalization provides critical care to stabilize individuals and prepare them for long-term recovery. It aims to prevent readmissions by equipping patients with coping skills, relapse prevention strategies, and aftercare plans. While it offers benefits such as immediate medical attention, challenges such as limited follow-up, cost, and dependence on institutional care remain. Ethical dilemmas around patient autonomy and treatment coercion also arise. Self-management, family support, and community resources play key roles in maintaining recovery after discharge, offering ongoing support to reduce relapse and prevent readmission.
The Role Benefits of Hospital-Based Addiction Treatment in Preventing Readmissions for Long-Term Recovery
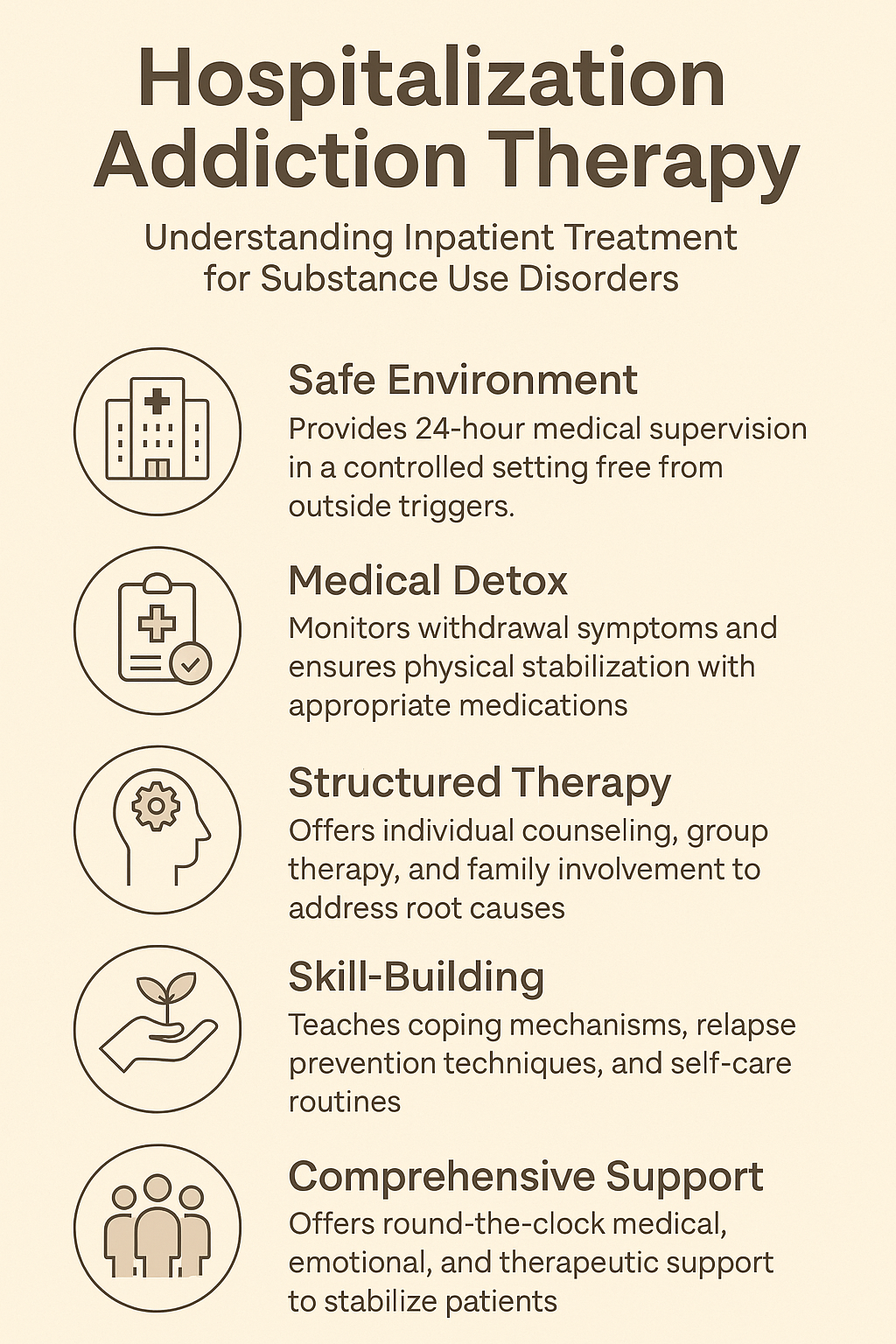
Addiction treatment during hospitalization can play a significant role in preventing readmissions, but its effectiveness depends on several factors, including the quality of treatment, aftercare planning, and the patient’s commitment to recovery. Here’s how therapy during hospitalization can help reduce the likelihood of readmissions: it plays a crucial role in supporting long-term recovery and reducing the possibility of relapse. Here are some key advantages:
1. Medically Supervised Detoxification and Stabilization
Advantage: Hospitalization provides a safe and controlled environment for detoxifying from substances, under the supervision of medical professionals using comprehensive detoxification and medical stabilization.
