Glucagon-like peptide-1 (GLP-1) drugs are emerging as a promising treatment for addiction, especially in managing obesity and substance use disorders. Initially developed for type 2 diabetes, these medications help reduce cravings but come with side effects like gastrointestinal issues and pancreatitis risk. Disadvantages include high costs and the need for injections, along with ethical concerns about access, informed consent, and weight stigma. Self-management strategies, such as healthy eating and exercise, empower individuals, while family support enhances emotional encouragement. Community resources like healthcare access and support groups further strengthen the necessary support systems for those using GLP-1 medications in addiction treatment. Exploring these aspects helps us understand the complexities of using GLP-1 drugs and the comprehensive support required for recovery.
Exploring GLP-1 Agonists in Addiction Treatment: Mechanisms and Emerging Research
GLP-1 (glucagon-like peptide-1) receptor agonists, widely known for managing type 2 diabetes and obesity, are now gaining attention as a potential treatment for addiction. Originally developed to help regulate blood sugar and suppress appetite, these medications may also influence the brain’s reward systems, offering promising new avenues for addiction management. Here’s how GLP-1 agonists are thought to work in addressing addictive behaviors and the current evidence supporting their potential.
Mechanisms of Action
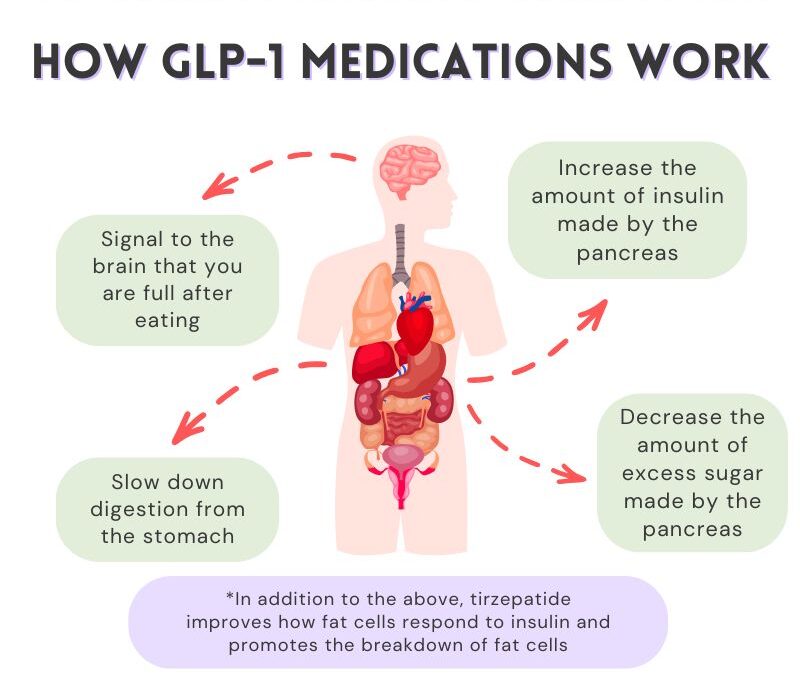
1. Appetite Regulation:
GLP-1 plays a crucial role in appetite suppression and controlling food intake. By promoting satiety, these drugs may help reduce cravings—not only for food but also for addictive substances like alcohol and drugs. This appetite regulation may benefit individuals with addiction by decreasing the intensity of cravings that drive compulsive behaviors.
2. Reward System Modulation:
GLP-1 receptors are found in brain regions associated with reward, including the nucleus accumbens, a critical area for addiction. Activating these receptors can affect the dopamine pathways that reinforce addictive behaviors. This modulation may decrease the reinforcing, “rewarding” effects of addictive substances, potentially weakening addiction’s hold on the individual.
3. Reduction in Substance Cravings:
Research shows that GLP-1 agonists may reduce cravings for substances like alcohol and nicotine. For individuals with substance use disorders, managing cravings is crucial in avoiding relapse, and GLP-1 drugs may offer a pharmacological aid to help sustain recovery.
4. Neuroprotection:
Some studies suggest GLP-1 has neuroprotective effects, which could help mitigate neurological damage caused by chronic substance abuse. These protective effects may support brain health during recovery, lowering the likelihood of relapse by promoting overall neurological well-being.
