Addiction recovery often involves managing intense physical and emotional symptoms that can interfere with treatment engagement. Alongside counseling and primary addiction medications, supportive therapies are sometimes used to ease withdrawal discomfort, anxiety, and sleep disruption. Gabapentin, originally developed for seizure and nerve pain treatment, has emerged as an adjunct medication in addiction therapy for its calming effects on the nervous system. While it does not treat addiction directly, gabapentin can help stabilize early recovery by reducing distress that often leads to relapse. When prescribed and monitored appropriately, it serves as a valuable support tool within comprehensive, evidence-based addiction care.
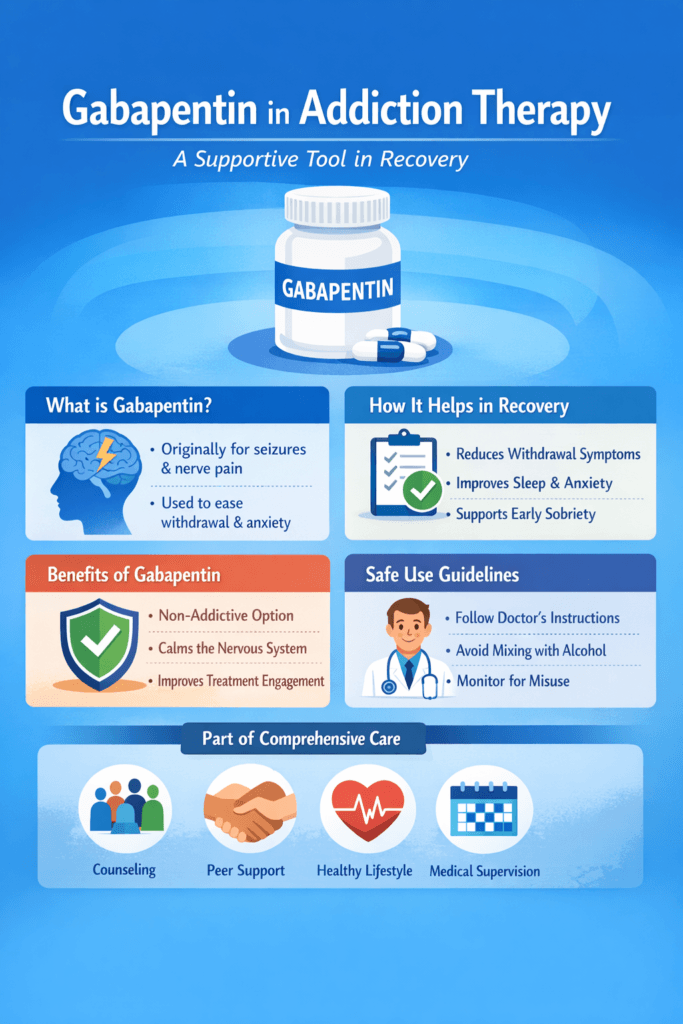
Gabapentin in Addiction Therapy: A Supportive Tool in Recovery
Addiction treatment has evolved beyond detox and abstinence alone. Modern recovery care now integrates medications that ease withdrawal, stabilize mood, and improve treatment retention. One medication gaining attention in addiction therapy is gabapentin. Originally developed to treat seizures and nerve pain, gabapentin is increasingly used as an adjunct medication in substance use disorder treatment. While not a primary addiction medication, it plays a supportive role in reducing withdrawal discomfort, anxiety, insomnia, and relapse risk when used appropriately under medical supervision.
Gabapentin’s Role in Addiction Treatment
Gabapentin works by modulating calcium channels in the nervous system, helping calm overactive neural signaling. In addiction recovery, this calming effect can be valuable during early abstinence, when the brain is adjusting to the absence of substances.
Clinicians most commonly use gabapentin in alcohol use disorder, where it helps reduce withdrawal symptoms such as tremors, agitation, and sleep disruption. It has also shown benefits in decreasing alcohol cravings and improving post-detox stabilization. In opioid withdrawal, gabapentin may ease muscle aches, restlessness, anxiety, and insomnia, making the detox process more tolerable. Some providers also use it to support individuals recovering from cannabis or stimulant dependence, particularly when anxiety or sleep problems interfere with recovery progress.
