GLP-1 receptor agonist (GLP-1 RA) therapy is an innovative treatment for alcohol use disorder (AUD), initially designed for diabetes and obesity. This therapy can reduce alcohol consumption, decrease cravings, and improve metabolic health. However, it has challenges, including side effects, individual variability, and ethical concerns related to informed consent and off-label use. Community resource strategies, such as education, comprehensive access to care, support networks, and advocacy for equitable access, are crucial to enhancing its integration into AUD treatment. These efforts can better support individuals in their recovery journey while maximizing the benefits of GLP-1 RA therapy.
GLP-1 Receptor Agonist Therapy: A Promising New Treatment for Alcohol Use Disorder
GLP-1 receptor agonist (GLP-1 RA) therapy is emerging as a potential new approach to treating alcohol use disorder (AUD). Initially developed for managing type 2 diabetes and obesity, GLP-1 receptor agonists like liraglutide and semaglutide are now being explored for their ability to reduce alcohol cravings and consumption. Here’s a closer look at how GLP-1 RA therapy works and its potential impact on AUD treatment.
Mechanism of Action
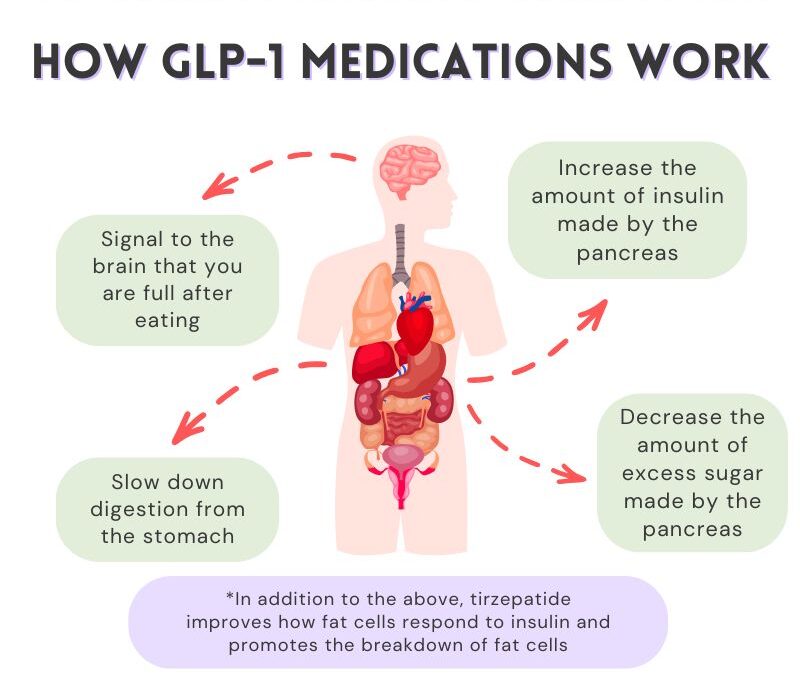
- GLP-1 Function: Glucagon-like peptide-1 (GLP-1) is a hormone that regulates appetite and glucose metabolism. Beyond its role in blood sugar control, GLP-1 also modulates brain pathways associated with reward and reinforcement.
- Impact on Alcohol Consumption: GLP-1 RAs may influence the brain’s reward system, specifically targeting pathways that drive alcohol-seeking behavior. By modulating these pathways, GLP-1 RAs can reduce the compulsion to drink, potentially lowering alcohol intake over time.
Benefits
- Reduced Alcohol Intake: Clinical studies have shown that GLP-1 RAs can reduce both the quantity and frequency of alcohol consumption. Patients using GLP-1 RAs often report fewer alcohol cravings and less frequent urges to drink.
- Weight Management: Many individuals with AUD also struggle with weight management, either due to the caloric intake from alcohol itself or related lifestyle factors. GLP-1 RAs, known for their appetite-suppressing effects, may help these individuals maintain a healthier weight as part of their recovery.
- Metabolic Benefits: People with AUD frequently face metabolic issues, including insulin resistance and liver problems. By improving blood sugar levels and supporting metabolic health, GLP-1 RAs may help address these complications, contributing to overall physical recovery.