Role: During hospitalization, individuals with addiction can receive medically supervised detoxification and stabilization, which can help reduce immediate physical health risks and withdrawal symptoms.
Prevention of Readmissions: Proper stabilization helps prevent relapse due to unmanaged withdrawal symptoms or medical complications, providing a solid foundation for long-term recovery.
Benefit: Detoxification helps manage withdrawal symptoms and reduces the physical risk of complications, providing a stable foundation for ongoing recovery and preventing immediate relapse or medical emergencies that could lead to readmission.
2. Addressing Co-Occurring Mental Health Issues
Advantage: Many people use integrated mental health care.
Role: Many individuals with addiction also experience co-occurring mental health disorders. Hospitalization provides an opportunity to address both the addiction and any underlying psychological issues, such as depression or anxiety, and mental health disorders, such as anxiety, depression, or PTSD. Inpatient treatment allows for the simultaneous treatment of both addiction and mental health conditions.
Prevention of Readmissions: Treating both addiction and mental health issues simultaneously can reduce the likelihood of future relapse and readmission, as clients gain tools to manage both conditions.
Benefit: Treating co-occurring disorders reduces the likelihood of relapse and readmission by addressing the root causes of addiction, rather than just the symptoms, and helping patients develop coping strategies for managing both conditions.
3. Individualized Treatment Plans
Role: Inpatient treatment allows healthcare providers to develop tailored, individualized treatment plans that consider the patient’s unique needs, substance use history, and comorbid conditions.
Advantage: During hospitalization, addiction treatment can be tailored to the individual’s specific needs, taking into account their history, triggers, and underlying issues.
Prevention of Readmissions: Personalized plans decrease the likelihood of a relapse.
Benefit: Personalized treatment increases the effectiveness of the therapy, helping patients focus on the areas where they need the most support, and improving the chances of successful recovery and reducing the risk of readmission, as they address the specific challenges the individual faces.
4. Comprehensive Support and Education
Advantage: Hospitalized patients often receive addiction education, therapy, life skills training, support groups, and patient education and skill-building.
Role: Hospitals often provide addiction education and life skills training, helping patients understand the nature of addiction, triggers, coping mechanisms, and relapse prevention strategies.
Prevention of Readmissions: Equipping patients with the knowledge and skills to navigate life after discharge can reduce the likelihood of relapse.
Benefit: These resources equip patients with the knowledge, tools, and coping mechanisms needed to navigate their recovery after leaving the hospital, reducing the likelihood of relapse and readmission.
5. Structured Environment with Fewer Triggers
Advantage: Inpatient treatment provides a structured environment free from the everyday triggers and stressors that might encourage substance use, aftercare planning, and support.
Role: A key component of addiction treatment during hospitalization is the development of a comprehensive aftercare plan, which may include outpatient therapy, community support groups, and sober living arrangements.
Prevention of Readmissions: Strong aftercare support reduces the risk of relapse by ensuring patients have ongoing resources and guidance after leaving the hospital.
Benefit: A safe, supportive environment during treatment can help patients focus on recovery without external pressures, reducing the risk of relapse once they return to the outside world.
6. Aftercare Planning and Continuity of Care
Advantage: Hospitalization often includes the development of an aftercare plan, which may involve outpatient therapy, support groups, and follow-up care, and using relapse prevention strategies
Role: Inpatient treatment often focuses on relapse prevention, teaching patients strategies to recognize early signs of relapse, cope with cravings, and make healthier decisions.
Prevention of Readmissions: This proactive approach can help individuals avoid situations that might lead to relapse, decreasing the likelihood of readmission to the hospital for addiction-related reasons.
Benefit: This continuity of care ensures that patients have a clear path for ongoing recovery after discharge, with access to support and resources that reduce the likelihood of relapse and readmission.