Research Evidence
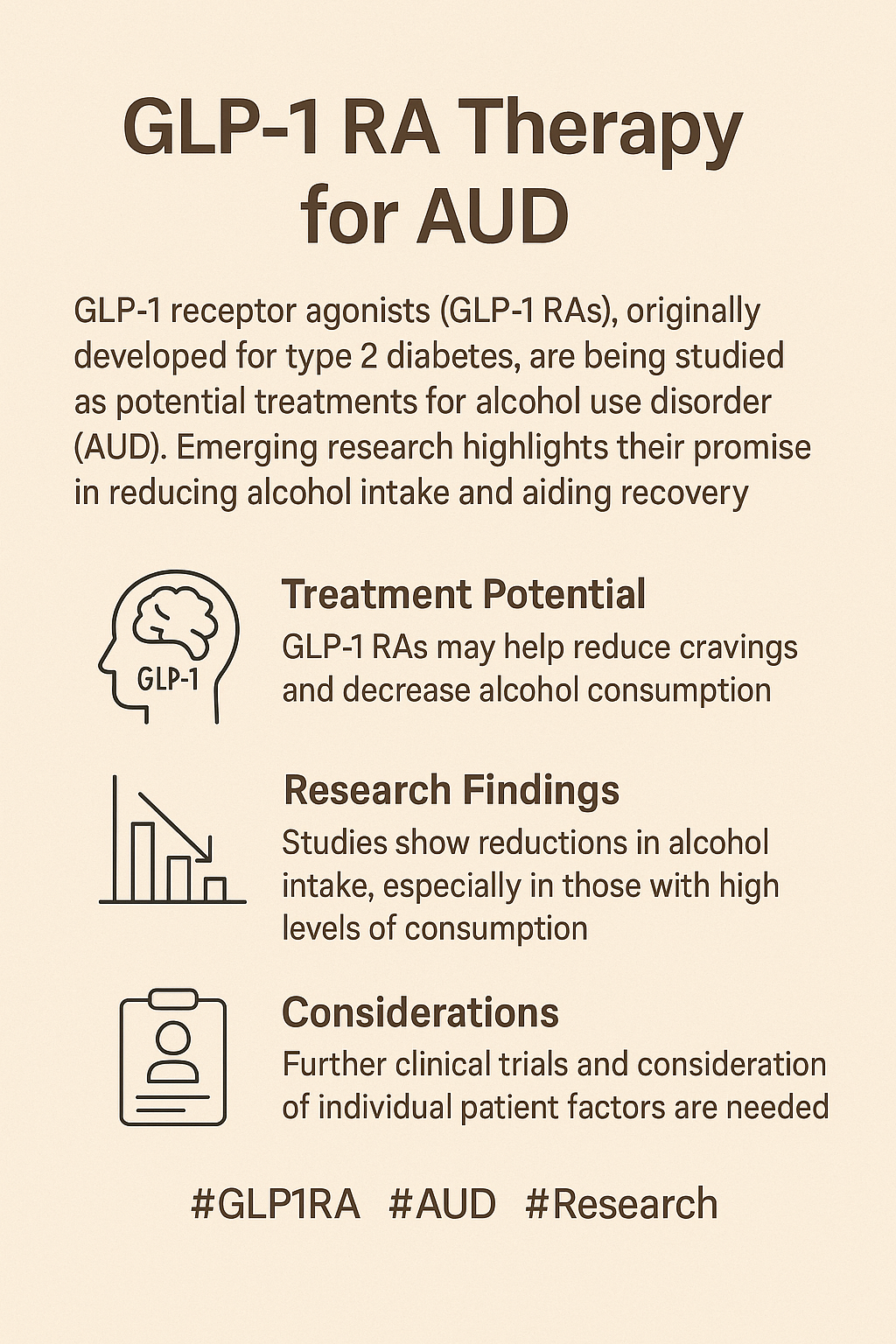
1. Alcohol Use Disorder:
Clinical studies have demonstrated that GLP-1 receptor agonists can reduce alcohol intake and cravings among individuals with alcohol use disorder. For instance, one study on liraglutide, a GLP-1 agonist, found that participants reported reduced alcohol consumption and lower craving intensity, suggesting it may have a role in treating alcohol dependence.
2. Opioid Addiction:
Emerging studies suggest GLP-1 drugs may have a role in opioid addiction as well. Animal studies show that activating GLP-1 receptors could reduce opioids’ rewarding effects, indicating the potential for opioid use disorder treatment. While still in the early stages, this research offers hope for broadening addiction treatment options.
In summary, GLP-1 drugs are not yet standard in addiction treatment, but their unique mechanisms—impacting appetite, reducing cravings, and modulating the brain’s reward pathways—hold significant promise for managing addiction. Ongoing research will be essential to fully understand the benefits and limitations of GLP-1 agonists for treating substance use disorders. As the evidence base grows, these medications may pave the way for a new class of addiction treatments, potentially transforming the landscape of addiction recovery.
Understanding the Side Effects of GLP-1 Receptor Agonists: A Comprehensive Guide
GLP-1 (glucagon-like peptide-1) receptor agonists are widely used for managing type 2 diabetes and, increasingly, for weight management. Although these medications are generally well-tolerated and practical, they can have side effects. Knowing what to expect can help patients manage them and recognize when to seek medical attention. Here’s a guide to common and severe side effects associated with GLP-1 drugs.