Considerations
- Side Effects: Like any medication, GLP-1 RAs have potential side effects. Common issues include gastrointestinal symptoms like nausea, vomiting, and diarrhea, as well as a rare but severe risk of pancreatitis. Regular monitoring can help manage these effects and ensure safe use.
- Individual Variation: The effectiveness of GLP-1 RA therapy may vary widely. While some individuals may experience significant reductions in alcohol cravings, others may see minimal effects. Further research is needed to determine which patient populations are most likely to benefit from this therapy.
Research and Future Directions
Ongoing research examines the efficacy and safety of GLP-1 RAs specifically for AUD, including studies on optimal dosing, potential long-term effects, and how these medications fit into a comprehensive treatment plan. As research advances, we may better understand how to use GLP-1 RAs effectively alongside other therapies, such as counseling and behavioral support.
In summary, GLP-1 receptor agonist therapy represents a novel approach to treating alcohol use disorder by targeting pathways associated with reward and appetite. With promising evidence supporting its potential to reduce alcohol intake, GLP-1 RA therapy could be a valuable tool in addiction recovery. However, more research is needed to solidify its role in AUD treatment, ensuring that it is safe, effective, and appropriately integrated into broader recovery programs.
Challenges of GLP-1 Receptor Agonist Therapy in Alcohol Use Disorder
GLP-1 receptor agonist (GLP-1 RA) therapy, originally used to treat type 2 diabetes and obesity, is now being explored for alcohol use disorder (AUD). Despite its promising potential to reduce alcohol cravings and consumption, GLP-1 RA therapy comes with notable challenges. Here’s an overview of the main disadvantages and considerations for using GLP-1 RAs in AUD treatment.
1. Side Effects
- Gastrointestinal Issues: GLP-1 RAs often cause gastrointestinal side effects like nausea, vomiting, diarrhea, and abdominal discomfort. For individuals already managing symptoms related to alcohol use, these side effects can exacerbate pain.
- Risk of Pancreatitis: A rare but serious risk of pancreatitis is associated with GLP-1 RAs. Careful monitoring is essential, particularly for patients with a history of pancreatic problems.
2. Cost and Accessibility
- High Costs: The expense of GLP-1 RAs can be a barrier for many, especially as insurance does not always cover these medications for AUD.
- Limited Availability: Since GLP-1 RAs are traditionally used for diabetes and weight management, not all healthcare providers are familiar with prescribing them for AUD. This limited knowledge can reduce access to appropriate care for patients seeking these treatments.
3. Individual Variation in Response
- Variable Efficacy: Treatment responses can vary significantly. Genetic factors, co-occurring health conditions, and individual preferences can influence how well a patient responds to GLP-1 RA therapy.
- Potential for Ineffectiveness: For some, GLP-1 RAs may not significantly reduce alcohol cravings or consumption, which can lead to frustration and diminished motivation.
4. Need for Lifestyle Adjustments
- Dietary Changes: Patients often need to make nutritional adjustments to minimize gastrointestinal side effects. For individuals with established dietary habits, this requirement can add an extra layer of difficulty.
5. Withdrawal Management Complications
- Complicating Withdrawal: Initiating GLP-1 RA therapy during active alcohol withdrawal may intensify gastrointestinal side effects, making withdrawal symptoms more challenging to manage and potentially increasing patient discomfort.
6. Limited Research
- Emerging Evidence: While early studies show potential, the body of evidence on GLP-1 RA therapy specifically for AUD is limited. More robust, large-scale clinical trials are needed to confirm the efficacy, safety, and optimal use of GLP-1 RAs in AUD treatment.
7. Potential for Psychological Dependency
- Medication Reliance: There’s a risk that patients may become reliant on the medication alone without addressing the behavioral and psychological factors that underlie their alcohol use disorder. Effective treatment for AUD often requires a holistic approach that goes beyond medication.
8. Ethical Considerations
- Informed Consent: Given the emerging nature of GLP-1 RA therapy for AUD, ensuring patients fully understand the benefits and risks can be challenging. Providers must carefully navigate informed consent to empower patients to make well-informed treatment choices.