7. Family and Social Support Involvement
Advantage: Support Systems and Family Involvement
Role: Many inpatient programs involve family members in the treatment process, strengthening the patient’s support system and therapy, and educating and involving loved ones in the recovery process.
Prevention of Readmissions: Family support is crucial in maintaining long-term recovery, and involving loved ones during hospitalization can provide a solid foundation for continued success after discharge.
Benefit: Strong family and social support post-discharge plays a crucial role in preventing relapse, and having this support during hospitalization helps strengthen the patient’s recovery network, leading to more sustained success and fewer readmissions.
8. Relapse Prevention Strategies
Advantage: While addiction treatment during hospitalization can significantly reduce the risk of readmission, it is not a cure-all. Success depends on comprehensive treatment, effective aftercare, and the patient’s ongoing commitment to recovery. A holistic approach that addresses both the medical and psychological aspects of addiction, along with strong post-discharge support, can help minimize the chances of readmission and promote lasting recovery. Often, it includes specific training on relapse prevention, teaching patients how to recognize early warning signs, handle cravings, and avoid high-risk situations.
Benefit: By learning to manage triggers and cope with stress in healthy ways, patients are better prepared to face life after treatment, significantly lowering the risk of readmission.
9. Holistic Care Approach
Advantage: Hospital-based addiction treatment often adopts a holistic approach, addressing the physical, psychological, and social aspects of addiction.
Benefit: This comprehensive care model ensures that all factors contributing to addiction are addressed, increasing the chances of long-term recovery and decreasing the likelihood of readmission.
Addiction treatment during hospitalization offers numerous advantages in preventing readmissions, including medical stabilization, comprehensive mental health care, individualized treatment, education, structured environments, and ongoing support. These factors combine to improve patients’ ability to maintain recovery, reduce relapse risks, and ensure they have the resources needed for sustained sobriety.
Disadvantages and Limitations of Hospital-Based Addiction Treatment
While addiction treatment during hospitalization requires a balance between effective care and patient autonomy. Here are some key ethical dilemmas related to addiction treatment during hospitalization can offer critical benefits, including detoxification and stabilization, there are also some disadvantages and limitations to consider. These include its potential to prevent readmissions:
1. Limited Duration of Treatment
Disadvantage: Inpatient treatment is often short-term, which means patients may not receive enough time to address the complexities of their addiction fully.
Concern: While stabilization and initial therapy are beneficial, the brief nature of hospitalization may not provide the depth of long-term recovery support needed to prevent future relapses and readmissions.
2. Over-reliance on Medical Intervention
Disadvantage: Hospitalization focuses on medical and detoxification support, which may leave gaps in other areas of recovery, such as life skills training, relationship repair, and addressing social factors that contribute to addiction.
Concern: Over-reliance on the medical model may not fully equip patients with the tools they need to succeed outside the hospital, leading to challenges in maintaining sobriety after discharge.
3. Lack of Real-World Preparation
Disadvantage: Hospital-based treatment often occurs in a controlled, safe environment, which might not adequately prepare patients for the stresses and temptations of everyday life outside the hospital.
Concern: Patients may struggle to adapt to the real-world challenges of staying sober when they face the same triggers, social pressures, and stressful situations they encountered before hospitalization.
4. High Costs
Disadvantage: Inpatient addiction treatment can be expensive, particularly if it is not covered by insurance or if the patient requires a prolonged stay.
Concern: The high cost may limit access to treatment for some individuals, potentially reducing opportunities for recovery or ongoing care. Financial strain could also lead to gaps in aftercare, increasing the risk of readmission.
5. Potential for Disconnect from Support Networks
Disadvantage: While inpatient care can be beneficial, it may isolate patients from their usual support networks, such as family, friends, or community groups.
Concern: This isolation can create a sense of disconnection or dependency on the hospital environment. Once discharged, the absence of these established support systems can contribute to feelings of loneliness or relapse.
6. Limited Focus on Long-Term Recovery
Disadvantage: Hospital treatment may focus primarily on immediate needs, such as detox and crisis management, rather than preparing patients for addiction therapy during hospitalization. While effective in many cases, this approach raises significant ethical dilemmas related to patient autonomy, confidentiality, the adequacy of care, and the integration of medical and psychological support. These moral concerns must be addressed carefully to ensure that treatment respects patients’ rights, promotes long-term recovery, and provides holistic care that considers the psychological, social, and medical aspects of addiction.