Common Side Effects
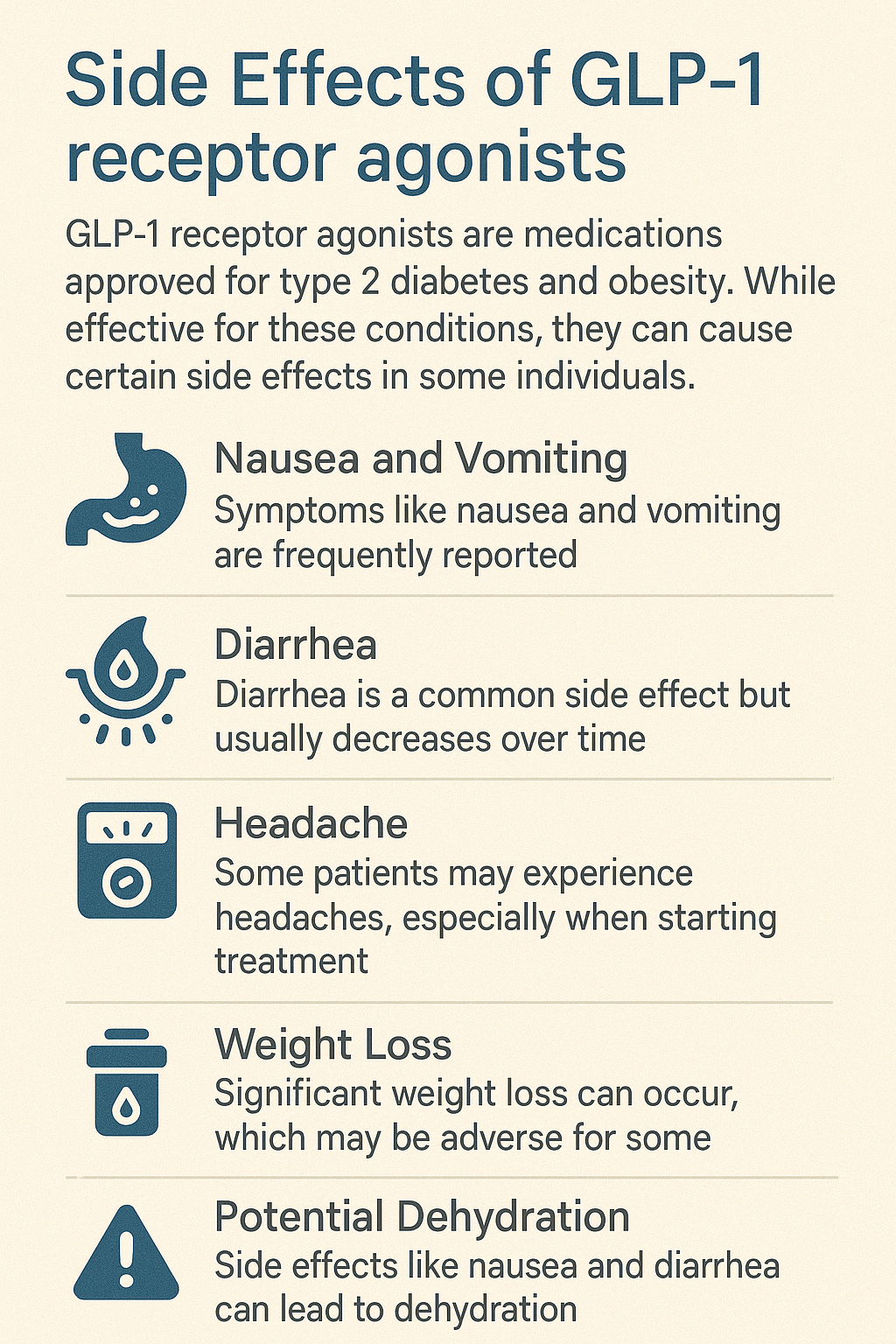
1. Gastrointestinal Issues
- Nausea: Common, especially at the beginning of treatment or with dose increases.
- Vomiting: Some individuals may experience vomiting, often related to nausea.
- Diarrhea: Loose stools can occur, particularly in the early stages.
- Constipation: Conversely, some may experience constipation as a response.
2. Appetite Changes
- Reduced Appetite: While this can support weight loss goals, it may be uncomfortable for some.
- Indigestion and Abdominal Discomfort include bloating, heartburn, and stomach pain.
3. Headache and Fatigue
- Headache: Often reported when starting the medication.
- Fatigue: Tiredness can occur as the body adjusts to GLP-1 drugs.
Serious Side Effects
1. Pancreatitis
- GLP-1 drugs have been associated with pancreatitis (inflammation of the pancreas), which presents with severe abdominal pain, nausea, vomiting, and sometimes fever. Immediate medical care is essential if these symptoms arise.
2. Kidney Issues
- GLP-1 drugs can impact kidney function, particularly in those with pre-existing kidney problems. Symptoms include decreased urine output and swelling in the legs or ankles.
3. Allergic Reactions
- Although rare, allergic reactions like rash, itching, or swelling may require immediate attention.
4. Thyroid Tumors
- Animal studies link GLP-1 drugs to potential thyroid C-cell tumors, although human relevance is unclear. Patients should be monitored for symptoms like a lump in the neck or hoarseness.
5. Hypoglycemia
- While less common than with some other diabetes medications, GLP-1 drugs can cause low blood sugar, especially if combined with other treatments for diabetes.
Other Considerations
1. Injection Site Reactions
- Some users may experience redness, swelling, or itching at injection sites.
2. Medication Interactions
- Discussing all medications with a healthcare provider is essential, as GLP-1 drugs can interact with certain medications.
GLP-1 receptor agonists are valuable tools for managing type 2 diabetes and aiding in weight loss, but they can cause side effects ranging from mild to serious. Patients should be aware of these potential issues and communicate regularly with healthcare providers to ensure the safe and effective use of GLP-1 medications. Recognizing symptoms and seeking timely medical care can optimize treatment outcomes and safety.