GLP-1 RA therapy presents both promising benefits and significant challenges in treating alcohol use disorder. Potential disadvantages include side effects, variable patient responses, and accessibility and cost issues. While this therapy may offer new hope for reducing alcohol cravings, careful consideration and additional research are essential to establish its role within comprehensive AUD management strategies.
Ethical Considerations of GLP-1 Receptor Agonist Therapy in Alcohol Use Disorder
GLP-1 receptor agonist (GLP-1 RA) therapy is gaining attention as a potential treatment for alcohol use disorder (AUD). Designed initially for managing diabetes and obesity, these medications are now being studied for their ability to reduce alcohol cravings. However, this off-label use raises complex ethical questions for healthcare providers. Here are the central ethical dilemmas associated with the use of GLP-1 RAs for AUD.
1. Informed Consent
- Complexity of Information: Given the emerging research, patients may struggle to fully understand the implications of using GLP-1 RA therapy for AUD. Providers must communicate the risks, benefits, and uncertainties, especially since the medication isn’t approved explicitly for AUD.
2. Off-Label Use
- Ethical Justification: Prescribing GLP-1 RAs for AUD is off-label, meaning the FDA has not explicitly approved their use for this indication. Providers face the ethical challenge of justifying their use based on limited evidence, weighing their clinical judgment against established standards.
3. Access and Equity
- Disparities in Treatment: The cost and availability of GLP-1 RAs may prevent equitable access, particularly for low-income patients who might benefit from this treatment. Providers must grapple with ethical concerns around healthcare equity and whether all patients have a fair chance to access effective treatment options.
4. Balancing Risks and Benefits
- Managing Side Effects: GLP-1 RAs carry risks, including gastrointestinal discomfort and, in rare cases, pancreatitis. Providers must ethically weigh these side effects against the potential benefits for each patient, navigating the dilemma of when the positives outweigh the potential harm.
5. Individualized Treatment
- Variability in Response: Not all patients respond similarly to GLP-1 RA therapy, which raises ethical questions about a one-size-fits-all approach. Providers are tasked with personalizing treatment plans while setting realistic expectations for patients.
6. Dependency Concerns
- Psychological Implications: There’s a risk that patients may become reliant on the medication rather than addressing deeper behavioral or psychological issues related to AUD. This raises ethical concerns about the goals of addiction treatment and the importance of sustainable recovery beyond pharmacological dependence.
7. Research and Development
- Transparency in Research: The ethical obligation to be open in research includes disclosing potential conflicts of interest and publishing both positive and negative findings. This transparency is crucial for building trust and ensuring providers make informed, ethical treatment decisions.
8. Impact on Treatment Goals
- Focus on Medication vs. Therapy: There’s a risk that using GLP-1 RA therapy might overshadow essential behavioral therapies and psychosocial support, which are crucial for comprehensive addiction treatment. Providers must consider the ethical implications of prioritizing medication over holistic care.
9. Long-Term Implications
- Future of Treatment: As GLP-1 RAs are still under investigation for AUD, the long-term effects and potential implications are unknown. Using an emerging treatment without fully understanding its long-term impact poses ethical challenges that require careful consideration.
Using GLP-1 RA therapy for alcohol use disorder involves a range of ethical considerations. These include informed consent, access to treatment, balancing risks and benefits, and ensuring individualized care. Addressing these ethical dilemmas requires open communication, commitment to patient autonomy, and a thoughtful approach to integrating new treatments into addiction recovery strategies.
Community Resource Strategies for Implementing GLP-1 Receptor Agonist Therapy in Alcohol Use Disorder Treatment
The use of GLP-1 receptor agonist (GLP-1 RA) therapy for alcohol use disorder (AUD) is emerging as a promising approach for reducing alcohol cravings. Community-based strategies are essential to ensure patients access this treatment, understand its potential benefits and side effects, and receive comprehensive support. Here are some key community resource strategies to effectively implement GLP-1 RA therapy for AUD.
1. Education and Awareness Programs
- Community Workshops: Hosting workshops for healthcare providers and community members can foster understanding about GLP-1 RAs for AUD. These sessions can cover potential benefits, side effects, and the role of GLP-1 RA therapy in a broader treatment plan.