Concern: Without a clear focus on continued care, therapy, and aftercare planning, patients may face challenges in maintaining sobriety after discharge, increasing the chances of relapse and readmission.
7. Stigma and Social Reintegration Challenges
Disadvantage: Being hospitalized for addiction treatment can sometimes be stigmatizing, which may create barriers to reintegration into society, including returning to work or rebuilding personal relationships.
Concern: This stigma can hinder recovery, as patients might feel ashamed or reluctant to seek out community support, potentially increasing their vulnerability to relapse and readmission.
8. Psychological Dependency on the Hospital Environment
Disadvantage: Patients may develop a psychological dependency on the hospital environment, where they feel safe and controlled, and may struggle to navigate the less structured environment of life after discharge.
Concern: This dependency can make it difficult for patients to successfully transition to outpatient care or self-management, leading to an increased risk of relapse.
9. Lack of Holistic Treatment for Underlying Issues
Disadvantage: Hospital treatment may focus more on the immediate, physical aspects of addiction and less on underlying psychological, emotional, and social issues that contribute to substance use.
Concern: Without addressing these deeper, root causes of addiction (such as trauma, family dynamics, or unresolved psychological issues), patients may be more vulnerable to relapse when they encounter stressors in their everyday lives.
10. Possible Delay in Addressing Behavioral Patterns
Disadvantage: In some cases, inpatient programs may not have the time or resources to deeply explore the behavioral patterns and habits that contribute to addiction.
Concern: Without a strong focus on behavioral therapy, patients may not fully develop the skills and strategies needed to prevent relapse once they return to their typical environment.
While addiction treatment during hospitalization provides essential benefits, it also presents several disadvantages, such as the limited duration of treatment, high costs, potential for social disconnection, and inadequate preparation for long-term recovery. Addressing these limitations through comprehensive aftercare planning and community support is essential to reducing the likelihood of readmission and supporting sustained recovery.
Ethical Dilemmas in Addiction Treatment During Hospitalization
Addiction treatment during hospitalization requires a balance between effective care and patient autonomy. Here are some key ethical dilemmas related to addiction treatment during hospitalization and its potential to prevent readmissions:
- Informed Consent and Autonomy
- Dilemma: Patients may not be fully able to make informed decisions about their treatment due to the nature of their addiction or its impact on their cognitive functioning.
- Concern: If patients are coerced into treatment or are not given adequate information about their treatment options and outcomes, their autonomy could be compromised. This raises the ethical issue of whether the treatment is being imposed in the patient’s best interests or respects their ability to make decisions.
- Confidentiality and Privacy
- Dilemma: Addiction treatment often requires the sharing of sensitive personal and medical information. In a hospital setting, this information may be disclosed to other professionals or family members.
- Concern: There is a risk of breaching confidentiality or not fully informing the patient about how their information will be shared. While family involvement is often encouraged, patients might feel their privacy is violated, especially if the disclosure of their condition leads to stigma or discrimination.
- Coercion vs. Voluntary Treatment
- Dilemma: In some cases, patients might be hospitalized involuntarily, either due to the severity of their addiction or because they are deemed a danger to themselves or others.
- Concern: Coercive treatment might be effective in the short term, but it raises ethical questions about patient rights and autonomy. Patients may not fully engage in their treatment or recovery process if they feel forced into it, which could affect the long-term success of treatment and lead to relapse after discharge.
- Balancing Medical Intervention with Psychological and Social Factors
- Dilemma: Addiction treatment in a hospital often focuses on medical stabilization and detoxification, but it may not sufficiently address the underlying psychological, emotional, or social issues that contribute to addiction.
- Concern: Focusing too much on medical treatment might neglect the root causes of addiction, such as trauma, mental health disorders, or socio-economic factors, which could lead to an incomplete treatment approach and a higher risk of readmission if these factors aren’t addressed.
- The Risk of Over-Medicalization
- Dilemma: Hospital-based addiction treatment often leans heavily on medical interventions such as medication-assisted treatment (MAT) and detoxification, which might overshadow behavioral therapy or holistic approaches.
- Concern: Relying too heavily on medical treatment might limit the development of critical coping skills and behavioral changes needed for long-term recovery. There’s also the risk that patients may become dependent on medication or medical interventions, which could hinder their recovery journey once discharged.
