Withdrawal motivation during forced addiction treatment is influenced by social support, addiction severity, and stress perception. Strong social support can ease distress and boost engagement, while severe addiction and high stress levels often reduce motivation and increase resistance. Understanding these factors is key to providing humane, person-centered care that supports long-term recovery, even in compulsory settings.
Motivation to Withdraw from Drugs in Compulsory Settings: The Interplay of Social Support, Stress, and Addiction Severity
Understanding What Drives Motivation During Forced Drug Withdrawal
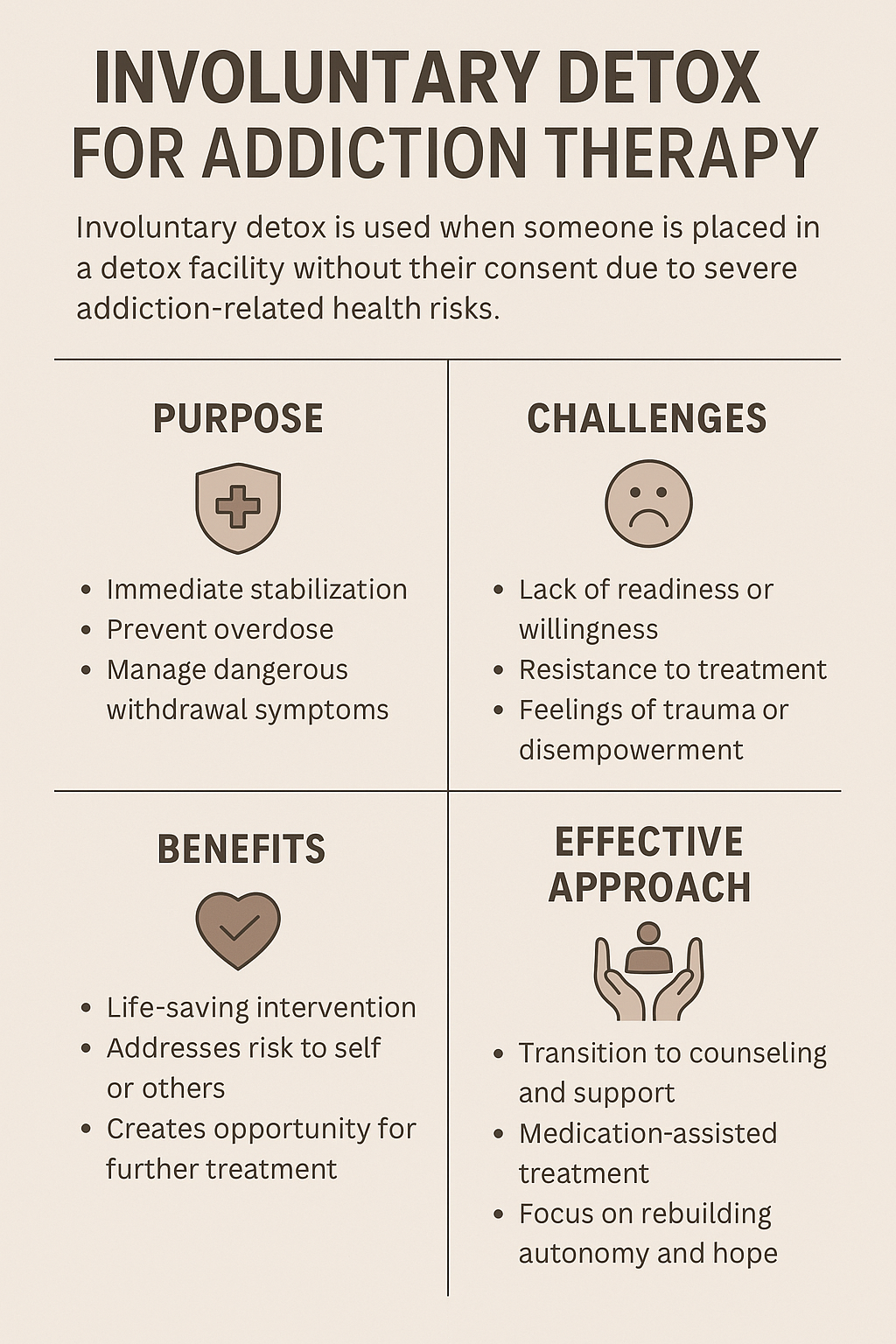
In rehabilitation centers, prisons, or court-mandated programs, many individuals face compulsory withdrawal—a situation where drug cessation isn’t voluntary. This raises a critical question: What influences their motivation to stay off drugs when choice is removed from the equation?