Benefits of Recovery Support
One of gabapentin’s key advantages is its non-opioid, non-sedating nature at therapeutic doses, making it a safer supportive medication compared to benzodiazepines. By improving sleep quality and reducing anxiety, gabapentin helps individuals stay engaged in counseling, peer support, and behavioral therapy. Better comfort during early recovery is often associated with lower dropout rates and improved treatment adherence.
Additionally, gabapentin may help stabilize co-occurring conditions such as chronic pain, neuropathy, or restless leg syndrome — all of which can trigger relapse if left untreated.
Risks and Responsible Use
Despite its benefits, gabapentin is not risk-free. Misuse potential has been reported, especially among individuals with opioid use disorder. For this reason, careful dosing, prescription monitoring, and medical oversight are essential. Gabapentin should always be part of a comprehensive treatment plan, not a standalone solution.
The Future of Supportive Medications in Addiction Care
As addiction medicine continues shifting toward whole-person, precision-based care, medications like gabapentin fill an important supportive niche. When combined with counseling, peer recovery services, lifestyle stabilization, and evidence-based addiction medications, gabapentin can improve comfort, engagement, and long-term recovery outcomes.
Conclusion
Gabapentin is not a cure for addiction, but it is a valuable recovery support tool. By easing withdrawal symptoms, improving sleep, and reducing anxiety, it helps individuals remain focused on healing rather than discomfort. With proper medical supervision, gabapentin contributes to a more compassionate, effective, and patient-centered approach to addiction treatment.
Self-Management When Using Gabapentin in Addiction Therapy
Recovery from substance use disorder requires more than willpower alone. Many individuals benefit from supportive medications that reduce withdrawal discomfort, stabilize mood, and improve sleep. Gabapentin is one such medication increasingly used as an adjunct in addiction therapy. However, because gabapentin can affect the nervous system and carries some misuse potential, successful outcomes depend heavily on self-management practices. Learning how to use gabapentin responsibly within a recovery plan empowers individuals to stay safe, engaged in treatment, and focused on long-term healing.
Understanding Gabapentin’s Purpose in Recovery
Gabapentin is not a primary addiction treatment medication. Instead, it serves as a supportive therapy to reduce symptoms that commonly trigger relapse — anxiety, insomnia, restlessness, irritability, and physical discomfort during withdrawal. When individuals understand that gabapentin’s role is symptom support rather than emotional escape, they are more likely to use it appropriately and avoid dependence.
Self-management begins with recognizing that medication is most effective when combined with counseling, peer support, and healthy daily routines.
Key Self-Management Strategies
Follow prescribed dosing exactly. Taking more gabapentin than prescribed does not speed recovery and increases side effects and misuse risks. Consistency matters more than quantity.
Track symptom changes. Keeping a simple journal of sleep quality, anxiety levels, cravings, and side effects helps healthcare providers adjust treatment safely.
Avoid mixing with alcohol or sedatives. Combining gabapentin with other depressants can cause dangerous breathing and coordination problems.
Build non-medication coping tools. Mindfulness, exercise, structured routines, hydration, and nutrition reduce reliance on medication alone for comfort.
Store medication safely. Keeping gabapentin in a secure place prevents accidental misuse by others and reinforces responsible personal use.
Communicate honestly with providers. Reporting cravings to misuse medication, side effects, or emotional changes allows early intervention before problems escalate.
Preventing Misuse and Dependence
Because gabapentin can produce calming or euphoric effects at high doses, individuals in recovery must remain aware of personal vulnerability to medication misuse. Self-awareness, accountability partners, pill organizers, and regular prescription check-ins help maintain safe boundaries. Viewing gabapentin as a temporary recovery aid rather than a long-term solution supports healthier treatment expectations.
Supporting Whole-Person Recovery
Self-management means recognizing that medication is only one part of healing. Therapy, peer recovery meetings, trauma support, housing stability, and stress management all influence long-term success. When individuals actively participate in their care plan, they strengthen confidence, autonomy, and resilience.
Conclusion
Gabapentin can ease the physical and emotional strain of early recovery, but its success depends on responsible self-management. By following medical guidance, practicing healthy coping strategies, and staying accountable, individuals can use gabapentin safely while building a strong foundation for lifelong recovery. Empowered self-management turns supportive medication into a stepping stone — not a substitute — for true healing.
