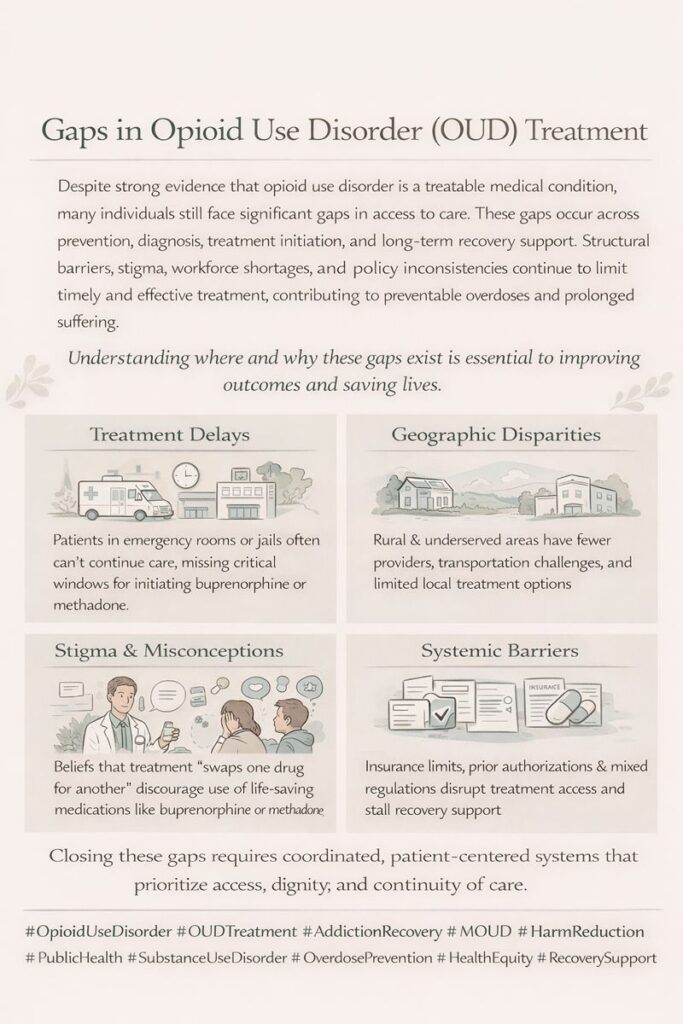
Opioid Use Disorder (OUD) treatments have gaps. Despite the effectiveness of Medication-Assisted Treatment (MAT) and behavioral therapies, barriers such as limited access, high costs, and stigma remain. Addressing these issues through social and government interventions is essential for better recovery outcomes.
“Addressing the Barriers to Accessing Opioid Use Disorder Treatments”
One of the most pressing issues in combating the opioid crisis is the limited access to effective treatments for Opioid Use Disorder (OUD). This challenge affects countless individuals, particularly those living in rural or underserved areas, where resources for addressing addiction are often scarce. Here’s a closer look at the barriers to accessing Medication-Assisted Treatment (MAT) and behavioral therapies, and the implications for those seeking help.
1. Geographic Barriers
Individuals in rural communities often face significant geographic barriers to accessing addiction treatment. Specialized addiction treatment facilities and providers are typically concentrated in urban areas, leaving rural residents with few options. This scarcity forces many to travel long distances—sometimes hundreds of miles—for care, which can be a significant barrier to treatment adherence. Travel logistics, including time, transportation costs, and the potential for lost income, can deter individuals from seeking the help they need.
2. Insurance and Cost Issues
The financial aspect of addiction treatment further complicates access to care. Many treatment options remain prohibitively expensive, and not all insurance plans cover comprehensive OUD treatment. High out-of-pocket costs can deter individuals from pursuing MAT and behavioral therapies, leading to untreated addiction and worsening health outcomes. This financial strain disproportionately affects low-income individuals and those without insurance, exacerbating existing inequalities in access to healthcare.
3. Limited Availability of Providers
Another significant barrier is the limited availability of healthcare providers trained in addiction treatment. Many primary care physicians may not be equipped to prescribe MAT or provide the necessary behavioral therapies, creating a care gap. Additionally, stigma surrounding addiction can prevent healthcare providers from adequately addressing these issues, further limiting access for individuals seeking help.
4. Lack of Awareness and Education
A lack of awareness about available treatment options also poses a challenge. Many individuals struggling with OUD may not know that MAT exists or how to access it. Educational campaigns and outreach efforts are crucial for informing communities about available resources and empowering individuals to seek treatment and support.