Understanding the Disadvantages of GLP-1 Medications: Key Considerations for Patients
GLP-1 (glucagon-like peptide-1) medications are widely used for managing type 2 diabetes and obesity due to their effectiveness in controlling blood sugar and aiding weight loss. However, these drugs come with their own set of limitations and potential drawbacks. Here’s an overview of some critical disadvantages patients should consider when starting or continuing GLP-1 medications.
1. Gastrointestinal Side Effects
Many users experience issues such as nausea, vomiting, diarrhea, and constipation, particularly when beginning treatment or adjusting doses. While these symptoms may lessen over time, they can be uncomfortable and disrupt daily life.
2. Injection Administration
Most GLP-1 drugs require subcutaneous injection, which can be inconvenient or intimidating compared to oral medications. Patients may also need training on injection techniques and site rotation, adding an extra layer of complexity.
3. Cost Considerations
GLP-1 medications are often costly, and insurance coverage may be limited. This financial burden can be a barrier for those without comprehensive insurance or high out-of-pocket costs.
4. Potential for Unintended Weight Loss
While weight loss is typically desired, some patients may experience excessive weight loss, which could lead to nutritional deficiencies or other health concerns, particularly for those already at a lower weight.
5. Risk of Pancreatitis
A serious complication, pancreatitis, can occur with GLP-1 medications. Symptoms like severe abdominal pain and vomiting require immediate medical attention and may necessitate discontinuation of the drug.
6. Thyroid Tumor Concerns
Animal studies indicate a risk of thyroid C-cell tumors with GLP-1 medications, though human relevance remains uncertain. Despite this, the potential risk may be concerning to patients, particularly those with thyroid issues.
7. Impact on Kidney Function
GLP-1 drugs may affect kidney function, especially in patients with pre-existing kidney disease. Monitoring kidney health is essential for those on long-term treatment to mitigate potential complications.
8. Hypoglycemia Risk with Other Medications
Though the risk is lower compared to insulin, combining GLP-1 medications with other diabetes treatments that reduce blood sugar can increase the likelihood of hypoglycemia, requiring careful management.
9. Limited Long-Term Data
While studies have been conducted for several years, long-term safety and efficacy data for GLP-1 medications, especially newer options, are still emerging, creating uncertainty for patients and providers alike.
10. Individual Variability
Responses to GLP-1 drugs vary widely. Some patients may not experience the desired effects, while others find side effects intolerable, underscoring the need for personalized treatment approaches.
In summary, GLP-1 medications provide significant benefits for managing diabetes and supporting weight loss, yet they also come with disadvantages that can impact treatment decisions. Patients are encouraged to discuss these pros and cons openly with healthcare providers to ensure a clear understanding of what to expect and how best to manage any side effects. This collaborative approach can empower patients to make informed choices aligned with their health goals.
Ethical Considerations in the Use of GLP-1 Medications for Diabetes and Obesity Management
GLP-1 (glucagon-like peptide-1) medications offer promising benefits for managing type 2 diabetes and obesity, but their use presents significant ethical challenges. Critical issues around access, informed consent, societal perceptions, and long-term implications require careful consideration by healthcare providers and patients. Here’s a closer look at some ethical dilemmas tied to GLP-1 treatment options.
1. Access and Equity
- Cost and Affordability: These medications are costly, and coverage is not universal, raising ethical concerns about unequal access. Patients without financial resources may be unable to access these treatments, potentially widening health inequities.
- Healthcare Disparities: Limited access to GLP-1 medications can exacerbate disparities, particularly among low-income or marginalized groups who face existing barriers to care.
2. Informed Consent
- Understanding Risks and Benefits: Patients should be fully informed about the risks, benefits, and potential side effects. Given the complexity of GLP-1 medications, healthcare providers must help patients understand these factors for informed consent.
- Vulnerable Populations: Special attention is needed when prescribing to individuals with cognitive impairments or vulnerable populations, as they may have a limited understanding of the treatment’s risks and benefits.
3. Weight Stigma and Body Image
- Perpetuating Stigmas: Promoting GLP-1 medications for weight loss can unintentionally reinforce societal weight stigmas, which can negatively impact individuals’ self-esteem and mental health.
- Overemphasis on Weight Loss: Focusing primarily on weight loss as a health outcome may overshadow the broader goals of overall well-being, potentially creating ethical tensions in patient care.
4. Long-term Effects and Research Uncertainty
- Unknown Long-term Outcomes: With ongoing research into GLP-1 medications’ long-term effects, prescribing these drugs without complete long-term data raises ethical questions about exposing patients to potential unknown risks.
- Animal Research Concerns: Animal studies show that risks such as thyroid tumors may not always translate directly to human health. How these findings are communicated to patients remains an ethical consideration.
5. Off-Label Use and Potential for Misuse
- Prescribing Beyond Indications: The off-label use of GLP-1 medications, especially for non-diabetic individuals seeking weight loss, poses ethical concerns about appropriate prescribing practices and motivations.
- Risk of Misuse: Given the potential desire for weight loss, patients may seek GLP-1 drugs without a genuine medical need, raising ethical considerations for healthcare providers when evaluating such requests.
6. Informed Decision-Making
- Balancing Patient Autonomy: Patients may reject GLP-1 medications despite clear health indications. Providers must carefully balance patient autonomy with sound medical advice to respect individuals’ rights to make decisions.