- Informational Campaigns: Developing brochures, pamphlets, and online resources can help educate patients and families on the purpose of GLP-1 RA therapy and its integration into comprehensive care.
2. Access to Healthcare Providers
- Training for Providers: It is crucial to offer specialized training for healthcare professionals on GLP-1 RA therapy in AUD treatment. Training can cover patient selection, monitoring, and managing side effects to ensure quality care.
- Referral Networks: Establishing referral networks between patients and trained providers can enhance access to knowledgeable practitioners and streamline treatment initiation.
3. Support Groups and Peer Counseling
- Peer Support Programs: Setting up support groups allows individuals using GLP-1 RAs to share their journeys, challenges, and successes in managing AUD. This can foster a sense of community and encouragement.
- Peer Navigators: Training individuals who have successfully used GLP-1 RAs can provide a support network for new patients, offering guidance and practical insights into the treatment process.
4. Access to Comprehensive Care
- Integrated Treatment Programs: Developing programs that combine GLP-1 RA therapy with behavioral therapies, counseling, and mental health services is essential for treating AUD holistically and addressing underlying issues.
- Holistic Health Services: Providing complementary therapies, such as nutrition counseling, exercise programs, and mindfulness practices, can support overall well-being and improve treatment outcomes.
5. Monitoring and Follow-Up Services
- Regular Check-Ins: Implementing regular follow-ups allows providers to monitor patients’ responses to GLP-1 RA therapy, make necessary adjustments, and address any emerging concerns.
- Data Collection: Establishing a database to track outcomes related to GLP-1 RA therapy for AUD can help inform best practices and contribute to the growing body of research.
6. Crisis Intervention Resources
- Emergency Support Services: Making crisis intervention resources available ensures patients experiencing severe withdrawal symptoms or other crises related to AUD receive timely help.
- 24/7 Helplines: Dedicated helplines provide patients with immediate support and guidance on their treatment when needed.
7. Research and Clinical Trials
- Collaboration with Research Institutions: Partnering with universities and research organizations to study GLP-1 RAs for AUD can enhance the evidence base and improve treatment protocols.
- Encouraging Participation: Informing patients about ongoing clinical trials can provide access to new treatments while advancing research in AUD treatment.
8. Policy Advocacy
- Advocacy for Funding: Working with local and state governments to secure funding can support community-based programs focused on GLP-1 RA therapy in AUD treatment.
- Support for Regulations: Advocating for policies that ensure the safe and effective use of GLP-1 RAs in AUD treatment fosters responsible implementation and accessibility.
9. Online Resources and Telehealth
- Telehealth Services: Offering telehealth options for consultations and follow-up appointments can help patients access care without geographic constraints.
- Educational Websites: Developing online platforms with articles, videos, and forums can educate patients on GLP-1 RA therapy and provide a community for shared experiences.
10. Community Partnerships
- Collaboration with Nonprofits: Partnering with nonprofit organizations that focus on addiction recovery can provide additional support and resources to patients using GLP-1 RAs for AUD.
- Engagement with Local Health Departments: Integrating GLP-1 RA therapy into community health initiatives ensures its accessibility as part of broader public health resources for AUD treatment.
Implementing these community resource strategies can create a strong support network for individuals considering or using GLP-1 RA therapy for alcohol use disorder. By educating the public, training providers, and developing comprehensive care models, communities can foster a well-rounded and accessible approach to AUD treatment with GLP-1 RA therapy.
Conclusion
GLP-1 receptor agonist (GLP-1 RA) therapy presents a promising avenue for addressing alcohol use disorder (AUD), offering benefits such as reduced cravings and improved metabolic health. However, its implementation is challenging, including potential side effects, variability in patient responses, and ethical dilemmas surrounding informed consent and off-label use. To maximize the effectiveness of this therapy, community resource strategies play a vital role in providing education, enhancing access to comprehensive care, and fostering support networks. By navigating these complexities thoughtfully, healthcare providers can better leverage GLP-1 RA therapy to support individuals in their recovery from AUD, ultimately improving treatment outcomes and quality of life.
Video: 5 Things GLP-1 Receptor Agonists Can Do for Alcohol Cravings