5. Cultural and Social Barriers
Cultural perceptions of addiction can create additional barriers to treatment. In some communities, stigma and negative attitudes toward those with substance use disorders may discourage individuals from seeking help. A culture that views addiction as a moral failing rather than a health issue can prevent individuals from accessing the support they need, leading to feelings of shame and isolation.
6. Potential Solutions
To address these barriers, a multifaceted approach is necessary. Expanding telehealth services can help bridge the gap for individuals in remote areas, providing them with access to specialized care without traveling. Policies that increase insurance coverage for MAT and behavioral therapies are essential to reducing financial barriers, while training more healthcare providers in addiction treatment can improve the availability of services.
Community outreach and education campaigns can raise awareness about seeking help for OUD. At the same time, efforts to reduce stigma can create a more supportive environment for those struggling with addiction. By fostering a culture of understanding and support, we can help individuals feel more comfortable seeking the treatment they need.
The limited access to OUD treatments remains a significant challenge in addressing the opioid crisis. Geographic barriers, insurance, cost issues, limited provider availability, and cultural perceptions contribute to this pressing problem. By implementing strategies to improve access to care, we can enhance treatment outcomes for individuals with OUD and support their journey toward recovery. Ultimately, addressing these barriers is not only a matter of health equity but also a crucial step in combating the ongoing opioid epidemic.
“Breaking Down the Barriers: Addressing the Stigma Surrounding Addiction and Treatment”
The stigma surrounding addiction and its treatment poses a significant barrier for individuals seeking help for Opioid Use Disorder (OUD). This pervasive issue not only deters people from seeking support but also exacerbates the challenges they face. Understanding the roots and impacts of stigma is crucial for fostering a more compassionate and practical approach to addiction treatment.
1. Understanding Stigma
Stigma can be defined as a mark of disgrace associated with a particular circumstance, quality, or person. In the context of addiction, both societal and institutional stigma contribute to negative perceptions and discrimination against individuals struggling with substance use disorders. These attitudes often stem from misunderstandings about addiction, viewing it as a moral failing rather than a complex health issue influenced by various factors, including genetics, environment, and mental health.
2. The Impact of Societal Stigma
Societal stigma manifests in various ways, leading to feelings of shame and isolation among those with OUD. Individuals may fear judgment from friends, family, and colleagues, preventing them from seeking help. This fear of negative perception often results in people suffering in silence, leading to a worsening of their condition. Isolation can further complicate their recovery journey, making it difficult for them to connect with support networks that are essential for healing.
3. Institutional Stigma in Healthcare Settings
Stigma also permeates healthcare systems, where individuals may encounter judgmental attitudes from providers. Discrimination in healthcare settings can severely impact the quality of care received, discouraging patients from being open about their struggles with addiction. This lack of trust may lead individuals to avoid seeking treatment altogether or result in suboptimal care, further perpetuating the cycle of addiction.
4. Consequences of Stigma
The consequences of stigma are profound. Beyond the immediate impact on individuals’ willingness to seek help, stigma can lead to systemic barriers within the healthcare system. Providers who harbor stigmatizing attitudes may be less likely to refer patients to necessary treatment options or to provide compassionate care. This creates a cycle where individuals with OUD are left without the support they need to recover.
5. Addressing Stigma Through Education and Advocacy
Breaking down the barriers of stigma requires a concerted effort focused on education and advocacy. Public awareness campaigns can challenge misconceptions about addiction, highlighting the complexities of substance use disorders and promoting understanding and compassion. Training healthcare providers to recognize and confront their biases can improve the quality of care and foster a more supportive environment for individuals seeking help.
6. Creating Supportive Communities
Community support plays a critical role in combating stigma. Initiatives that promote open dialogue about addiction can help normalize the conversation around OUD, making it easier for individuals to seek assistance. Peer support programs and community engagement activities can empower those affected by addiction to share their experiences, fostering a sense of belonging and connection.
The stigma surrounding addiction and treatment significantly hinders individuals’ ability to seek help and access the care they need. By addressing societal and institutional stigma, we can create a more supportive environment for those with Opioid Use Disorder. Through education, advocacy, and community engagement, we can dismantle the barriers that prevent individuals from pursuing recovery, ultimately contributing to more effective treatment outcomes and a healthier society. Breaking the stigma is not just a moral imperative; it is a necessary step toward healing individuals and communities affected by addiction.