- Encouraging Lifestyle Change: The availability of GLP-1 drugs may encourage a quick-fix approach, in which patients may choose medication over sustainable lifestyle adjustments, raising concerns about promoting a holistic view of health.
Ethical dilemmas surrounding GLP-1 medications highlight the need for a balanced approach in healthcare. Addressing these issues through open dialogue, clear patient-provider communication, and thoughtful prescribing practices is crucial to ensure ethical integrity in treatment decisions. Ongoing discussions among providers, patients, and policymakers can help address these challenges, support effective treatment, and respect patient rights.
Enhancing Addiction Recovery with GLP-1 Receptor Agonists: Self-Management Strategies for Success
Using GLP-1 receptor agonists as part of an addiction recovery plan has shown promising results, especially when combined with self-management practices, behavioral therapies, and lifestyle changes. Originally designed to treat type 2 diabetes and obesity, GLP-1 drugs are now recognized for their potential to reduce cravings and influence the brain’s reward system in addiction treatment. Here’s a guide to effective self-management strategies for individuals using GLP-1 medications in their recovery journey.
1. Education and Awareness
Learn About GLP-1 Drugs
Knowing how GLP-1 medications work, their benefits, and potential side effects helps individuals make informed treatment decisions.
Recognize Triggers
Identifying personal triggers for cravings and documenting them in a journal can reveal patterns that lead to substance use and help in managing them.
2. Monitor Progress
Keep a Journal
Tracking food intake, cravings, and mood each day can help gauge how effectively GLP-1 medication is working to reduce cravings.
Set SMART Goals
Establishing specific and measurable goals, like reducing substance use or improving dietary habits, provides clear milestones for success.
3. Integrate Healthy Habits
Balanced Nutrition
A healthy diet rich in fruits, vegetables, and lean proteins complements GLP-1’s appetite-suppressing effects and supports overall health.
Regular Exercise
Physical activity can enhance mood, decrease cravings, and boost motivation, all of which are essential for long-term recovery.
4. Practice Behavioral Strategies
Mindfulness and Stress Management
Meditation and deep breathing can reduce stress, making cravings more manageable.
Develop Coping Skills
Creating a toolkit of strategies, such as distraction, hobbies, or reaching out to support networks, helps one effectively deal with cravings.
5. Build a Support System
Participate in Therapy
Behavioral therapies like cognitive-behavioral therapy (CBT) or motivational interviewing address the psychological side of addiction.
Join Support Groups
Engaging with support groups or online communities offers accountability and shared encouragement from others on similar journeys.
6. Medication Management
Follow Prescribing Guidelines
Adhering to the prescribed GLP-1 dosage and schedule is essential. Always consult a healthcare provider before making adjustments.
Regular Health Check-ins
Ongoing appointments with a healthcare provider can track progress, adjust treatment, and address any side effects.
7. Avoid Substance Triggers
Reduce Exposure
Avoiding high-risk environments or situations that trigger cravings is a proactive step toward staying on track.
Plan for High-Risk Situations
Prepare strategies to handle cravings when they arise, helping maintain control in challenging moments.
8. Celebrate Milestones
Acknowledge Progress
Celebrating small achievements, like reducing substance use or making healthier choices, reinforces positive behaviors and boosts motivation.
In summary, GLP-1 receptor agonists, when combined with self-management strategies and a solid support network, can be powerful tools in treating addiction. By educating themselves, setting goals, and building coping mechanisms, individuals can strengthen their recovery and reduce the risk of relapse. Always consult with healthcare providers to guide treatment, ensuring a comprehensive, supportive approach to overcoming addiction.
Family Resource Strategies for Supporting GLP-1 Treatment in Addiction Recovery
Family support can significantly enhance the effectiveness of GLP-1 medications in treating addiction by providing a stable, understanding, and encouraging environment. By actively participating in a loved one’s recovery journey, family members can help improve treatment outcomes. Here are resource strategies that families can implement to support individuals using GLP-1 drugs for addiction treatment.
1. Education and Awareness
- Understand GLP-1 Medications: Family members should educate themselves about the role of GLP-1 drugs in addiction treatment, including potential benefits and side effects. This foundation of knowledge enables families to offer informed support.
- Learn About Addiction: Understanding addiction as a multifaceted condition can reduce stigma and build empathy. Resources like books, online courses, and support groups can provide valuable insights into addiction’s complexities.
2. Create a Supportive Environment
- Encourage Healthy Habits: Families can promote a healthy lifestyle by incorporating nutritious meals and regular physical activity. Cooking and planning meals together fosters a positive environment that supports recovery.
- Reduce Temptations: Minimize access to substances that may trigger cravings. Clearing the home of alcohol, unhealthy foods, or other addictive substances can help prevent relapse.
3. Open Communication
- Encourage Open Dialogue: A judgment-free atmosphere for discussing cravings, challenges, and progress can strengthen trust and support.
- Practice Active Listening: Listening attentively when a loved one shares experiences helps them feel understood and valued, reinforcing positive communication.
4. Engage in Joint Activities
- Participate in Therapy Together: Family therapy can help address dynamics that influence addiction and strengthen the support system.
- Plan Sober Activities: Enjoying substance-free activities as a family—such as outdoor hikes, games, or other hobbies—helps create new, positive experiences that support sobriety.