- Duration of Hospitalization and Discharge Planning
- Dilemma: The duration of inpatient treatment is often limited, and patients may be discharged before they are fully prepared to manage recovery on their own.
- Concern: If discharge planning is rushed or not comprehensive enough, patients might leave the hospital without adequate support systems, relapse prevention strategies, or aftercare plans in place. This raises ethical concerns about the adequacy of care and whether patients are truly ready to transition to outpatient treatment.
- Discrimination and Stigmatization
- Dilemma: Patients undergoing addiction treatment in a hospital setting may experience stigma or discrimination from healthcare professionals or other patients.
- Concern: Stigmatization can hinder recovery, as it may cause patients to feel shame or worthlessness, which can undermine their motivation to continue treatment. Ethical concerns arise about the hospital’s responsibility to create a non-judgmental, supportive environment for patients with addiction.
- Ethical Responsibility for Aftercare and Community Integration
- Dilemma: Hospitals have an ethical responsibility to ensure that patients are not discharged into environments that might contribute to relapse, such as abusive relationships or high-risk situations.
- Concern: There is an ethical dilemma regarding the hospital’s and healthcare providers’ responsibility to provide strong aftercare and community support. Without adequate follow-up or resources for reintegration into society, patients may struggle to maintain sobriety, leading to readmission.
- Patient Engagement and Motivation
- Dilemma: Patients may not always be motivated to engage fully in treatment, either due to denial of their addiction or ambivalence about recovery.
- Concern: If patients are not motivated to participate in their own recovery, there is an ethical issue in how much intervention or persuasion is appropriate. Too much pressure to engage in treatment might compromise the patient’s autonomy, while insufficient engagement could jeopardize the effectiveness of the treatment plan.
- Cultural and Socioeconomic Sensitivity
- Dilemma: Addiction treatment in a hospital setting may not always account for the cultural, social, or economic factors that influence a patient’s experience of addiction and recovery.
- Concern: Failing to consider cultural differences or socioeconomic challenges could result in treatment plans that are less effective or even alienating to specific patients. Ethical issues arise when treatment is not culturally competent, leading to inequality in care and the potential for inadequate support.
Addiction treatment during hospitalization, while effective in many cases, raises significant ethical dilemmas related to patient autonomy, confidentiality, the adequacy of care, and the integration of medical and psychological support. These moral concerns must be addressed carefully to ensure that treatment respects patients’ rights, promotes long-term recovery, and provides holistic care that considers the psychological, social, and medical aspects of addiction.
The Role of Family Support in Preventing Readmissions During Addiction Treatment
Family support plays a crucial role in addiction treatment during hospitalization and can be key to preventing readmissions. The involvement of family members not only provides emotional and practical support but also helps ensure a stable environment for the individual after discharge. Here are some effective family support strategies that can help prevent readmissions in addiction treatment:
1. Educating Family Members about Addiction
Strategy: Family members should be educated about the nature of addiction, the recovery process, and the challenges involved in overcoming substance use disorders.
Benefit: This helps reduce stigma, promotes understanding, and enables family members to provide more compassionate and informed support. It also encourages realistic expectations regarding recovery and relapse prevention.
2. Encouraging Open Communication
Strategy: Fostering open, honest communication between the patient and their family members is vital during hospitalization and after discharge.
Benefit: Healthy communication can strengthen trust, allow patients to express their needs, and encourage family members to participate in the recovery process actively. It can help prevent isolation and misunderstandings that could lead to relapse.
3. Involving the Family in Treatment
Strategy: Involving family members in therapy sessions, group counseling, or family therapy during hospitalization can help them understand how addiction affects their loved one and what role they can play in supporting recovery.
Benefit: This approach helps family members become active participants in the recovery process, allowing them to provide ongoing support, reinforce positive behaviors, and recognize signs of potential relapse early.
4. Establishing Healthy Boundaries
Strategy: Family members should learn to set and maintain healthy boundaries with the individual in recovery, avoiding enabling behaviors or rescuing the person from the consequences of their actions.
Benefit: Setting boundaries encourages accountability and fosters independence in the person recovering from addiction. It helps create a supportive but non-enabling environment, which is crucial for long-term recovery.
5. Creating a Supportive Home Environment
Strategy: Families can work to create a stable, supportive, and substance-free environment at home by removing triggers, ensuring a routine, and providing a safe space for the recovering individual.