“The Importance of Integrated Care Models in Treating Opioid Use Disorder”
The treatment landscape for Opioid Use Disorder (OUD) is fraught with challenges, primarily characterized by inconsistencies in the availability of evidence-based treatments and the quality of care provided. As the opioid crisis continues to impact communities nationwide, addressing these inconsistencies is crucial for improving treatment outcomes and supporting individuals on their recovery journeys.
1. Inconsistent Availability of Evidence-Based Treatments
Despite the proven efficacy of evidence-based treatments such as Medication-Assisted Treatment (MAT) and behavioral therapies, access to these options can be inconsistent. Geographic disparities often leave rural and underserved populations with limited access to effective treatments. Moreover, the quality of available services varies widely, with some facilities providing comprehensive care while others may offer subpar options lacking essential components of effective treatment.
2. Fragmented Care Systems
The current healthcare system often operates in silos, with different types of care—such as medical, psychological, and social support—functioning independently. This fragmentation can result in disjointed care experiences, where individuals with OUD may receive treatment from various providers without coordinated support. This lack of integration makes it challenging to address the multifaceted nature of addiction, which often involves intertwined physical, mental, and social health issues.
3. The Need for Integrated Care Models
Integrated care models that combine medical, psychological, and social support are essential for effective OUD treatment. These models foster collaboration among healthcare providers, ensuring that individuals receive comprehensive and continuous care tailored to their needs. For example, a patient receiving MAT should also have access to behavioral therapies, mental health support, and social services to address underlying issues such as trauma or housing instability.
4. Enhancing Provider Training
Healthcare professionals need extensive training in managing OUD to implement effective integrated care models. Many providers lack the necessary knowledge and skills to treat addiction effectively, which can lead to hesitation in addressing these issues or employing evidence-based practices. Comprehensive training programs should include education on the complexities of OUD, strategies for integrating care, and effective communication with individuals seeking help.
5. Overcoming Barriers to Integration
Several barriers hinder the implementation of integrated care models. These include financial constraints, providers’ limited awareness of integration’s benefits, and resistance to change within established healthcare systems. Advocating for policy changes that support integrated care initiatives, increasing funding for comprehensive treatment programs, and promoting collaboration between healthcare providers are crucial steps toward overcoming these barriers.
6. Improving Patient Outcomes
By addressing the inconsistencies in the availability of evidence-based treatments and promoting integrated care models, we can significantly improve patient outcomes for individuals with OUD. Coordinated care that addresses all aspects of a person’s health can lead to better recovery rates, reduced relapse, and enhanced overall well-being.
The current state of OUD treatment highlights the urgent need for a paradigm shift toward integrated care models that provide comprehensive support to individuals seeking help. By fostering collaboration among providers, enhancing training, and advocating for systemic changes, we can create a more effective and equitable treatment landscape for those affected by Opioid Use Disorder. Integrating care not only addresses the complexities of addiction but also empowers individuals on their path to recovery, ensuring they receive the holistic support necessary for lasting change.
“Personalizing Opioid Use Disorder Treatment for Enhanced Efficacy”
Tailoring treatments to meet the unique needs of individuals with Opioid Use Disorder (OUD) is paramount for improving efficacy and fostering successful recovery outcomes. OUD is a heterogeneous condition characterized by a variety of underlying factors that influence an individual’s experience with addiction. Therefore, personalized treatment approaches are essential in addressing the complexities of this disorder.
1. Understanding the Heterogeneity of OUD
OUD manifests differently in each person, influenced by various factors such as genetics, psychological health, environmental circumstances, and social support systems. This variability means that a one-size-fits-all treatment approach often falls short. Recognizing these differences allows for the development of tailored interventions that resonate with the individual’s needs and circumstances.
2. Personalized Treatment Approaches
Implementing personalized treatment plans involves several key components:
- Genetic Considerations: Genetic predispositions can affect how individuals metabolize medications and their susceptibility to addiction. Genetic testing can provide insights into which medications are most effective and which carry a higher risk of adverse effects.
- Addressing Co-occurring Disorders: Many individuals with OUD also struggle with mental health disorders such as depression, anxiety, or PTSD. Acknowledging and treating these co-occurring conditions concurrently can improve overall treatment efficacy. Integrated care that combines substance use and mental health treatment is vital for this population.
- Personal Circumstances: Socioeconomic status, living situation, and support networks are crucial in recovery. Personalized treatment plans should consider these elements to create a comprehensive approach that supports the individual’s unique situation.