5. Develop Coping Strategies Together
- Collaborative Problem Solving: Brainstorm solutions to manage triggers or high-risk situations as a family, helping reinforce the individual’s coping mechanisms.
- Practice Mindfulness: Family mindfulness practices like meditation or yoga can reduce stress and create a calm, supportive home environment.
6. Support Therapy and Medication Management
- Encourage Adherence: Remind the individual to follow their medication regimen and attend appointments to ensure treatment consistency.
- Track Progress Together: Keeping a shared journal or chart to mark progress and celebrate milestones can boost motivation and reinforce success.
7. Seek Professional Support
- Involve Healthcare Providers: Encourage open communication with healthcare providers to ensure the individual receives well-rounded care.
- Utilize Family Support Services: Community resources such as counseling, family support groups, and online forums can provide family members with additional guidance and emotional support.
8. Develop Boundaries and Self-Care
- Establish Healthy Boundaries: Set clear boundaries about each person’s role in support to avoid enabling behaviors and maintain family well-being.
- Prioritize Self-Care: Family members should also practice self-care to maintain their emotional and mental resilience, allowing them to provide more effective support.
Implementing these family resource strategies creates a supportive environment for individuals using GLP-1 medications in addiction treatment. A collaborative and informed approach can foster progress and resilience, enhancing the recovery journey and strengthening family bonds.
Enhancing Addiction Recovery with GLP-1 Medications: Community Resource Strategies
Community resources play a vital role in supporting individuals using GLP-1 medications for addiction treatment. Communities can significantly enhance recovery outcomes by providing education, access to healthcare, peer networks, and a healthy environment. Here are strategies that communities can implement to support individuals in their journey to overcome addiction with the help of GLP-1 drugs.
1. Education and Awareness Campaigns
- Public Information Sessions: Organize workshops and seminars to educate the community about GLP-1 medications, addiction, and the importance of holistic health. These sessions can demystify the process and encourage supportive attitudes.
- Distribute Informational Materials: Create brochures, flyers, and online content explaining GLP-1 medications, their role in addiction recovery, and local resources available. Accessible information can empower individuals and families.
2. Access to Healthcare Services
- Support Local Clinics: Encourage local health centers to offer services by healthcare professionals trained in GLP-1 medications and addiction treatment. This ensures patients have access to knowledgeable care providers.
- Offer Comprehensive Care: Promote integrated care models that combine addiction treatment with diabetes and weight management support. Such services make it easier for patients to address interconnected health issues in one setting.
3. Support Groups and Peer Networks
- Establish Peer Support Groups: Create dedicated support groups for individuals using GLP-1 drugs in recovery. Peer groups offer a safe space for sharing challenges, successes, and coping strategies.
- Facilitate Family Support Programs: Family members play a crucial role in recovery. Family support groups focused on education and coping strategies can strengthen their ability to support loved ones effectively.
4. Crisis Intervention Services
- Develop Crisis Hotlines: Provide 24/7 hotlines for individuals in crisis, offering immediate support and resources for those struggling with cravings, relapse risks, or other challenges.
- Train Community Responders: Equip first responders and community workers with training on addiction and GLP-1 medications to ensure they can effectively assist in emergencies.
5. Healthy Lifestyle Promotion
- Community Fitness Programs: Organize exercise groups, classes, or recreational activities that promote physical well-being and social connection, creating supportive, substance-free environments.
- Nutrition Education: Host cooking and nutrition classes that highlight healthy eating habits. These classes complement the appetite-regulating effects of GLP-1 drugs and promote sustained recovery.
6. Collaboration with Local Businesses
- Partner with Local Pharmacies: Work with pharmacies to provide consultations about GLP-1 medications, helping patients manage dosage, side effects, and treatment adherence.
- Engage Restaurants and Cafes: Collaborate with eateries to create healthy menu options and promote initiatives that support recovery, like “healthy choices” meal discounts or nutrition-based community events.
7. Advocacy and Policy Support
- Advocate for Policy Changes: Support local and state policies that expand access to addiction treatments and medications, including insurance coverage for GLP-1 drugs.
- Promote Stigma Reduction: Host community events and campaigns that reduce the stigma associated with addiction and medication use, fostering a more compassionate and understanding environment.
8. Research and Evaluation
- Conduct Community-Based Research: Support studies evaluating the effectiveness of GLP-1 drugs within the community. Community-based research can improve understanding and shape interventions tailored to local needs.
- Gather Feedback: Regularly solicit feedback from individuals and families using GLP-1 drugs in recovery. This helps ensure that community programs remain relevant and responsive to the needs of those in treatment.
By implementing these community strategies, neighborhoods can create a supportive and holistic environment for individuals using GLP-1 drugs in their addiction treatment. Through education, healthcare access, support networks, and a focus on healthy lifestyles, communities can contribute to improved recovery outcomes and overall well-being.
Frequently Asked Questions
Here are some common questions:
Question: Provide a patient decision aid or a discussion guide to use with providers or peer supporters
Answer: GLP-1 & Addiction: Patient Decision Aid + Discussion Guide
🧠 1. What Is This About?