Benefit: A safe and supportive home environment helps reduce stress and temptations, making it easier for the individual to maintain sobriety and avoid situations that could lead to relapse and readmission.
6. Promoting Healthy Family Dynamics
Strategy: Encouraging healthy family dynamics involves addressing any codependency, enabling, or dysfunctional patterns that may have contributed to the addiction.
Benefit: Strengthening family relationships and promoting healthier interactions fosters a positive support system and reduces the likelihood of behaviors that may undermine the person’s recovery.
7. Supporting the Development of Coping Skills
Strategy: Families can encourage and support their loved ones in practicing coping strategies, such as mindfulness, stress management, and emotional regulation techniques learned during treatment.
Benefit: Developing healthy coping skills for managing stress and emotions is essential for preventing relapse. Family support in reinforcing these skills increases the chances of success in long-term recovery.
8. Assisting with Aftercare Planning
Strategy: Families can actively participate in planning aftercare options, such as outpatient therapy, support groups, or sober living arrangements, ensuring the patient has ongoing support after discharge.
Benefit: A solid aftercare plan, which includes family involvement, provides a structured and consistent support system, reducing the risk of relapse and readmission by ensuring the individual has continuous care.
9. Monitoring Progress and Providing Accountability
Strategy: Families can help monitor the individual’s progress by regularly checking in on their treatment, participating in family meetings or therapy, and offering positive reinforcement for progress made.
Benefit: Providing consistent support and accountability encourages the individual to stay committed to their recovery goals, helping to prevent setbacks that might lead to relapse and readmission.
10. Providing Emotional Support and Encouragement
Strategy: Offering ongoing emotional support, encouragement, and reassurance can help individuals feel valued and motivated in their recovery.
Benefit: Positive emotional reinforcement from family members boosts self-esteem, enhances motivation to stay sober, and helps individuals feel less isolated or hopeless during challenging moments in their recovery.
11. Helping to Reinforce Treatment Goals and Values
Strategy: Family members can help reinforce the goals and values developed during treatment by regularly discussing these goals, encouraging adherence to recovery practices, and staying involved in the individual’s progress.
Benefit: Reinforcing the treatment goals and values ensures that recovery remains a priority and that the patient stays committed to the long-term process, making it easier to prevent relapse and avoid readmissions.
12. Promoting Community Support Participation
Strategy: Encouraging family members to help their loved one engage with community resources like support groups, sober activities, or recovery networks can create a strong external support system.
Benefit: Involvement in community support increases the likelihood of sustained recovery by connecting the patient with like-minded individuals who can offer additional encouragement and understanding outside the family unit.
Conclusion: Family support strategies are essential for preventing readmissions during addiction treatment. By educating family members, fostering open communication, establishing boundaries, and maintaining a supportive home environment, families can create the foundation needed for lasting recovery. With the active involvement of family in the treatment and aftercare process, individuals are more likely to avoid relapse and stay committed to their sobriety journey.
The Role of Community Resources in Preventing Readmissions During Addiction Treatment
Community resources play a crucial role in supporting individuals with addiction during hospitalization and preventing readmissions. By providing ongoing support, stability, and access to essential services, community resources can help individuals sustain their recovery after discharge. Here are some community resource strategies that can contribute to preventing readmissions:
1. Access to Support Groups and Peer Networks
Strategy: Connecting patients with support groups such as Alcoholics Anonymous (AA), Narcotics Anonymous (NA), or other 12-step programs during and after hospitalization.
Benefit: Peer support helps individuals feel less isolated and provides them with the opportunity to share their experiences, gain insights, and receive encouragement. These groups also offer accountability, reducing the risk of relapse and readmission.
2. Aftercare Services and Outpatient Counseling
Strategy: Ensuring patients have access to outpatient counseling or therapy services, such as individual therapy, group therapy, or family therapy, after discharge.
Benefit: Continuity of care through aftercare services helps patients manage stress, cravings, and triggers in their everyday lives, preventing relapse and providing a structured approach to maintaining recovery.
3. Sober Living Environments
Strategy: Referral to sober living houses or recovery residences that provide a substance-free environment where individuals can transition back to independent living while staying surrounded by others who are in recovery.
Benefit: Sober living homes offer stability, structure, and support, which are critical during the early stages of recovery. They reduce exposure to relapse triggers and provide a safe, supportive environment that helps prevent readmission.