3. Cultural Sensitivity and Inclusivity
Culturally sensitive treatment approaches that respect and incorporate individuals’ diverse backgrounds can significantly enhance engagement and effectiveness. Understanding cultural attitudes toward addiction, stigma, and treatment can foster trust and improve communication between patients and providers. This sensitivity fosters a more inclusive treatment environment in which individuals feel valued and understood, leading to higher participation rates in treatment programs.
4. Engagement in Treatment
When individuals see that their treatment plans are tailored to their specific needs, they are more likely to engage actively. Personalized care fosters a sense of ownership over one’s recovery journey, motivating individuals to adhere to treatment protocols and actively participate in therapeutic activities. Moreover, involving patients in treatment decision-making enhances their commitment and accountability.
5. Monitoring and Adjusting Treatment Plans
Personalized treatment is not static; it requires ongoing assessment and adjustment. Regular progress monitoring, including patient feedback and clinical evaluations, ensures that treatment remains relevant and practical. As circumstances change, the treatment plan can be adapted to address emerging challenges or shifts in the individual’s health status.
6. Collaborative Care Models
Implementing personalized treatment approaches necessitates a collaborative care model involving multidisciplinary teams, including physicians, therapists, social workers, and peer support specialists. This collaboration ensures a holistic approach considering all aspects of an individual’s health and well-being.
Tailoring OUD treatments to individual needs is crucial for improving efficacy and supporting lasting recovery. By embracing personalized treatment approaches that account for genetic, psychological, and sociocultural factors, healthcare providers can better meet the diverse needs of individuals struggling with addiction. Creating a responsive and inclusive treatment environment enhances engagement and promotes healthier, more sustainable recovery outcomes. Through collaboration, ongoing assessment, and cultural sensitivity, we can make significant strides in effectively addressing the complexities of Opioid Use Disorder.
“Bridging the Gaps in Opioid Use Disorder Treatment: A Comprehensive Approach”
Bridging the gaps in Opioid Use Disorder (OUD) treatment requires a multifaceted approach that addresses the diverse barriers faced by individuals seeking help. As the opioid crisis continues to evolve, it becomes increasingly crucial to implement strategies that expand access, reduce stigma, enhance treatment integration, and personalize care.
1. Expanding Access to Treatment
One of the primary barriers to effective OUD treatment is limited access, particularly for individuals in rural or underserved areas. Expanding access through telemedicine can help overcome geographic challenges by allowing patients to connect with healthcare providers remotely. This approach improves availability and offers flexibility for those who may have difficulty attending in-person appointments. Additionally, advocating for policy changes that reduce treatment costs can make comprehensive care more accessible. Lowering the financial burden on patients will encourage more individuals to seek the help they need.
2. Combating Stigma
The stigma surrounding addiction remains a significant obstacle that deters individuals from seeking treatment. Public education campaigns aimed at raising awareness about OUD can help dismantle misconceptions and foster a more compassionate understanding of addiction. Training healthcare providers to approach patients empathetically and without judgment is also essential. Creating a supportive environment can encourage more individuals to reach out for help.
3. Enhancing Treatment Integration
Integrating care for OUD with other medical and mental health services is vital for improving treatment outcomes. Developing and implementing integrated care models that facilitate collaboration among various healthcare providers can ensure that individuals receive comprehensive support. By fostering teamwork among physicians, therapists, social workers, and peer support specialists, we can address the multifaceted needs of individuals with OUD, leading to better health outcomes.
4. Personalizing Treatment Approaches
Personalized treatment is critical to addressing the unique needs of individuals with OUD. Utilizing genetic and clinical data allows providers to tailor treatment plans that are more effective for each patient. Furthermore, ensuring cultural competence in treatment approaches can enhance engagement and outcomes, as patients are more likely to adhere to programs that respect and understand their backgrounds.
5. Community-Based Support
Community interventions play a critical role in bridging the gaps in OUD treatment. Establishing community-based peer support programs can provide individuals with a sense of belonging and connection, encouraging them to seek available resources. Local outreach initiatives can help raise awareness of treatment options and services, fostering a supportive community environment.
6. Addressing Economic and Social Factors
Broad social and government interventions are essential for improving the chances of recovery. Economic and social support, such as stable housing and job opportunities, significantly impact an individual’s ability to maintain recovery and reduce the risk of relapse. By addressing these underlying social determinants of health, we can create a more conducive environment for individuals on their recovery journey.
Bridging the gaps in OUD treatment requires a holistic, collaborative approach that encompasses individual, community, and systemic efforts. By expanding access through telemedicine, combating stigma, enhancing treatment integration, personalizing care, fostering community support, and addressing economic factors, we can create a more effective and compassionate system for individuals struggling with OUD. Together, we can build a supportive framework that empowers individuals to seek help, engage in treatment, and achieve lasting recovery.