Family Support Strategies When Using Gabapentin in Addiction Therapy
Addiction recovery is rarely a solo journey. Family involvement often determines whether treatment plans succeed or fall apart. When a loved one is prescribed gabapentin as part of addiction therapy, families play an important role in supporting safe medication use, emotional stability, and long-term recovery progress. Because gabapentin is a supportive medication — not a cure — families who understand its purpose can help reinforce healthy routines, accountability, and hope throughout the recovery process.
Understanding Gabapentin’s Role
Gabapentin is commonly used in addiction care to reduce withdrawal discomfort, anxiety, sleep disruption, and restlessness. It does not treat addiction directly but helps stabilize symptoms that might otherwise trigger relapse. Families who understand this distinction are better prepared to offer encouragement without viewing medication as a complete solution or, conversely, as a weakness.
Learning basic information about the medication builds trust and reduces fear or misunderstanding.
Creating a Safe Medication Environment
Families can support responsible gabapentin use by helping establish safe routines. This may include encouraging consistent dosing schedules, using pill organizers, or setting reminder alarms. Secure storage of medications prevents accidental or intentional misuse by household members. Families should also remain aware of potential side effects, such as dizziness, fatigue, or mood changes, and report any concerns to healthcare providers as needed.
Encouraging Accountability Without Control
Supportive involvement is most effective when families practice accountability rather than surveillance. Asking open, nonjudgmental questions about how the medication is working encourages honest communication. Offering transportation to appointments, helping track refills, or attending family education sessions reinforces partnership in recovery rather than policing behavior.
Promoting Non-Medication Coping Skills
Families can strengthen recovery by helping loved ones build daily structure and emotional balance beyond medication. Shared meals, regular sleep schedules, exercise, and relaxation activities improve physical stability. Encouraging participation in therapy, peer support groups, or spiritual communities provides additional emotional grounding that medication alone cannot offer.
Watching for Misuse Warning Signs
Although gabapentin is generally safe when prescribed appropriately, misuse can occur. Families should watch for red flags such as taking higher doses than prescribed, frequent early refill requests, excessive sedation, or secretive medication behavior. Early, compassionate conversations and provider involvement can prevent escalation.
Supporting Emotional Healing
Addiction often damages family trust. Recovery is a time for rebuilding relationships through patience, honesty, and consistent support. Celebrating progress, acknowledging setbacks without shame, and participating in family counseling fosters healing on both sides.
Conclusion
When gabapentin is part of addiction therapy, family support becomes a powerful stabilizing force. By understanding the medication’s purpose, encouraging safe routines, promoting open communication, and supporting whole-person recovery, families help transform medication assistance into meaningful, lasting change. Recovery grows stronger when no one has to walk the path alone.
Community Resource Strategies for Using Gabapentin in Addiction Therapy
Successful addiction recovery depends on more than medical treatment alone. Community-based resources provide structure, connection, and real-world support that help individuals stay engaged in care. When gabapentin is used as a supportive medication in addiction therapy, community resources play an essential role in reinforcing safe medication use, reducing relapse risk, and promoting long-term stability. A recovery-friendly community turns clinical treatment into sustainable daily living.
Understanding Gabapentin’s Supportive Role
Gabapentin is often prescribed to reduce withdrawal discomfort, anxiety, sleep disruption, and restlessness during recovery. While helpful, it is not a stand-alone addiction treatment. Community education programs, recovery centers, and peer groups help individuals understand that medication is one tool among many in a broader recovery plan. When communities normalize evidence-based treatment, stigma decreases, and treatment participation improves.
Peer Recovery Support Programs
Peer recovery organizations provide mentorship, accountability, and shared lived experience. Individuals using gabapentin in treatment benefit from peer groups that reinforce healthy medication routines, coping strategies, and honest discussion about challenges. Peer specialists can also help individuals navigate healthcare systems, refill schedules, and treatment appointments.
Community Health Clinics and Integrated Care
Local health centers and addiction clinics offering integrated medical and behavioral care ensure gabapentin is prescribed and monitored safely. These centers provide medication management, counseling, case management, and mental health services in one setting. Easy access to providers reduces gaps in care that often lead to relapse.
Recovery Housing and Supportive Living
Stable housing is one of the strongest predictors of recovery success. Recovery residences and sober-living environments provide structured routines, medication accountability, and supportive peer environments. These settings reduce exposure to triggers and reinforce consistent self-care practices.