Emerging research reveals a complex relationship between social support, addiction severity, and perceived stress that profoundly impacts motivation. Here’s a closer look.
🔍 Key Factors Shaping Motivation in Compulsory Drug Withdrawal
1. Social Support
Support from family, peers, or professionals can:
- Improve emotional resilience
- Foster hope for recovery
- Increase adherence to treatment
On the flip side, lack of support or stigmatizing environments often lead to emotional isolation, resistance, and reduced motivation.
2. Addiction Severity
Those with more severe substance use (longer duration, more frequent use, or polydrug patterns) tend to experience:
- More intense cravings
- Lower intrinsic motivation to stop using
- Worse withdrawal symptoms, both physical and mental
3. Stress Perception
Forced withdrawal frequently heightens stress due to:
- Loss of control over daily life
- Anticipation of painful withdrawal
- Strict institutional rules
When stress is perceived as unmanageable, it diminishes the ability to cope and lowers the drive to remain abstinent.
🔄 How Addiction Severity and Stress Mediate Motivation
Interestingly, social support doesn’t directly boost motivation—it works through mediators like stress and addiction level.
| Effect of Social Support on Motivation | Effect on Social Support’s Impact on Motivation |
|---|---|
| Addiction Level | High severity blunts the benefits of support |
| Stress Perception | High stress cancels out motivation gains from support |
In other words, even the best support system can fall short if stress is unmanaged or addiction is too severe.
🔧 Improving Compulsory Withdrawal Programs: Practical Implications
To create more humane and effective systems for compulsory drug withdrawal, interventions must account for this complex interplay:
- Embed Social Support Throughout Programs
- Train staff in empathetic communication
- Offer peer mentorship and family involvement
- Reduce institutional stigma
- Assess and Address Addiction Severity Early
- Use tools like the ASI or DSM-5 criteria
- Match treatment intensity to addiction complexity
- Provide psychiatric and medication support when needed
- Implement Stress-Reduction Strategies
- Cognitive Behavioral Therapy (CBT)
- Mindfulness and breathing techniques
- Group therapy and structured routines
- Adopt a Dynamic View of Motivation
- Understand that motivation fluctuates daily
- Create flexible environments where people feel safe to grow
- Reinforce small wins and progress over time
In summary, motivation to withdraw from drugs during compulsory treatment isn’t just about willpower—it’s about support, stress, and addiction biology. Programs that integrate these elements into their design stand a better chance of fostering real, lasting recovery.
By treating people as dynamic individuals rather than passive subjects, we can build a more compassionate and practical approach to forced withdrawal—and ultimately, to addiction treatment as a whole.
How Social Support Transforms Forced Drug Withdrawal into a Path Toward Recovery
Social support plays a vital role in improving outcomes during forced drug addiction withdrawal, such as in court-mandated rehab, incarceration-based treatment, or compulsory detox programs. It does so by influencing emotional resilience, motivation to change, and engagement in long-term recovery. Here’s how:
✅ 1. Reduces Psychological Distress
- Forced withdrawal often increases anxiety, fear, and resistance due to a lack of choice or autonomy.
- Support from family, peers, or professionals helps buffer this emotional strain by offering empathy, reassurance, and validation.
✅ 2. Improves Motivation for Change
- People with strong social support are more likely to shift from external (forced) to internal motivation for recovery.
- Encouragement from loved ones or peer role models can make abstinence feel meaningful—not just imposed.
✅ 3. Buffers the Effects of Stress
- High stress levels during forced withdrawal can worsen cravings or emotional instability.
- Social connections help reduce perceived stress, providing calming, regulating influences that support a focus on recovery.
✅ 4. Reinforces Self-Worth and Identity
- Supportive interactions help counter feelings of shame or hopelessness.
- A sense of being cared for enhances self-efficacy—the belief that change is possible.
✅ 5. Improves Compliance with Treatment
- Encouragement from family, counselors, or peer mentors often increases participation in therapeutic activities, group sessions, or medication routines.
✅ 6. Creates a Safety Net Post-Withdrawal
- Social support during forced withdrawal often translates into aftercare support, which is essential for long-term recovery success.