4. Case Management and Recovery Coaching
Strategy: Offering case management services that help individuals access resources such as healthcare, housing, employment, or legal assistance, and providing recovery coaching to guide individuals through their recovery journey.
Benefit: Case managers and recovery coaches provide personalized support and ensure individuals stay connected to necessary services. This reduces the risk of stressors or unmet needs contributing to relapse and readmission.
5. Employment Support and Vocational Training
Strategy: Referring individuals to vocational rehabilitation programs, job training, or employment placement services to help them build a sustainable livelihood.
Benefit: Stable employment can provide financial security, a sense of purpose, and a constructive focus for individuals in recovery, all of which reduce the likelihood of returning to old substance use behaviors and prevent readmission to the hospital.
6. Mental Health and Dual Diagnosis Support
Strategy: Connecting individuals to mental health professionals who specialize in dual diagnosis (co-occurring mental health and substance use disorders) to address any underlying psychological conditions contributing to addiction.
Benefit: Treating co-occurring disorders simultaneously helps address the root causes of addiction, ensuring that individuals have the necessary tools to manage both their mental health and recovery, which can prevent relapse and readmission.
7. Crisis Intervention Services
Strategy: Providing access to crisis intervention services such as hotlines, emergency counseling, or 24/7 addiction support services for individuals at risk of relapse or experiencing a mental health crisis.
Benefit: Immediate access to crisis intervention services ensures that individuals in distress are supported promptly, reducing the chance of a crisis leading to substance use and hospital readmission.
8. Recovery-Oriented Social and Recreational Activities
Strategy: Offering or connecting individuals to social and recreational activities that are specifically designed for those in recovery, such as sober events, sports leagues, or creative arts groups.
Benefit: Engaging in recovery-oriented activities promotes a healthy, substance-free lifestyle and helps individuals build a support network outside of traditional therapy or meetings, which can reduce feelings of isolation and prevent relapse.
9. Health and Wellness Programs
Strategy: Connecting patients to community-based health and wellness programs that promote physical well-being through exercise, nutrition, mindfulness, and stress reduction.
Benefit: A focus on physical health contributes to overall recovery by improving self-esteem, reducing stress, and providing positive coping mechanisms. Physical health improvements also reduce the temptation to self-medicate with substances, helping prevent relapse.
10. Access to Legal and Financial Assistance
Strategy: Referring individuals to legal services, financial counseling, or assistance programs to help them manage any legal or economic challenges that might have contributed to or resulted from their addiction.
Benefit: Addressing legal and financial concerns can reduce stress, which is a common trigger for relapse. Legal and financial stability supports long-term recovery by helping individuals focus on building a sober life.
11. Family Support and Education Programs
Strategy: Providing family members with educational resources and support groups designed to help them better understand addiction, recovery, and how to support their loved ones.
Benefit: Educating families can strengthen the home environment and create a more supportive, understanding space for the person in recovery, which reduces the likelihood of dysfunctional behaviors or enabling that could lead to relapse and readmission.
12. Ongoing Monitoring and Follow-Up
Strategy: Community resources can offer follow-up programs that track patients’ progress after they leave the hospital. These programs can include regular check-ins or phone calls to ensure they are staying on track with their treatment plan.
Benefit: Regular monitoring helps identify issues early, so patients can receive additional support before a crisis or relapse, thereby reducing the risk of readmission.
Community resources provide critical ongoing support that helps individuals maintain their recovery after hospitalization and reduce the risk of readmission. By connecting patients with aftercare services, support groups, sober living environments, and vocational programs, they are equipped with the tools they need to build a stable, sober life. Access to comprehensive community resources ensures continuous support. It helps individuals address the personal, social, and environmental factors that contribute to addiction, ultimately leading to a lower likelihood of relapse and hospital readmission.
Conclusion
Addiction treatment during hospitalization is essential for stabilizing individuals and laying the foundation for long-term recovery. While it provides immediate medical care and therapeutic support, it also presents challenges, including the potential for dependence on institutional care and ethical concerns about patient autonomy. Self-management strategies, family support, and community resources are critical in preventing relapse and ensuring a successful transition from hospitalization to everyday life. By integrating these elements, individuals are better equipped to maintain sobriety and avoid readmission, ultimately fostering sustained recovery and well-being.
Video: Can Hospitalization Really Help You Overcome Addiction?