Educational Workshops and Family Programs
Community organizations frequently offer workshops on medication safety, relapse prevention, stress management, and family recovery education. These programs help individuals and families understand gabapentin’s purpose, recognize misuse risks, and build collaborative recovery plans.
Employment, Transportation, and Social Services
Community workforce programs, transportation services, and social support agencies reduce practical barriers to treatment adherence. Reliable access to appointments and a stable income reduce stress and improve medication adherence.
Reducing Stigma Through Public Awareness
Community awareness campaigns that promote addiction as a medical condition encourage individuals to seek treatment without shame. When medication-assisted recovery is accepted publicly, individuals feel safer following prescribed treatment plans.
Conclusion
Gabapentin can ease withdrawal and stabilize early recovery, but community resources transform short-term symptom relief into long-term healing. Through peer support, integrated healthcare, stable housing, education, and stigma-free environments, communities strengthen the effectiveness of medication-supported recovery. Healing grows strongest when medical care and community support work together.
Frequently Asked Questions
Here are some common questions:
What is gabapentin, and why is it used in addiction therapy?
Gabapentin is a medication originally developed for seizures and nerve pain. In addiction therapy, it is used as a supportive medication to reduce withdrawal symptoms, anxiety, restlessness, and sleep disturbances that can interfere with recovery.
Does gabapentin treat addiction directly?
No. Gabapentin does not cure addiction or replace primary addiction medications. It helps manage uncomfortable symptoms that may trigger relapse, making it easier to stay engaged in treatment.
Which substance use disorders commonly use gabapentin as support?
Gabapentin is most commonly used in alcohol use disorder and opioid withdrawal support. It may also help with anxiety and sleep problems in cannabis or stimulant recovery.
How does gabapentin help during withdrawal?
Gabapentin calms overactive nerve signaling in the brain. This reduces physical discomfort, muscle tension, irritability, anxiety, and insomnia often experienced during early recovery.
Is gabapentin addictive?
Gabapentin is not considered a primary addictive substance, but misuse can occur, especially in individuals with a history of substance use disorder. Medical monitoring and proper dosing reduce this risk.
Can gabapentin be taken with other addiction medications?
Yes. Gabapentin is often used alongside medications like buprenorphine, methadone, or naltrexone when prescribed by a healthcare provider.
What are the common side effects?
Common side effects include drowsiness, dizziness, fatigue, and coordination issues. Most side effects improve with dose adjustment under medical supervision.
Can gabapentin be taken with alcohol?
No. Mixing gabapentin with alcohol or other sedatives increases the risk of dangerous breathing problems and should be avoided.
How long has gabapentin used in addiction therapy?
Duration varies by individual needs. Some use it short-term during withdrawal, while others may use it longer for ongoing symptom management under provider guidance.
What signs suggest gabapentin misuse?
Warning signs include taking higher doses than prescribed, running out of medication early, excessive sedation, or seeking prescriptions from multiple providers.
How can families support someone using gabapentin in recovery?
Families can encourage adherence to medication regimens, safe storage, open communication, and participation in therapy and support groups.
Do I still need therapy if I take gabapentin?
Yes. Medication is most effective when combined with counseling, behavioral therapy, and peer recovery support.
Is gabapentin safe for everyone?
Gabapentin is generally safe when prescribed properly, but people with kidney problems or certain medical conditions require dose adjustments.
What should I do if I feel cravings to misuse gabapentin?
Tell your healthcare provider immediately. Honest communication helps adjust treatment and prevents relapse.
Can gabapentin improve sleep in recovery?
Yes. Many individuals experience improved sleep quality, which supports emotional stability and relapse prevention.
Is gabapentin part of evidence-based addiction care?
Yes. While not a primary addiction medication, it is recognized as a helpful adjunct in evidence-based, whole-person recovery plans.
Conclusion
Gabapentin is not a cure for substance use disorder, but it can play a meaningful role in improving comfort and stability during recovery. Easing withdrawal symptoms, reducing anxiety, and supporting better sleep help individuals stay engaged in therapy and daily recovery routines. Its effectiveness depends on responsible medical oversight and integration with behavioral treatment, peer support, and lifestyle change. When used appropriately, gabapentin contributes to a compassionate, whole-person approach that strengthens the foundation for long-term recovery.
Video: Does Gabapentin Actually Help With Addiction Recovery #addiction #recovery