- Examples include transitional housing, sober peer networks, or continued emotional connection to family.
In summary, social support during forced drug withdrawal turns an externally controlled process into a personally meaningful journey, increasing the chances of lasting recovery by reducing stress, boosting motivation, and reinforcing positive identity.
How Addiction Severity Shapes Motivation in Forced Drug Withdrawal
Addiction severity plays a significant role in determining withdrawal motivation during forced or compulsory treatment, such as court-ordered rehab, incarceration-based detox, or mandated inpatient care. The more severe the addiction, the more complex and diminished the individual’s motivation may be—especially in involuntary settings.
🔍 How Addiction Severity Influences Withdrawal Motivation
1. Neurobiological Dependence and Craving
- Severe addiction leads to greater physical dependence and significant changes in dopamine pathways, resulting in:
- Stronger cravings
- More intense withdrawal symptoms
- Higher resistance to abstinence
- These neurobiological shifts make the idea of quitting feel overwhelming, decreasing intrinsic motivation to participate in treatment.
2. Psychological Attachment to Substance Use
- For many, especially those with long-term use, the substance becomes a primary coping mechanism rather than just a habit.
- This emotional reliance weakens commitment to change, particularly when treatment is perceived as punishment or coercion.
3. Impaired Decision-Making and Insight
- Advanced addiction often impairs executive function, including judgment, planning, and impulse control.
- This results in ambivalence, denial, or resistance, particularly when treatment is not self-initiated.
4. Increased Exposure to Trauma or Co-occurring Disorders
- Trauma, PTSD, depression, or anxiety frequently accompany severe addiction.
- If these aren’t addressed alongside detox, forced withdrawal can intensify emotional distress, making treatment feel threatening rather than helpful.
5. Frequent Relapse History
- Many individuals with severe addiction have experienced multiple failed quit attempts.
- This can lead to learned helplessness—a sense that change isn’t possible—which further reduces motivation in compulsory settings.
🔁 The Vicious Cycle
Higher addiction severity → more difficult withdrawal → more stress and fear → lower motivation → greater resistance to treatment.
However, There Is Hope
With the right support systems—such as trauma-informed care, peer mentorship, medication-assisted treatment, and family involvement—individuals with even the most severe addiction can begin to move from external compliance to internal motivation.
Once early withdrawal symptoms are stabilized and emotional safety is established, many can engage more meaningfully in recovery.
How Perceived Stress Shapes Motivation in Compulsory Drug Withdrawal
Perceived stress—how an individual interprets and reacts to stress—directly affects withdrawal motivation during compulsory addiction treatment.
In mandated settings like court-ordered rehab, incarceration, or forced detox, high stress perception can significantly undermine a person’s willingness and ability to engage in recovery.
🔍 How Perceived Stress Influences Withdrawal Motivation
1. High Stress Perception Increases Emotional Resistance
- Involuntary treatment often triggers feelings of:
- Powerlessness or entrapment
- Stigma or punishment
- Fear of painful withdrawal
- If individuals perceive the environment as hostile or unsupportive, they are more likely to resist treatment mentally.
2. Stress Triggers Avoidance Behaviors
- High stress activates survival-mode responses (fight, flight, or freeze), which makes it harder to:
- Trust the staff or the program
- Participate in counseling
- Focus on long-term goals
- This leads to lower motivation and disengagement from treatment.
3. Stress Undermines Self-Efficacy
- Those who doubt their ability to cope with stress often conclude: “I can’t recover.”
- This low self-efficacy is a strong predictor of poor motivation and early dropout.
4. Stress Magnifies Withdrawal Symptoms
- Psychological stress can intensify physical withdrawal symptoms such as:
- Anxiety
- Insomnia
- Cravings
- As detox becomes more unbearable, individuals may mentally check out, even in a supervised setting.
5. Chronic Stress Increases Relapse Thinking
- Overwhelmed individuals may romanticize past drug use as a way to escape current distress.
- This mental loop makes recovery feel less appealing or achievable, especially without internal motivation.
🧠 Key Insight
It’s not just the presence of stress—but how it’s perceived—that determines whether a person leans into recovery or shuts down.