“The Essential Role of Government Interventions in Opioid Use Disorder Recovery”
Government interventions are vital for creating a supportive environment that fosters recovery from Opioid Use Disorder (OUD). With the ongoing opioid crisis affecting millions, legislative measures, regulatory oversight, public health initiatives, and investment in research and innovation are essential to ensure effective treatment and support for those in need.
1. Legislative Efforts to Improve Access
One primary way the government can assist in OUD recovery is through legislation that expands access to treatment. Policies to remove barriers to Medication-Assisted Treatment (MAT) and behavioral therapies are crucial. This includes provisions to increase the number of treatment facilities, simplify insurance processes, and ensure that treatment options are available in underserved areas. Governments can help more individuals receive the care they require by prioritizing access.
2. Support for Harm Reduction Strategies
Harm reduction strategies are critical components of a comprehensive approach to managing OUD. Legislative support for initiatives such as needle exchange programs, supervised consumption sites, and naloxone distribution can save lives and reduce the risks associated with substance use. By funding and promoting these programs, governments can contribute to minimizing the health consequences of addiction while encouraging individuals to seek more comprehensive treatment.
3. Regulatory Oversight for Quality Care
Regulatory oversight is necessary to ensure that OUD treatments maintain high standards of quality and accessibility. Governments should establish and enforce regulations that hold treatment facilities accountable for their practices. This includes regular inspections, transparency in operations, and mechanisms for reporting and addressing complaints. Ensuring all patients have access to safe and effective treatment can help prevent disparities arising from poor-quality care.
4. Integration into Public Health Initiatives
Integrating OUD treatment and prevention into broader public health initiatives can enhance the visibility and effectiveness of these programs. Governments should work to include OUD strategies within existing healthcare frameworks, ensuring that they receive adequate attention and resources. This holistic approach not only addresses addiction directly but also tackles associated issues such as mental health, housing, and employment, promoting overall community well-being.
5. Investment in Research and Innovation
Investment in research is crucial for the ongoing advancement of OUD treatment options. Governments should prioritize funding research into new therapies, treatment models, and prevention strategies. This investment can drive innovation in the field, leading to more effective and personalized approaches to managing OUD. Additionally, research into the social determinants of health can help identify barriers to treatment and inform policy decisions.
Government interventions are essential in shaping a supportive environment for recovery from Opioid Use Disorder. Through legislative efforts to improve access to treatment, support harm reduction strategies, ensure regulatory oversight of quality care, integrate OUD into public health initiatives, and invest in research, governments can significantly advance the fight against OUD. By adopting a comprehensive approach that prioritizes the needs of individuals struggling with addiction, we can foster a society that supports recovery and promotes health for all. Together, we can make strides toward addressing the opioid crisis and its devastating effects on communities.
Frequently Asked Questions
Here are some common questions:
Why do many people with OUD not receive treatment?
Common reasons include stigma, lack of trained providers, long wait times, insurance barriers, transportation issues, fear of judgment, and limited awareness that OUD is a treatable medical condition.
What is the most critical gap in OUD care?
Failure to start or continue MOUD is one of the most dangerous gaps. Delays or interruptions in medications like buprenorphine or methadone significantly increase overdose risk, especially after detox, incarceration, or hospitalization.
How do geographic factors affect OUD treatment access?
Rural and underserved areas often have fewer clinics, pharmacies, and prescribers. Long travel distances, limited public transportation, and workforce shortages make consistent treatment difficult.
How does stigma create treatment gaps?
Stigma can discourage people from seeking care and providers from offering MOUD. Misbeliefs that medications “replace one addiction with another” reduce the use of lifesaving treatments and isolate patients.
What role do insurance and policy barriers play?
Prior authorizations, dosage limits, step therapy, and inconsistent state regulations delay treatment initiation and disrupt continuity, even when clinical need is clear.
Conclusion
Addressing the gaps in OUD treatments requires a comprehensive approach that includes expanding access, combating stigma, enhancing treatment integration, and personalizing care. Social, societal, and government interventions are crucial in creating a supportive environment for individuals with OUD. By combining these efforts, we can bridge the gaps in treatment and work towards a more effective and equitable approach to managing Opioid Use Disorder, ultimately improving outcomes for those affected by this challenging condition.
Video: Gaps in Opioid Use Disorder OUD Treatment