This guide will help you:
- Understand the risks and benefits
- Clarify how you feel about using a medication like this
- Prepare to talk with your doctor, counselor, or peer support team
🔍 2. Key Facts
| 💊 What It Is | A class of medications that reduces cravings, appetite, and reward sensitivity |
|---|---|
| 📋 FDA Approval | Approved for diabetes and obesity, not yet for addiction |
| 📉 Potential Benefits | Reduces cravings, helps with impulse control, may support recovery |
| ⚠️ Common Side Effects | Nausea, vomiting, fatigue, decreased desire/pleasure (e.g., food, sex, social activities) |
| 💰 Cost | Can be expensive; often not covered for addiction treatment |
📊 3. Personal Reflection
A. How much are cravings interfering with your recovery?
- ☐ A lot
- ☐ Somewhat
- ☐ Not much
B. Have you tried other treatments? (Check all that apply)
- ☐ Counseling/therapy
- ☐ Medication (e.g., naltrexone, buprenorphine)
- ☐ Peer support (e.g., 12-step, SMART Recovery)
- ☐ Lifestyle or spiritual changes
C. What matters most to you right now?
(Check your top 2–3 priorities)
- ☐ Reducing cravings
- ☐ Avoiding relapse
- ☐ Keeping emotions and motivation strong
- ☐ Avoiding side effects
- ☐ Losing weight
- ☐ Keeping costs low
- ☐ Feeling in control of my recovery
💬 4. Questions to Ask Your Provider or Peer Supporter
| Topic | Questions |
|---|---|
| Effectiveness | – How well does this medication work for my specific addiction? – What will success look like? |
| Side Effects | – How will it affect my mood, energy, and emotions? – Will it interfere with sex, appetite, or relationships? |
| Recovery Fit | – Will I still need therapy, support groups, or lifestyle changes? – Does this fit with my personal view of recovery? |
| Alternatives | – What are the other options? Have I tried them? – Should this be a first or last resort? |
| Access & Cost | – Is this covered by my insurance? – How long would I need to take it? – Can I afford it long-term? |
| Monitoring | – How often will I check in with you? – What will we track to see if it’s helping or hurting? |
⚖️ 5. Pros and Cons Chart
Fill this out with your provider or support team:
| Pros (Why I Might Want to Use It) | Cons (Why I Might Not Want to Use It) |
|---|---|
| e.g., Less craving, better control | e.g., Side effects, cost, emotional flatness |
📌 6. Decision Confidence Scale
How confident are you right now about trying a GLP-1 medication?
1 = Not at all confident | 5 = Very confident
☐ 1 ☐ 2 ☐ 3 ☐ 4 ☐ 5
If you’re below a 4, what would help you feel more confident?
- More info?
- More time?
- A second opinion?
- Talking to peers who’ve used it?
💡 7. Next Steps
✅ Schedule a follow-up discussion
✅ Ask about a trial period (e.g., 4–6 weeks)
✅ Track your experiences (energy, mood, cravings)
✅ Keep support systems active (therapy, peers, etc.)
In summary, GLP-1 medications may help you turn down the volume on cravings—but they won’t replace the work of healing. The best decision is one that feels right for your body, your mind, and your recovery path.
Question: From the provider’s point of view, which areas should the provider consider for GLP-1?
Answer: From a healthcare provider’s perspective, considering the use of GLP-1 receptor agonists (GLP-1RAs)—like semaglutide or liraglutide—for treating addiction involves a complex balance of clinical, ethical, and practical factors. Below is a breakdown of the key areas providers must evaluate:
🧠 1. Clinical Assessment
- Diagnosis clarity: Is the patient diagnosed with a DSM-5 substance use disorder (SUD)? What is the severity?
- Comorbidities: Does the patient have metabolic conditions (e.g., type 2 diabetes, obesity) that already indicate GLP-1 use?
- Addiction type: Evidence is strongest for alcohol use disorder (AUD), emerging for opioids, nicotine, and cannabis, but limited for stimulants.
- Treatment history: Have first-line, evidence-based treatments been tried (e.g., naltrexone for AUD, buprenorphine for OUD)?
⚖️ 2. Evidence Base
- Efficacy: Current evidence is preliminary but promising—mostly from observational studies and small trials.
- Lack of FDA approval: GLP-1s are not approved for the treatment of SUDs. Providers must carefully document the rationale for off-label use.
- Need for monitoring: Frequent follow-up is needed to track changes in cravings, mood, side effects, and weight.
🗣️ 3. Informed Consent & Communication
- Full disclosure: Patients must understand that:
- The drug is being used off-label.
- Side effects can include nausea, reduced pleasure, libido changes, or mood blunting.
- Patient autonomy: Ensure patients are involved in shared decision-making rather than being prescribed based on weight-loss trends or anecdotal success.
💊 4. Polypharmacy and Drug Interactions
- Caution with other meds: Consider interactions with psychiatric medications (e.g., antidepressants, antipsychotics) or other anti-craving meds.
- Overmedication risk: Patients in recovery are often prescribed multiple drugs. Avoid layering GLP-1 without a clear justification.
💰 5. Access, Coverage, and Cost
- Insurance limitations: Many payers do not cover GLP-1RAs for off-label uses like addiction. Out-of-pocket costs can exceed $1,000/month.
- Socioeconomic barriers: Marginalized populations with addiction may lack access unless cost assistance is arranged.