🌱 Protective Role of Positive Stress Perception
When stress is seen as manageable, and individuals feel supported, they are more likely to:
- View treatment as an opportunity
- Commit to abstinence
- Set and pursue recovery goals
Therapeutic approaches such as:
- Coping skills training
- Mindfulness practices
- Cognitive restructuring
…can dramatically reduce harmful stress perception and improve engagement—even in compulsory environments.
Building a Humane Framework for Forced Withdrawal: Practical Strategies to Support Recovery in Compulsory Treatment Settings
Involuntary addiction treatment—whether through incarceration, court-ordered rehab, or mandated inpatient care—can feel harsh and disempowering. But by applying trauma-informed, person-centered practices, we can transform these settings into places that spark healing.
Here are practical strategies to strengthen support, reduce stress, and tailor treatment to addiction severity—cornerstones of a more humane, evidence-based approach to compulsory withdrawal.
🧩 1. Strengthening Support Systems
a. Peer Recovery Specialists
- Assign trained recovery coaches with lived experience.
- Example: A peer mentor meets weekly with individuals during detox to normalize symptoms, build trust, and reduce isolation.
b. Family Reconnection Programs
- Offer structured therapy or virtual visits during detention.
- Example: A weekly “family healing hour” reduces shame and increases external motivation for recovery.
c. Staff Training in Compassion-Focused Communication
- Train all staff—custodial and clinical—in trauma-informed care and motivational interviewing.
- Example: Correctional officers use empathy and curiosity instead of confrontation, improving rapport and compliance.
🧘 2. Reducing Stress in Compulsory Settings
a. Mindfulness and Emotional Regulation Classes
- Offer daily practices like meditation, breathwork, or grounding techniques.
- Example: In-custody rehab units run 15-minute mindfulness breaks to prevent panic during early withdrawal.
b. Environmental Modifications
- Soften institutional spaces with calming visuals, natural light, and noise control.
- Example: Detox units install low lighting, privacy partitions, and soothing murals to reduce sensory overload.
c. Predictable Schedules with Coping-Focused Activities
- Structure daily routines around recovery-focused tasks.
- Example: Clients use “resilience planners” to track triggers, moods, and healthy coping behaviors.
⚖️ 3. Tailoring Treatment to Addiction Severity
a. Severity Assessments at Intake
- Use standardized tools like the ASI to triage levels of care.
- Example: Mild substance use may be addressed with CBT, while more severe cases require medication-assisted treatment.
b. Flexible Withdrawal Protocols
- Adjust detox plans based on drug type, use history, and comorbidities.
- Example: Opioid users receive buprenorphine and close monitoring; stimulant users focus on sleep restoration and nutrition.
c. Integrated Mental Health and Trauma Services
- Treat underlying trauma and psychiatric conditions alongside addiction.
- Example: Individuals receive therapy for PTSD or depression while in withdrawal, helping them stabilize emotionally and physically.
In summary, a more humane approach to forced drug withdrawal isn’t about easing consequences—it’s about delivering targeted, trauma-informed, and evidence-based care that respects human dignity.
By strengthening support, reducing stress, and customizing care to addiction severity, we can turn coercive systems into gateways for real recovery—starting on day one.
Frequently Asked Questions
Here are some common questions:
Question: How can an addict realize that the forced withdrawal regimen is the best option to deal with the addiction?
Answer: An individual with addiction might come to realize that a forced withdrawal regimen is the best option only under specific psychological, social, or situational conditions. But this realization is rarely immediate or voluntary, and it often requires supportive framing, crisis clarity, and post-withdrawal reinforcement. Here’s a breakdown of how this insight might emerge:
🧠 1. Cognitive Realization: Understanding the Urgency
- Clarity through crisis: Many realize withdrawal is necessary when they face an acute crisis—e.g., overdose, job loss, family breakdown, or incarceration. These moments can shake denial.
- Health deterioration: Physical symptoms like liver damage, collapsed veins, or cognitive decline may force the realization that continuing use is unsustainable.
- Education from professionals: Skilled providers can explain how withdrawal is not punishment but a first step toward regaining control, especially if medically supervised.
❤️ 2. Emotional Catalysts: Wanting Change
- Emotional exhaustion: Living in addiction is often deeply tiring. When the pain of use outweighs the fear of withdrawal, people may accept it as necessary.
- Family involvement: When loved ones set healthy boundaries or initiate interventions, it may prompt someone to consider withdrawal.
- Loss of pleasure from substance: Tolerance or anhedonia (lack of pleasure) may make the drug stop “working,” triggering the thought: “Why keep doing this if it doesn’t even help anymore?”
🛠️ 3. Environmental or Structural Pressure
- Involuntary admission or jail: Some people only undergo forced withdrawal when detained or hospitalized. The experience, while difficult, may later be seen as life-saving.
- Court mandates: Drug courts or conditional probation sometimes require detox. After completing it, individuals may feel grateful for the interruption.
- No access to drugs: If availability is disrupted (e.g., moving, arrests, or cost barriers), the body begins detoxing anyway, and that space can allow new insight to emerge.
🌱 4. Post-Acute Insight: Seeing the Benefits
Once someone completes acute withdrawal, they may retrospectively realize its value:
- Improved sleep, emotions, and energy
- More mental clarity and fewer cravings
- First time feeling “normal” in years
- Positive feedback from family or therapists
This post-withdrawal clarity can reinforce the idea that it was the right choice, even if initially resisted.
💬 How to Help Them See It Sooner:
- Normalize the fear: “Withdrawal sounds scary because your body has relied on the drug. But with support, it’s survivable—and temporary.”
- Share peer stories: Real-life testimonies from those who came through withdrawal and found peace can be powerful.
- Focus on short-term goals: Framing withdrawal as just a step (not the whole journey) makes it less overwhelming.
- Use motivational interviewing: Help them explore their values and how addiction is blocking what matters most.
⚠️ Important Note:
Forced withdrawal without support or follow-up care can be dangerous and often leads to relapse. It’s most effective when:
Framed as a choice made under pressure, but still a turning point
Paired with compassionate medical care
Followed by behavioral therapy or medication-assisted treatment (MAT)
Question: How can the family of the addict realize that the forced withdrawal therapies are the best option to manage the addiction?
Answer: For families, realizing that forced withdrawal therapy (i.e., involuntary detox or treatment without the addict’s full cooperation) is the best option often comes with emotional conflict, moral distress, and desperation. It’s not an easy decision. Here’s how they might come to that conclusion—ethically, practically, and emotionally:
🧠 1. Understanding the Nature of Addiction
- Addiction is a brain disease, not just a choice or weakness. Families may begin to accept that rational negotiation often fails when someone is in the grip of severe addiction.
- The person may be unable to act in their own best interest due to impaired judgment, memory, and emotional regulation.
- Realization: “They aren’t choosing this anymore—they’re trapped.”
❤️ 2. Reaching a Breaking Point
- Families often reach this conclusion after:
- Multiple failed attempts at voluntary rehab or outpatient care
- Relapse cycles that put the person or others at serious risk
- Crises, such as overdose, violence, arrest, or medical emergencies
- Realization: “If we wait for them to be ready, they might die.”
🛡️ 3. Recognizing When Harm Reduction Isn’t Enough
- Harm reduction (like using fentanyl test strips or Narcan) is significant—but it doesn’t always address the root addiction.
- Forced withdrawal becomes a last resort when:
- The person is a danger to themselves or others
- Their use is so severe that waiting is enabling
- All other options have been exhausted
🗣️ 4. Guidance from Professionals
- Health providers, therapists, and addiction counselors may explain:
- The medical safety of supervised withdrawal
- Detox is a necessary first step, not the whole solution
- The legal or ethical pathways for family-initiated care (e.g., court-mandated detox, Marchman Act, civil commitment)
- Realization: “This isn’t about control—it’s about saving a life while we still can.”
📊 5. Seeing Long-Term Benefits from Others
- Support groups like Al-Anon, Nar-Anon, or parent networks often share success stories where forced withdrawal led to:
- First-time clarity
- Willingness to try treatment
- Restored relationships after detox
- Realization: “Other families went through this—and it worked. We’re not alone.”
🧩 6. Shifting the Family Role: From Enabling to Boundaries
- Families often enable unintentionally: giving money, covering up, or bailing out.
- Choosing forced withdrawal may reflect a shift to tough love:
- Setting limits without cutting off love
- Refusing to allow the addiction to dominate the household
- Committing to long-term support after detox
⚠️ 7. What Families Must Consider Before Choosing Forced Withdrawal
- It should be medically supervised, not done cold turkey at home.
- There should be a plan for follow-up care (e.g., inpatient rehab, MAT, counseling).