📉 6. Side Effects and Risks
- Common side effects: Nausea, vomiting, delayed gastric emptying, fatigue.
- Emotional changes: Some patients report emotional flatness, reduced motivation, or even anhedonia.
- Weight loss risk: Unintended weight loss in already undernourished or frail patients with addiction can be dangerous.
🌱 7. Recovery and Psychosocial Factors
- Integration with therapy: Medication should complement—not replace—counseling, peer support, or recovery models.
- Behavioral change support: Some patients may experience “craving suppression” without building coping skills, which may impair long-term recovery resilience.
📋 8. Documentation & Legal Considerations
- Clinical notes: Clearly document the rationale for off-label use, the patient’s understanding, and the monitoring plan.
- State/federal scrutiny: GLP-1 use in addiction could attract legal or audit questions if not justified clearly.
✅ Summary Checklist for Providers
| Area | Questions to Consider |
|---|---|
| Clinical | Is addiction diagnosis clear and severe? Tried other treatments first? |
| Evidence | Is there research support for this type of addiction? |
| Consent | Have I explained off-label use and risks fully? |
| Side Effects | Can the patient tolerate nausea, appetite loss, or mood changes? |
| Access | Can the patient afford or access the medication reliably? |
| Psychosocial | Is this integrated into a full recovery plan? |
| Documentation | Is this integrated into a complete recovery plan? |
In summary, providers must avoid overenthusiasm driven by media hype or weight loss trends. Instead, GLP-1 use in addiction should be guided by careful clinical judgment, ethical reflection, and patient-centered care.
Question: What is the latest research on GLP-1 Receptor Agonists and Addiction?
Answer: Recent research has highlighted the potential of GLP-1 receptor agonists (GLP-1RAs), such as semaglutide (Ozempic, Wegovy) and liraglutide (Saxenda), in treating various forms of addiction, including alcohol, nicotine, opioids, and stimulants.
🧪 Clinical Evidence in Humans
- Alcohol Use Disorder (AUD): A randomized controlled trial published in JAMA Psychiatry demonstrated that semaglutide significantly reduced alcohol cravings and consumption. Participants receiving the medication drank approximately 40% less alcohol compared to those on a placebo. People.com
- Comparative Effectiveness: A large-scale observational study involving over 228,000 individuals found that semaglutide and liraglutide were associated with a 21–22% reduction in alcohol-related hospitalizations. Notably, these reductions were more substantial than those observed with traditional AUD treatments like naltrexone and disulfiram. New York Post+2PMC+2JAMA Network+2
- Opioid Use Disorder (OUD): Research from Loyola University Chicago indicated that GLP-1RA users with OUD experienced a 40% lower rate of opioid overdose. Similarly, individuals with AUD saw a 50% reduction in alcohol intoxication events. Loyola Today+1The Pharmaceutical Journal+1
- Cannabis Use Disorder: Preliminary data suggest that semaglutide may reduce the incidence and relapse rates of cannabis use disorder, although further research is needed to confirm these findings. JAMA Network+1PMC+1
🧠 Mechanisms of Action
GLP-1RAs appear to influence addiction-related behaviors through several pathways:
- Dopamine Modulation: These agents may reduce the rewarding effects of addictive substances by modulating dopamine release in the brain’s reward centers. Newsroom+1The Pharmaceutical Journal+1
- Gut-Brain Axis: GLP-1RAs interact with the gut-brain axis, potentially affecting cravings and reward processing. PubMed
- Neuroinflammation Reduction: By decreasing neuroinflammation, GLP-1RAs might contribute to improved mental health outcomes, including reduced depressive symptoms. The Pharmaceutical Journal
⚠️ Considerations and Ongoing Research
- Side Effects: Common adverse effects include gastrointestinal symptoms, muscle loss, and emotional blunting. Some users report a general reduction in desires, affecting social interactions and intimacy. The Australian
- Need for Further Studies: While initial findings are promising, experts emphasize the necessity for more randomized controlled trials to establish causality, optimal dosing, and long-term safety. Newsroom
- Regulatory Status: Currently, GLP-1RAs are not FDA-approved for treating substance use disorders. Off-label use should be approached with caution until more definitive evidence is available.
In summary, GLP-1 receptor agonists show potential as novel treatments for various addictions, particularly alcohol use disorder. Their ability to modulate reward pathways and reduce cravings positions them as promising candidates in addiction medicine. However, comprehensive clinical trials are essential to fully understand their efficacy and safety profiles before they can be widely recommended for this purpose.
Conclusion
GLP-1 drugs present a promising avenue for treating addiction, particularly in addressing obesity and substance use disorders through their appetite-regulating effects. However, their use is not without challenges, including potential side effects, high costs, and ethical dilemmas surrounding access and informed consent. The successful integration of GLP-1 medications into treatment plans necessitates a holistic approach that encompasses self-management strategies, family support, and community resources. Empowering individuals to take control of their health through lifestyle changes while fostering a supportive environment can enhance recovery outcomes. Ultimately, addressing the multifaceted aspects of GLP-1 drugs in addiction treatment will be essential in ensuring equitable access and practical support, paving the way for improved long-term recovery for individuals facing these challenges.
Video: GLP-1 Side Effects You Should Know!