- Forced withdrawal isn’t a cure—it’s a door opener.
- Family must be prepared for initial resistance, anger, or relapse.
✅ Final Realization Families May Come To:
“We can’t wait for rock bottom. We have to interrupt the addiction cycle, even if they don’t want us to. It might hurt short-term, but it gives them a real shot at recovery.”
Question: How can the government court use forced withdrawal to help the addict manage his addiction?
Answer: Governments and courts can use forced withdrawal (involuntary detoxification) as a legal and clinical intervention to interrupt severe addiction and move individuals into treatment they would not otherwise choose. While controversial, this approach is sometimes the only viable option when addiction creates danger to self or others.
Here’s how government courts can ethically and effectively use forced withdrawal to help someone manage their addiction:
⚖️ 1. Legal Tools Courts Use to Enforce Withdrawal and Treatment
🏛️ Civil Commitment Laws (e.g., Marchman Act, Casey’s Law)
- These allow family members or professionals to petition the court to mandate assessment, detox, and treatment.
- Criteria often include:
- Loss of control over substance use
- Refusal of voluntary treatment
- Serious risk to self, children, or community
- Once approved, the court can order:
- Involuntary medical detox
- Residential or outpatient treatment for 30–90 days or longer
👩⚖️ Drug Courts
- Instead of jail time, courts offer structured treatment plans that may begin with detox or withdrawal management.
- Participants are monitored through:
- Mandatory treatment attendance
- Drug testing
- Case management
- Withdrawal may occur under medical supervision at entry, then lead to long-term care.
🚓 Criminal Court Diversion (Pretrial or Post-Conviction)
- People charged with non-violent drug offenses may be diverted into court-mandated detox and treatment instead of prison.
- This is often combined with probation or suspended sentencing.
- Real goal: Break the cycle of addiction and reoffending.
🧠 2. How Forced Withdrawal Helps Addicts via the Court System
| Protects children, partners, or the community from harm caused by untreated addiction | Explanation |
|---|---|
| Safety-first intervention | Immediate removal from substance access in medically supervised detox setting |
| Cognitive clarity post-withdrawal | Removes fog of intoxication, allowing rational thought and better treatment buy-in |
| Legal leverage | Court pressure creates accountability—especially for those with impaired insight |
| Bridge to longer treatment | Detox opens the door to longer rehab, MAT, therapy, housing, or vocational help. |
| Family protection | Protects children, partners, or community from harm caused by untreated addiction |
💡 3. Key Elements of an Effective Court-Based Forced Withdrawal Program
- Medical Supervision
- No jailhouse cold-turkey detox
- Must be safe, humane, trauma-informed
- Integrated Treatment Continuum
- Detox is step 1—not the end
- Court orders should include referrals to:
- Residential/inpatient rehab
- Outpatient counseling
- Medication-Assisted Treatment (e.g., methadone, buprenorphine)
- Peer support programs
- Wraparound Services
- Housing, job training, mental health care
- Helps address why the person was used in the first place
- Judicial Monitoring
- Ongoing check-ins with judges and case managers
- Positive reinforcement (graduation ceremonies, reduced probation)
⚠️ 4. Risks & Ethical Considerations Courts Must Navigate
| Court orders must consist of aftercare and MAT, not just withdrawal | How to Address It |
|---|---|
| Violation of autonomy | Use only when all voluntary options fail and danger is clear |
| Trauma from coercion | Use trauma-informed staff and include mental health support |
| Risk of relapse post-detox | Court orders must include aftercare and MAT, not just withdrawal |
| Racial or economic bias | Ensure fair access and non-discriminatory enforcement practices |
✅ Conclusion: The Court’s Role in Compassionate, Structured Intervention
Forced withdrawal, when done through the court with medical care and treatment planning, can save lives. It’s not a punishment—it’s a lifeline. The goal is not just to stop drug use temporarily but to restore long-term capacity for choice, dignity, and recovery.
Conclusion
The combined impact of social support, addiction severity, and stress perception shapes withdrawal motivation during forced treatment. Addressing these factors through tailored care, emotional support, and stress-reduction strategies can transform mandatory therapy into a more humane and effective recovery experience. Prioritizing person-centered approaches ensures that even in involuntary settings, individuals are met with dignity, compassion, and the tools needed for lasting change.
Video: Is Forced Detox REALLY the Best Option for Severe Addiction?